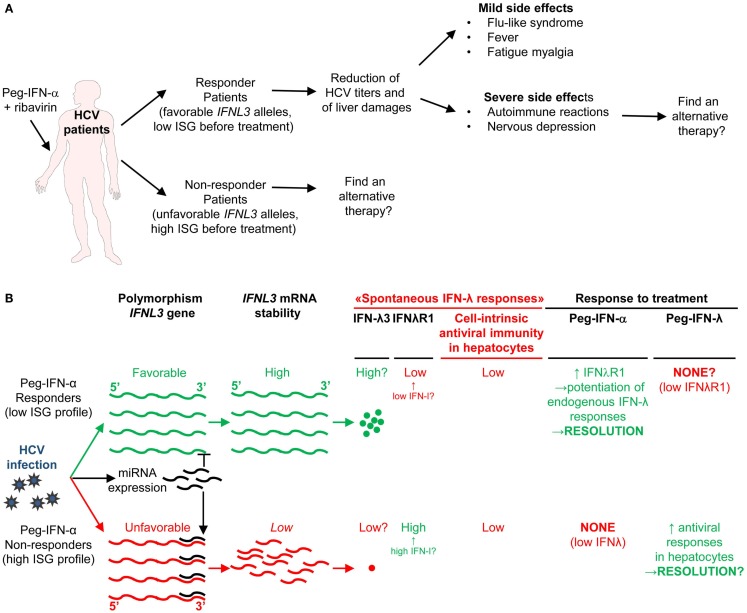
Figure 7.
A novel hypothetical model attempting to explain the respective roles of IFN-I and IFN-III in HCV infection. (A) Classification of patients suffering from chronic HCV infection and treated with PEG-IFN-α in non-responders and responders, and identification of IFNL3 (IL28B) gene polymorphisms as the best predictors for treatment response. The side-effects induced by PEG-IFN-α treatment are also listed since they can severely affect the patient’s quality of life and lead to treatment failure due lack of compliance or suicide. Hence, new approaches are needed to promote beneficial over deleterious effects of IFN-I administration in chronic HCV infection. (B) Proposal of a new hypothesis explaining the relationships between endogenous ISG levels in patients prior to treatment, IFNL3 gene polymorphism, endogenous expression of IFN-I, IFN-λ, and IFNλR1, and responsiveness to IFN-I administration. Efficient control of HCV infection may depend on hepatocyte response to IFN-λ rather than IFN-α. Upon HCV infection, the virus induces the expression of host miRNA able to bind the 3′ UTR of IFNL3 mRNA to promote their degradation. The favorable IFNL3 allele associated with responsiveness to PEG-IFN-α treatment may allow endogenous expression of sufficient levels of IFNL3 for efficient induction of cell-intrinsic anti-viral defenses in hepatocytes. This process is, however, hampered by the limited expression of the receptor for this cytokine (IFNλR1) in these patients. PEG-IFN-α treatment might promote resolution of the infection by inducing IFNλR1 in these patients, potentiating their response to their endogenous production of IFNL3. In the patients that do not respond to PEG-IFN-α treatment, endogenous levels of IFNL3 are insufficient for efficient induction of cell-intrinsic anti-viral defenses in hepatocytes, due to the degradation of the corresponding mRNA in infected hepatocytes. In these patient’s hepatocytes, however, IFNλR1 is already expressed to high levels prior to treatment due to their high endogenous IFN-I responses. Administration of exogenous IFN-λ might cure these patients. See main text for further details.