Abstract
Introduction
Autologous fat transplantation has attracted great interest in breast augmentation for cosmetic purpose. In the present study, we reported our experience in fat grafting in breast in 105 cases, and some detailed procedure concerning efficacy and safety of grafting was evaluated.
Methods
Fat was harvested using 20-mL syringe attached to a 3-hole blunt cannula in a diameter not beyond 3 mm. After washing with cool normal saline to remove blood, the fat was managed with open method using cotton towel as a platform for concentration fat tissue and separating them from fluids, oil, and debris. A 14-gauge, 1-hole blunt cannula was used to place the fat through 3-mm incision on inframammary fold. The fat was infiltrated into the breast from deep to superficial subcutaneous plane.
Results
Between July 2002 and August 2010, 105 patients have undergone this procedure. The age distribution of the patients ranged from 18 to 45 years, with a mean of 31.3 years. Grafted fat volume has ranged from 120 to 250 mL (average, 205 mL) per breast per session. All women had a significant improvement in their breast size and shape postoperatively, and the breasts were soft and natural in appearance.
Conclusions
Liposuction and autologous fat transplantation is a suitable approach for augmentation mammaplasty.
Key Words: autologous fat injections, breast augmentation
The number of patients choosing to receive augmented mammaplasty is increasing steadily with rapid economic development in China. Although implantation of breast prosthesis remains the most popular cosmetic breast surgery, a large number of patients completely refused this operation because of their nonacceptance of having artificial materials in body. Concerning adverse effects of postoperation residual scars, contracture deformity, as well as less natural shape and feel in breast augmentation, some other patients turned to breast augmentation with injectable materials. It was estimated that Amazing Gel (polyacrylamide hydrogel) injection, which induced severe complications including breast tissue necrosis and chronic pectoralis inflammation evoked by material infiltration, have been performed in more than 500,000 people. Clinical application use of Amazing Gel was prohibited by Chinese government in April 2006.1
In recent years, autologous fat grafting for breast augmentation showed great outcomes in cosmetic enhancement in size, shape, and texture of breast. Zheng et al,2 Illouz and Sterodimas,3 Coleman and Saboeiro,4 and other authors all reported autologous fat graft as an effective method either for breast reconstruction or cosmetic breast augmentation. Besides, as the traditional aesthetic conception of Chinese tends to mingle with the Western, people admire a figure both plump and slender. Moreover, autologous fat grafting combines liposuction and breast augmentation, so it becomes more and more popular.
This article seeks to present our 8-year clinical experience with autologous fat transplantation for breast augmentation and describe our harvesting and fat processing and transfer techniques, along with review of clinical results of our patients.
PATIENTS AND METHODS
A total of 105 female patients who underwent autologous fat grafting in breast from July 2002 to August 2010 were included in this retrospective study. The age distribution of the patients at the time of the operation ranged from 18 to 45 years, with a mean of 31.3 years. Indications for fat grafting in these patients included micromastia (101 patients), tuberous breast deformity (2 patients), and severe asymmetry (2 patients). All the patients underwent major or mild body contouring at the same time. The study protocol complied with the Declaration of Helsinki and all patients were provided written informed consent. Before operation, breast magnetic resonance imaging (MRI) or x-ray mammography was performed.
SURGICAL TECHNIQUE
Areas for liposuction and breast lipoinjection were marked with the patients in the upright position. Liposuction area included abdomen, flanks, trochanteric region, inner thigh, medial aspect of knees, and upper arms, respectively, depending on the patient’s natural fat distribution. Under general anesthesia, the liposuction area was infiltrated with tumescent solution (20 mL of 2% lidocaine with epinephrine, 1:100,000 per liter of normal saline) following the principles described by Coleman. The fat is aspirated using a 3-holed blunt cannula (3 mm in the inner diameter) connected to a 20-mL syringe. All aspirated fat was collected together within a sterile container with a single-layered cotton gauze in it (Fig. 1). The aspirate was washed 3 to 4 times with 4°C cool normal saline and condensed with dry cotton pad to allow saline, oil, and blood cells to be absorbed. Through the previously mentioned process, 50% to 70% of the liposuction was successfully acquired which contains mainly pure lipoparticle for lipoinjection (Fig. 2).
FIGURE 1.

The fat is collected in a sterile cup dressed with a gauze (left). The aspirate is washed with 4 °C cool normal solution one to two times (right).
FIGURE 2.
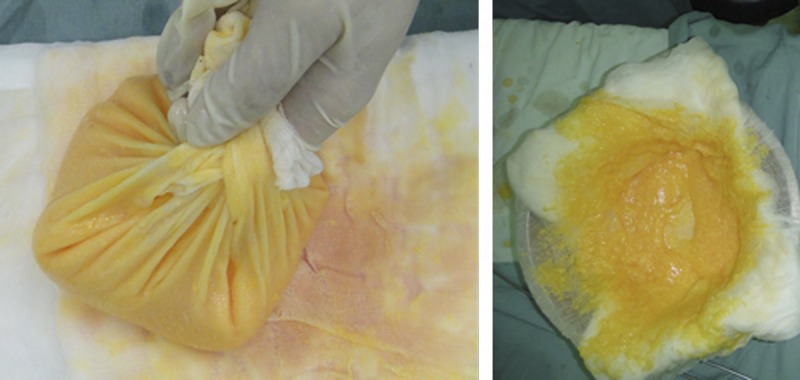
The washed aspirate packed in the gauze is left to dry on a cotton pad (left), which is changed with a dry one every 5 min, until it reaches a semisolid state (right).
Before lipoinjection, a tiny incision was made at the lateral region of the inframammary fold. Each breast was infiltrated with tumescent solution in the retroglandular and subcutaneous layer. A 14-gauge, 1-hole blunt cannula was connected to a 20-mL Luer-Lok syringe filled with the processed fat (Fig. 3, left). During the injection, the fat was dispersed evenly into the breast tissue, whereas the cannula was withdrawn in conjunction with slow and steady pressure on the plunger, leaving behind the form of fine noodle-like adipose tissue (Fig. 3, middle). The fat is placed in multiplane from deep to subcutaneous tissue (Fig. 3, right). Approximately two thirds of the collected fat was injected into the retroglandular and intraglandular space layer by layer. The remaining tissue was injected in the subcutaneous space. After injection, the injected area was carefully molded and reshaped to adapt the outline of the desired breast (Fig. 4).
FIGURE 3.

The fat was injected in small quantities through stab incision made in the lateral region of inframammary fold (left), in the form of fine cylinders resembling noodle (middle). The fat was placed multidirectionally from deep to superficial subcutaneous plane (right).
FIGURE 4.

Fat tissue is carefully molded and reshaped to obtain a smooth and regular surface.
All patients were discharged from the surgery center after recovery from anesthesia and were informed with activity limitation of 3 to 7 days. Local cold compresses were carried out as needed to reduce and prevent secondary injury resulting from edema and inflammation. The patient was instructed not to compress or massage the breasts within the duration of 3 months after surgery.
The clinical outcomes were evaluated according to the methods described by Zheng et al2 at 6 months after the last fat grafting. In brief, the results were graded based on the improvement of breast augmentation and correction of contour defect. Fifteen patients who received a second or third fat grafting were examined by MRI of breast to evaluate survival of injected fat as well as potential lump formation. Clinical data relating to any complications, especially the development of breast lump that can be palpated, were collected during follow-ups in all patients.
RESULTS
Among all patients in the present study, 80 patients received 1 session of fat grafting, 20 patients received 2 sessions of fat grafting, and 5 patients received 3 session of fat grafting. An average of 205 mL of fat was transplanted at each session per breast (range, 120–250 mL). The average clinical follow-up was 18 months (range, 6–72 months). Of a total of 105 patients, 47 (44.8%) were evaluated as significantly improved (Figs. 5–7), 41 (39.0%) as improved, and 17 (16.2%) as not improved. There was no evidence of newly occurring oil cyst, fat necrosis, or breast masses seen in the postoperative MRI scan. Two patients developed benign-appearing calcifications easily distinguishable from cancer. Three patients developed small nodules that revealed fat necrosis on aspiration (Figs. 8 and 9).
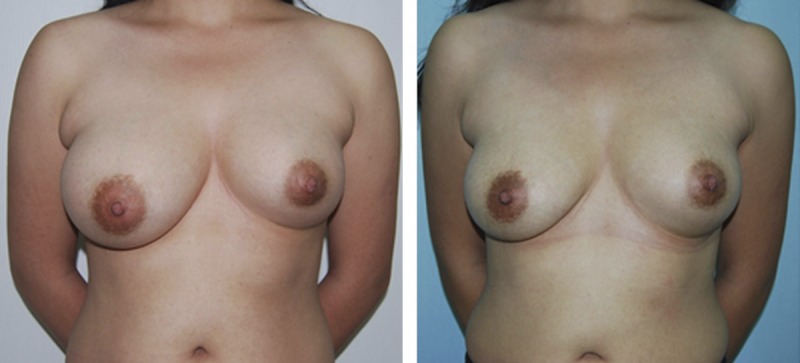
FIGURE 5.
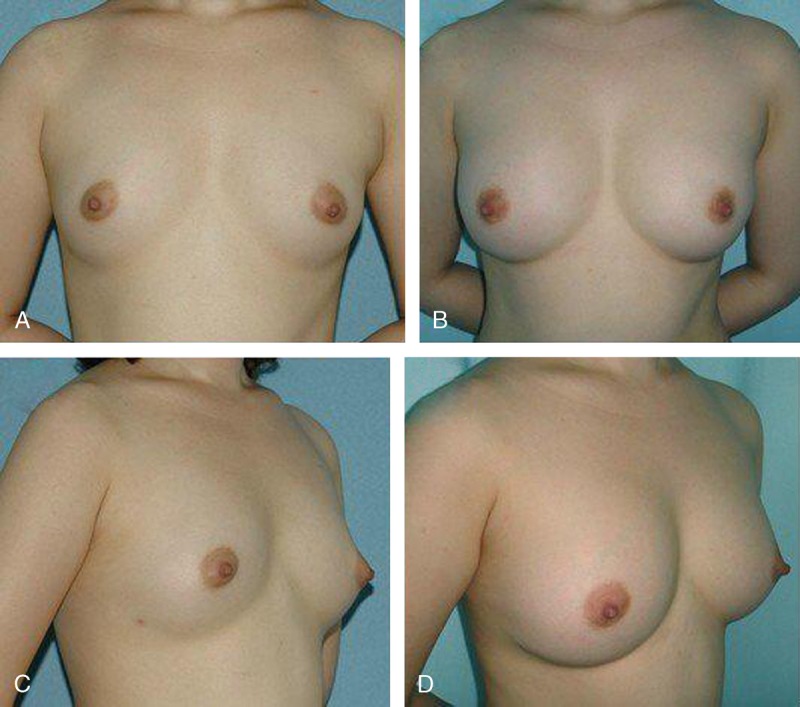
A and C, Preoperative views of a 21-year-old girl requesting breast augmentation. B and D, Postoperative views 8 months after breast augmentation with 220 ml fat in each breast.
FIGURE 7.
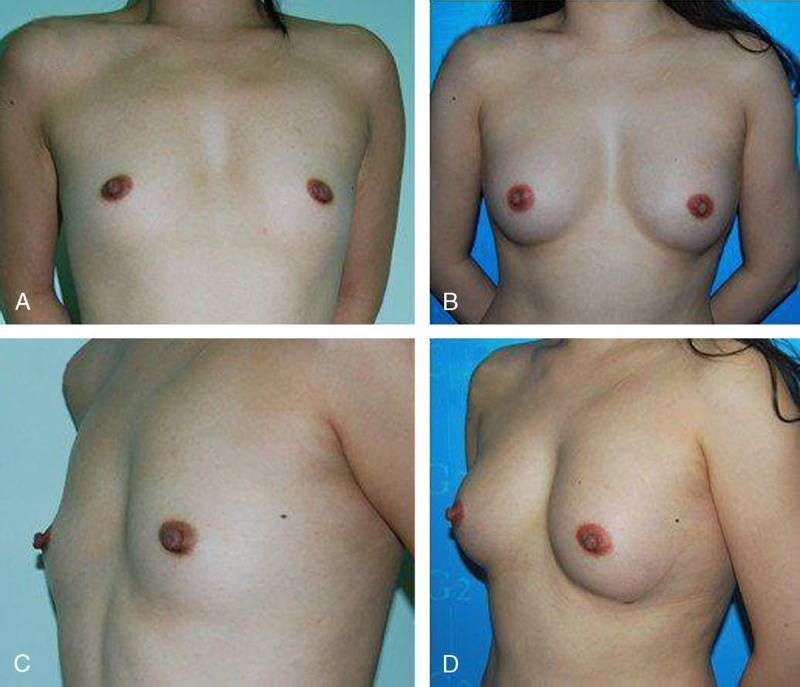
A and C, Preoperative views of a 30-year-old woman with a severe breast hypotrophy. B and D, Postoperative view after three sessions of breast lipo?lling six months after the last procedure (injections of 190 ml, 220 ml and 210 ml, respectively).
FIGURE 8.

A and C, Preoperative views of a 29-year-old woman with bilateral tuberous breast deformity. B and D, Postoperative view after three sessions of breast lipo?lling six months after the last procedure (injections of 210 ml, 250 ml and 280 ml, respectively).
FIGURE 9.
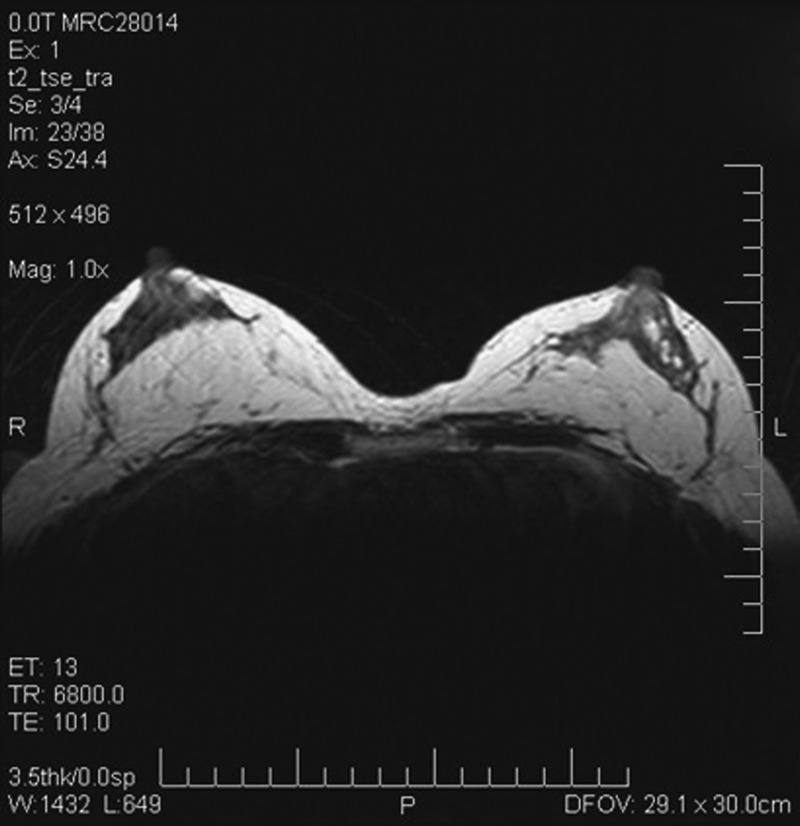
Magnetic resonance imaging (MRI) shows that injected fat survives very well in retroglandular and subcutaneous plane. There are no cysts, masses, or fat necrosis.
FIGURE 6.
Preoperative views of a 21-year-old woman with marked breast asymmetry (right breast with hyperplasia and left beast with hypoplasia). Seven months after right breast reduction by liposuction of 200 ml fat and left breast augmentation by injection of 200 ml fat from the abdomen (right).
DISCUSSION
In the present study, we found that outcomes for breast augmentation correlated well with the total amount of injected fat. If the volume of the fat transplanted into the breast is less than 150 mL on each side, the result of augmentation is less obvious. Among all patients treated in this study, no cosmetic improvement was noticed in 17 (16.2%) thin patients who had been injected less than 150 mL of fat because no more adipose deposit was suitable for harvesting. Therefore, in our opinion, autologous fat transfer for breast augmentation is not suitable for thin women who have insufficient fat deposit. Significant cosmetic improvement was achieved through 2 or 3 sessions of fat grafting in patients with adequate adipose deposit even if their breasts are very small (Fig. 7). Interestingly, we found out that when patients received a second fat graft, the cosmetic result would be enhanced significantly. This may be attributed to the increased vascularization that resulted from survival of previously transplanted fat.
Although various preparation techniques have been suggested for improving survival of fat grafts,5–7 including centrifugation,8–12 simple decantation,13 vigorous washing,14 no washing at all,15 and dense-cloth fat concentration,16 there is still controversy about their long-term results. Coleman8 stressed the importance of removing nonviable fat aspirate components such as oil, blood, and lidocaine by centrifugation. He reports high physician and patient satisfaction from his “structural fat grafting” technique. This method has gained widespread clinical application and has become fundamental to many techniques described in numerous reports. However, centrifugation was challenged by Rohrich et al,17 who found that fat survival rate from centrifugation showed no better than that of filtration. Ramon et al18 compared samples prepared either via centrifugation or cotton towel drying in a nude mouse model, and observed no differences in fat weight or volume, yet the towel separated samples exhibited decreased fibrosis on histologic analysis.
Khater et al,19 in a clinical and experimental study, presented their experience with the following 2 different techniques of fat processing: centrifugation and serum washing. The authors concluded that in noncentrifuged adipose tissue, more active preadipocytes were maintained, which could possibly lead to enhanced survival of injected fat.
In a clinical trial, Botti et al demonstrated that there was no significant difference of survival between washed and centrifuged fat. They, thus, went back to use the simple filtered fat after some years of using centrifuged fat.20
The processing procedure we used to prepare fat for injection is similar to the method described by Kuran and Tumerdem.21 It is simple, safe, and effective. The aspirate was cleansed of blood, oil, and lidocaine by filtering after the gentle washing with cool 0.9% normal saline (Fig. 1). According to the study by Condé-Green et al,13 the aspirate processed by washing not only maintained considerable number of adipocyte with good integrity deprived of blood cell contaminants but also preserved a great number of endothelial and mesenchymal stem cells, which are believed to contribute to increased neoangiogenesis, reduced apoptosis, and promotion of adipocyte differentiation.22 After filtering, there is still a lot of water and oil in the fat. Del Vecchio and Rohrich find that after sedimentation and discarding unwanted crystalloid, there is still 20% to 30% of additional crystalloid in the fat. Ignoring the step of condensation reduces long-term volume maintenance, there is a “percentage yield” by 20% to 30% before the procedure is finished than condensation method.23 Thus, through the process of gauze filtering, cool saline washing, and cotton pad concentrating, the desired pure semisolid fat was achieved for further injection (Fig. 2).
Time efficiency (optimization) versus effectiveness of technique (maximization) is a critical workflow concept in fat transplantation.23 The method we used is associated with a Chinese traditional philosophy—the “Golden mean,” which means we must achieve the best balance between minimal injury and less ischemic time of the fat before it is transplanted into the breast. It is reported that most of adipocytes in aspirate preserved at room temperature beyond 4°C experienced significant damage. The lipotransfer should be performed as quickly as possible after aspiration.24
Using smaller syringes (10 mL) with minimal negative pressure is considered as a standardized technique for harvesting of fat.25,26 However, this technique is time consuming for collecting large volume of fat for grafting. Therefore, a 20-mL syringe was used in the present study for fat harvesting in an effort to reduce the time consumed in the whole surgery.
Grafted fat that is too large in volume for injection may suffer central necrosis in vivo because of a lack of both adequate nutrition diffusion and neoangiogenesis. Minimizing the amount of fat grafted with each pass of cannula during injection will maximize the surface area of contact between the grafted fat and recipient tissue. Coleman’s technique of fat grafting has been popularized and known to many surgeons, which emphasizes on atraumatic method of fat harvesting, proper centrifugation, and miniscule injection aimed at maximal contact between transplanted fat and recipient tissue, but it took approximately 3 hours to place 250 mL into an individual breast.4 The negative effects of extracorporeal ischemic time potentially outweigh the benefit of the technique of minimal trauma to fat for injection. To enhance the efficiency of fat injection while reducing the ischemic time, we used a 20-mL Luer-Lok syringe for fat injection in which injection of 20 mL of fat contained in 1 syringe can be completely fulfilled in 1 minute.
CONCLUSIONS
Remarkable, long-lasting, and natural improvements of breast size and shape are achieved with autologous fat grafting in most patients in the present study. The more details you pay during the process of the procedure, the better clinical outcomes you will get. The details in the duration of breast augmentation including low pressure but efficient technique of harvesting of fat, condensation with cotton pad after gentle washing and filtering, multilayered deposition of fat, and decrease of ischemic time are discussed in the study.
Footnotes
Conflicts of interest and sources of funding: none declared.
REFERENCES
- 1. Cheng MH, Huang JJ. Augmentation mammaplasty in Asian women. Semin Plast Surg. 2009; 23: 48– 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zheng DN, Li QF, Lei H, et al. Autologous fat grafting to the breast for cosmetic enhancement: experience in 66 patients with long-term follow up. J Plast Reconstr Aesthet Surg. 2008; 61: 792– 798. [DOI] [PubMed] [Google Scholar]
- 3. Illouz YG, Sterodimas A. Autologous fat transplantation to the breast: a personal technique with 25 years of experience. Aesthetic Plast Surg. 2009; 33: 706– 715. [DOI] [PubMed] [Google Scholar]
- 4. Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007; 119: 775– 785. [DOI] [PubMed] [Google Scholar]
- 5. Jackson IT, Simman R, Tholen R, et al. A successful long-term method of fat grafting: recontouring of a large subcutaneous postradiation thigh defect with autologous fat transplantation. Aesthetic Plast Surg. 2001; 25: 165– 169. [DOI] [PubMed] [Google Scholar]
- 6. Toledo LS, Mauad R. Fat injection: a 20-year revision. Clin Plast Surg. 2006; 33: 47– 53. [DOI] [PubMed] [Google Scholar]
- 7. Smith P, Adams WP, Jr, Lipschitz AH, et al. Autologous human fat grafting: effect of harvesting and preparation techniques on adipocyte graft survival. Plast Reconstr Surg. 2006; 117: 1836– 1844. [DOI] [PubMed] [Google Scholar]
- 8. Coleman SR. Structural fat grafts: the ideal filler? Clin Plast Surg. 2001; 28: 111– 119. [PubMed] [Google Scholar]
- 9. Coleman SR. Long-term survival of fat transplants: controlled demonstrations. Aesthetic Plast Surg. 1995; 19: 421– 425. [DOI] [PubMed] [Google Scholar]
- 10. Coleman SR. Facial recontouring with lipostructure. Clin Plast Surg. 1997; 24: 347– 367. [PubMed] [Google Scholar]
- 11. Fulton JE, Parastouk N. Fat grafting. Dermatol Clin. 2001; 19: 523– 530. [DOI] [PubMed] [Google Scholar]
- 12. Kononas TC, Bucky LP, Hurley C, et al. The fate of suctioned and surgically removed fat after reimplantation for soft-tissue augmentation: a volumetric and histologic study in the rabbit. Plast Reconstr Surg. 1993; 91: 763– 768. [DOI] [PubMed] [Google Scholar]
- 13. Condé-Green A, de Amorim NF, Pitanguy I. Influence of decantation, washing and centrifugation on adipocyte and mesenchymal stem cell content of aspirated adipose tissue: a comparative study. J Plast Reconstr Aesthet Surg. 2010; 63: 1375– 1381. [DOI] [PubMed] [Google Scholar]
- 14. Asken S. Autologous fat transplantation: micro and macro techniques. Am J Cosmet Surg. 1987; 4: 111– 121. [Google Scholar]
- 15. Pinski KS, Roengik HH., Jr Autologous fat transplantation: long-term follow-up. J Dermatol Surg Oncol. 1992; 18: 179– 184. [DOI] [PubMed] [Google Scholar]
- 16. Carraway JH, Mellow CG. Syringe aspiration and fat concentration: a simple technique of fat autologous fat injection. Ann Plast Surg. 1990; 24: 293– 296; discussion 297 [DOI] [PubMed] [Google Scholar]
- 17. Rohrich RJ, Sorokin ES, Brown SA. In search of improved fat transfer viability: a quantitative analysis of the role of centrifugation and harvest site. Plast Reconstr Surg. 2004; 113: 391– 395; discussion 396–397. [DOI] [PubMed] [Google Scholar]
- 18. Ramon Y, Shoshani O, Peled IJ, et al. Enhancing the take of injected adipose tissue by a simple method for concentrating fat cells. Plast Reconstr Surg. 2005; 115: 197– 201. [PubMed] [Google Scholar]
- 19. Khater R, Atanassova P, Anastassov Y, et al. Clinical and experimental study of autologous fat grafting after processing by centrifugation and serum lavage. Aesthetic Plast Surg. 2009; 33: 37– 43. [DOI] [PubMed] [Google Scholar]
- 20. Botti G, Pascali M, Botti C, et al. A clinical trial in facial fat grafting: filtered and washed versus centrifuged fat. Plast Reconstr Surg. 2011; 126: 2464– 2473. [DOI] [PubMed] [Google Scholar]
- 21. Kuran I, Tumerdem B. A new simple method used to prepare fat for injection. Aesthetic Plast Surg. 2005; 29: 18– 22. [DOI] [PubMed] [Google Scholar]
- 22. Kamakura T, Ito K. Autologous cell-enriched fat grafting for breast augmentation. Aesthetic Plast Surg. 2011; 35: 1022– 1030. [DOI] [PubMed] [Google Scholar]
- 23. Del Vecchio D, Rohrich RJ. A classification of clinical fat grafting: different problems, different solutions. Plast Reconstr Surg. 2012; 130: 511– 522. [DOI] [PubMed] [Google Scholar]
- 24. Matsumoto D, Shiqeura T, Sato K, et al. Influences of preservation at various temperatures on liposuction aspirates. Plast Reconstr Surg. 2007; 120: 1510– 1517. [DOI] [PubMed] [Google Scholar]
- 25. Crawford JL, Hubbard BA, Colbert SH, et al. Fine tuning lipoaspirate viability for fat grafting. Plast Reconstr Surg. 2010; 126: 1342– 1348. [DOI] [PubMed] [Google Scholar]
- 26. Pu LLQ, Cui X, Fink BF, et al. The viability of fatty tissues within adipose aspirates after conventional liposuction: a comprehensive study. Ann Plast Surg. 2005; 54: 288– 292. [PubMed] [Google Scholar]


