Abstract
Background
Socioeconomic inequalities in mortality are one of the greatest challenges for health policy in all European countries, but the potential for reducing these inequalities is unclear. We therefore quantified the impact of equalizing the distribution of six risk factors for mortality: smoking, overweight, lack of physical exercise, lack of social participation, low income, and economic inactivity.
Methods
We collected and harmonized data on mortality and risk factors by educational level for 21 European populations in the early 2000s. The impact of the risk factors on mortality in each educational group was determined using Population Attributable Fractions. We estimated the impact on inequalities in mortality of two scenarios: a theoretical upward levelling scenario in which inequalities in the risk factor were completely eliminated, and a more realistic best practice scenario, in which inequalities in the risk factor were reduced to those seen in the country with the smallest inequalities for that risk factor.
Findings
In general, upward levelling of inequalities in smoking, low income and economic inactivity hold the greatest potential for reducing inequalities in mortality. While the importance of low income is similar across Europe, smoking is more important in the North and East, and overweight in the South. On the basis of best practice scenarios the potential for reducing inequalities in mortality is often smaller, but still substantial in many countries for smoking and physical inactivity.
Interpretation
Theoretically, there is a great potential for reducing inequalities in mortality in most European countries, for example by equity-oriented tobacco control policies, income redistribution and employment policies. Although it is necessary to achieve substantial degrees of upward levelling to make a notable difference for inequalities in mortality, the existence of best practice countries with more favourable distributions for some of these risk factors suggests that this is feasible.
Introduction
Inequalities in health between socioeconomic groups are increasingly recognized as one of the main challenges for health policy [1]. Studies comparing different European countries have shown that health inequalities are substantial almost everywhere, but that there are important variations between countries in the magnitude of health inequalities, suggesting great scope for reduction [2], [3].
Explanatory research has identified many factors contributing to inequalities in health. These include behavioural risk factors such as tobacco smoking, excessive alcohol consumption, and physical inactivity, but more ‘upstream’ social and economic risk factors such as social isolation, low income, unemployment, and occupational risks have been shown to contribute as well [4]–[8].
On the basis of these explanatory findings, policy proposals have been developed, both at the national level [9]–[14] and internationally (1). However, it is unclear what the potential for reducing health inequalities is in quantitative terms, and most of these proposals have not been based on a formal analysis of what the most important determinants of health inequalities are.
We have therefore set out to quantify the potential for reducing inequalities in mortality by tackling each of a number of key determinants. We have done this by estimating the reduction of educational inequalities in mortality that would be obtained, if European populations would succeed in reducing or even eliminating inequalities in important risk factors through effective policy interventions.
The first group of determinants is a set of three ‘downstream’ risk factors: smoking, overweight, and physical inactivity. These risk factors are relatively easy to measure and have a reasonably well-documented causal effect on mortality [15]–[18]. It has already been shown that these risk factors have a higher prevalence in lower socioeconomic groups in many European countries [19]–[23].
Because an emphasis on behavioural risk factors may distract from the necessary action on ‘upstream’ risk factors [24]–[26], we have also studied three social and economic risk factors: lack of social participation, low income, and economic inactivity. Lack of social participation, low income and economic inactivity (through temporary unemployment or more permanent detachment from the labour market) probably all increase mortality [27]–[34], and their prevalence is higher in lower socioeconomic groups [35]–[37].
The main purpose of this paper is to show to what extent inequalities in mortality can potentially be reduced by tackling each of these determinants, and to provide guidance on priorities for health policy in different European countries. As will be demonstrated, the potential for reducing inequalities in mortality is substantial, but priorities for action should not be the same everywhere.
Data and Methods
Data
Data on mortality by sex, age, cause of death and education were obtained from mortality registries for all European populations for which good quality data are available. They cover people aged 30–79 in 21 European populations in the period ca. 2000 – ca. 2005 and are mainly based on longitudinal or linked cross-sectional studies representing whole nations. These populations are those of Finland, Sweden, Norway and Denmark in the North; Scotland, England and Wales, Netherlands, Belgium, France, Switzerland, and Austria in the West; Spain (Barcelona, Basque Country and Madrid) and Italy (Turin and Tuscany) in the South, and Czech Republic, Poland, Hungary, Lithuania and Estonia in the Centre/East. Our main sources of mortality data are presented as supporting information (Table S1 in File S1).
We have focused on educational inequalities in mortality (instead of, e.g., occupational inequalities in mortality) because data on educational attainment are available for both men and women in all European populations under study. In addition, education is the most stable measure of socioeconomic position because it is normally completed early in adulthood, which avoids reverse causation problems (i.e., health problems at older ages cannot change a person's level of education) [38]. Educational level was harmonized across countries according to the International Standard Classification of Education (ISCED) and split into three internationally comparable categories. These correspond to less than secondary education (low), complete secondary education (mid), and tertiary education (high).
Risk factor prevalence data by sex, age, and level of education were collected for the early 2000s, mainly from national health surveys. Smoking was measured in three categories (‘never smokers’, ‘former smokers’, ‘current smokers’), overweight in three (BMI <25, 25–30, 30+), leisure-time physical activity in two (‘active’: less than once a week and ‘sedentary’: once a week or more), social participation in two (‘participation in at least one voluntary organization’, ‘no participation’), income in four (equivalent net household income quartiles), and economic activity in two (‘economically active’, ‘economically inactive’). Temporary unemployed were classified with the inactive in Norway, Sweden, Switzerland, and Madrid, and with the active in all other populations.
Relative risks for the impact of smoking, overweight, physical inactivity and lack of social participation on mortality were collected from large reviews and meta-analyses [18], [29], [39], [40] making sure that the estimates of relative risk were adjusted for the effect of relevant confounders. For income and economic inactivity no authoritative estimates were available in the literature. We therefore calculated relative risks for lower income quartiles using a Finnish register-based follow-up study of three million men and women, with adjustment for age, household structure, spouse's economic activity, occupational class, education and own economic activity [41]. We calculated relative risks for economic inactivity from our own mortality data, adjusting for age and educational attainment, and estimating a separate relative risk for countries where unemployed were classified with the inactive. A full account of all data sources can be found elsewhere [42]. All data used in the calculations and their definitions are presented as supporting information. These include characteristics of the mortality data (Table S1 in File S1), rate ratios for the association between education and all-cause mortality (Table S2 in File S1), relative risks for the impact of risk factors on all-cause mortality (Table S3 in File S1), sources of prevalences (Table S4 in File S1), and the prevalences of smoking (Table S5 in File S1), overweight (Table S6 in File S1), physical inactivity (Table S7 in File S1), social participation (Table S8 in File S1), income (Table S9 in File S1), economic inactivity (Table S10 in File S1). Furthermore, analyses of the potential reduction (in %) of relative educational inequalities in all-cause mortality between low and high educated, by risk factor, country and sex are given in Table S11 in File S1 (upward levelling scenario) and Table S12 in File S1 (best practice scenario).
Written informed consent of the usage of mortality and survey data was given by the relevant administrative units in the respective countries.
Methods
We quantified educational inequalities in mortality by calculating rate ratios (RR) and rate differences (RD) from age-adjusted mortality rates using high education as a reference category. In this paper we only present scenario changes in RRs and RDs comparing the lowest with the highest educational group. Results for all educational groups can be found elsewhere [42].
The estimates of the potential reduction of inequalities in mortality are based on two different types of counterfactual scenarios. The first is an upward levelling scenario which assumes that the exposure to a risk factor would be reduced to the level currently seen among the highest educated within each country. This will identify a possible upper limit to what can be achieved in each country. In the uncommon case that the lower educated are less frequently exposed to risk factors than the higher educated, which mainly applies to female smokers in the South of Europe, we assume that the potential reduction of inequalities in mortality is zero.
The second type is a best practice scenario, in which we choose the country with the smallest educational inequalities in a risk factor (as identified by the upward levelling scenario, but making sure that small inequalities in this country stem from a low risk factor exposure among the low educated and not from a high risk factor exposure among the high educated). In the uncommon case that the prevalence of the risk factor was less favourable among high educated in the best practice country than in the country analysed, which mainly applies to smoking, we assume that the potential reduction of inequalities in mortality is zero. After we had identified the best-practice countries for each risk factor, we took the prevalences from both the highest and the lowest educational groups from these countries and applied them to other countries.
We used a specially developed, excel-based tool to quantify the expected changes in mortality that would result from modifying the population distribution of exposure to a risk factor. This tool is based on Population Attributable Fractions (PAF) and estimates the impact of counterfactual distributions of the risk factors on the magnitude of social inequalities in mortality [43].
The PAF is defined as the fraction of deaths which would have been avoided if the prevalence of a specific risk factor had been lower, and is measured with the following formula:
 |
n = number of exposure categories
Pi = proportion of population currently in the ith exposure category
P′i = proportion of population in the ith exposure category in the counterfactual (alternative) scenario
RRi = relative mortality risk for the ith exposure category
For the low- and mid-educated we first calculated age-specific PAFs in order to estimate new mortality rates and numbers of saved deaths in each age group (30–44, 45–59, 60–69 and 70–79). In a second step we summed up the age-specific saved deaths for the ages 30–79 years and calculated the overall PAF in each educational group.
To account for sampling variability, particularly of the risk factor distributions which were derived from survey data with limited sample sizes, we calculated 95% confidence intervals (CIs) around the PAF values of the lower educated using bootstrapping in R.
Results
Population-Attributable Fractions
Table 1 presents the educational inequalities in mortality as they were observed in the populations under study, on the basis of the mortality rate difference between the low and high educated, and shows that inequalities exist everywhere but vary importantly in magnitude: they are smallest in the South, and largest in the Centre/East.
Table 1. Mortality rate difference between low and high educated (in deaths per 100,000), by country and sex.
| Men | Women | |||||||||
| Age group | Age group | |||||||||
| Population | 30–44 | 45–59 | 60–69 | 70–79 | 30–79 | 30–44 | 45–59 | 60–69 | 70–79 | 30–79 |
| Finland | 291 | 537 | 926 | 1723 | 615 | 223 | 326 | 834 | 2188 | 260 |
| Sweden | 139 | 308 | 693 | 1539 | 418 | 76 | 203 | 431 | 930 | 258 |
| Norway | 198 | 438 | 989 | 2000 | 579 | 93 | 256 | 479 | 1069 | 304 |
| Denmark | 214 | 495 | 862 | 1660 | 554 | 103 | 259 | 590 | 970 | 319 |
| England/W | 75 | 321 | 662 | 1723 | 410 | 52 | 95 | 516 | 1167 | 245 |
| Scotland | 192 | 434 | 885 | 2112 | 568 | 120 | 240 | 623 | 1442 | 366 |
| Netherlands | 62 | 272 | 627 | 2248 | 430 | 49 | 134 | 382 | 609 | 185 |
| Belgium | 140 | 347 | 776 | 1646 | 456 | 61 | 131 | 304 | 871 | 200 |
| France | 201 | 507 | 902 | 2091 | 599 | 90 | 149 | 221 | 456 | 166 |
| Switzerland | 186 | 421 | 904 | 1720 | 528 | 72 | 114 | 188 | 666 | 160 |
| Austria | 168 | 478 | 958 | 1784 | 557 | 62 | 146 | 214 | 893 | 193 |
| Barcelona | 178 | 290 | 452 | 851 | 325 | 74 | 42 | 102 | 413 | 98 |
| Basque C. | 157 | 251 | 321 | 637 | 262 | 60 | 52 | −22 | 251 | 61 |
| Madrid | 176 | 285 | 418 | 804 | 312 | 47 | 10 | 160 | 470 | 90 |
| Turin | 105 | 198 | 648 | 944 | 304 | 41 | 65 | 34 | 70 | 51 |
| Tuscany | 117 | 248 | 506 | 1011 | 309 | 47 | 64 | 162 | 243 | 90 |
| Hungary | 678 | 2140 | 2481 | 3801 | 1788 | 211 | 463 | 587 | 883 | 425 |
| Czech R | 207 | 868 | 2226 | 4388 | 1158 | 74 | 288 | 745 | 1970 | 434 |
| Poland | 623 | 1208 | 1971 | 3414 | 1310 | 180 | 293 | 643 | 1458 | 413 |
| Lithuania | 668 | 1531 | 2018 | 2719 | 1389 | 294 | 575 | 646 | 1199 | 536 |
| Estonia | 1039 | 1680 | 2423 | 3028 | 1679 | 451 | 657 | 858 | 1532 | 691 |
| All # | ||||||||||
# Median value of all populations included in the analysis.
Table 2 presents the PAF values for each risk factor for the low educated. Values range between a little above 0 (e.g., for physical inactivity among Czech men, and for overweight among Estonian men) to more than 10% (e.g. for smoking among men and women in several countries, and for low income among men in Scotland, Hungary and Poland), implying that between 0 and more than 10% of all deaths among the low educated could be avoided if they would have the risk factor prevalence of the high educated in the same country.
Table 2. Potential reduction of all-cause mortality among the low educated if they would have the risk factor prevalence of the high educated (Population Attributable Fraction (in %, with 95% CI)), by risk factor, country and sex.
| Behavioural risk factors | Social and economic risk factors | |||||||||||
| Smoking | Overweight | Physical inactivity | Lack of social participation | Low income | Economic inactivity | |||||||
| Population | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women |
| Finland | 8.0 (6.7–9.1) | 3.5 (3.0–4.8) | 1.1 (0.9–1.6) | 3.4 (2.4–4.4) | 0.9 (0.7–1.2) | 0.3 (0.0–0.8) | 2.5 (2.4–2.6) | 1.9 (1.8–2.0) | 9.6 (8.8–10.3) | 4.4 (3.9–4.9) | 3.3 (3.2–3.4) | 3.2 (2.9–3.3) |
| Sweden | 8.1 (6.3–9.8) | 4.8 (3.5–6.2) | 2.7 (1.7–3.6) | 3.9 (2.9–4.7) | na | na | 1.9 (1.2–3.0) | 4.3 (3.2–5.2) | 8.9 (8.0–9.6) | 3.7 (3.2–4.2) | 2.8 (2.7–2.9)* | 3.0 (2.8–3.2) * |
| Norway | 14.0 (11.7–16.1 ) | 8.8 (7.0–10.5) | 3.5 (2.1–5.0) | 4.2 (3.1–5.4) | 2.3 (1.4–3.3) | 2.3 (1.7–2.9) | 3.1 (2.0–4.4) | 4.6 (3.3–5.9) | 9.3 (8.5–10.0) | 5.7 (5.2–6.1) | 3.5 (3.3–3.7) * | 3.8 (3.5–4.1) * |
| Denmark | 8.4 (6.8–9.9) | 3.5 (2.8–4.4) | 3.8 (2.8–4.7) | 4.1 (3.6–4.8) | 2.4 (1.7–3.1) | 4.4 (1.5–3.3) | 4.7 (3.1–6.1) | 3.5 (2.0–5.2) | 7.8 (7.3–8.1) | 4.0 (3.7–4.2) | na | na |
| England &W | 10.7 (9.6–11.9) | 5.9 (5.0–6.9) | 2.3 (1.5–3.1) | 4.8 (4.0–5.4) | na | na | 4.0 (2.9–5.1) | 4.2 (3.0–5.2) | 8.4 (7.9–8.8) | 5.3 (4.9–5.5) | 1.7 (1.5–1.9) | 2.0 (1.7–2.4) |
| Scotland | 11.1 (9.4–12.7) | 9.9 (8.5–11.1) | 2.5 (1.4–3.5) | 2.0 (1.2–3.0) | na | na | na | na | 10.0 (9.4–10.5) | 5.2 (4.8–5.6) | na | na |
| Netherlands | 5.5 (4.1–6.9) | 2.3 (1.8–2.9) | 3.7 (2.9–4.6) | 4.3 (3.7–4.9) | 1.0 (0.3–1.8) | 3.2 (2.3–3.9) | 2.2 (1.2–3.4) | 3.1 (2.0–4.1) | 8.6 (7.7–9.5) | 4.8 (4.2–5.3) | na | na |
| Belgium | 3.3 (2.5–4.3) | 0.8 (0.6–1.1) | 3.2 (2.5–3.9) | 5.5 (4.9–6.0) | 2.6 (2.1–3.1) | 7.1 (6.3–7.8) | 3.8 (2.4–5.1) | 1.6 (0.7–2.7) | 8.5 (8.1–8.8) | 4.9 (4.7–5.1) | na | na |
| France | 3.0 (2.4–4.3) | 0.9 (0.6–1.2) | 4.6 (3.9–5.4) | 6.2 (5.5–6.9) | na | na | 4.5 (3.2–5–5) | 6.1 (5.1–7.1) | 9.6 (8.6–10.5) | 6.4 (5.8–6.9) | na | na |
| Switzerland | 5.0 (3.1–7.1) | 0.7 (0.5–1.3) | 4.4 (3.4–5.4) | 6.4 (5.8–7.0) | 4.0 (3.0–5.0) | 5.8 (4.8–6.8) | na | na | 9.2 (7.6–10.8) | 4.9 (4.2–5.7) | 4.1 (3.9–4.3) * | 3.1 (3.0–3.3) * |
| Austria | 4.8 (3.2–7.5) | 0.6 (0.4–1.0) | 5.4 (3.7–6.9) | 6.7 (5.8–7.7) | na | na | 2.6 (1.7–3.7) | 7.0 (5.9–7.9) | na | na | 1.6 (1.4–1.7) | 2.4 (2.2–2.7) |
| Barcelona | 2.6 (2.3–3.3) | 0.5 (0.4–0.6) | 2.7 (2.2–3.1) | 6.4 (5.9–6.9) | 2.6 (2.5–2.8) | 2.8 (2.7–3.0) | 5.0 (4.1–5.8) | 2.1 (1.7–2.6) | na | na | na | na |
| Basque C | 2.7 (1.9–4.1) | 0.7 (0.4–1.0) | 1.4 (0.7–2.1) | 5.8 (5.1–6.4) | 2.6 (2.5–2.7) | 2.8 (2.7–3.0) | 5.0 (4.0–5.8) | 2.2 (1.7–2.6) | na | na | 1.1 (1.0–1.1) | 5.6 (5.2–6.0) |
| Madrid | 2.4 (2.1–3.0) | 0.4 (0.3–0.5) | 2.6 (2.2–3.1) | 6.3 (5.9–6.8) | 2.6 (2.4–2.7) | 2.7 (2.5.2.9) | 5.0 (4.1–5.9) | 2.0 (1.5–2.4) | na | na | 3.2 (3.1–3.3) * | 4.7 (4.4–5.0) * |
| Turin | 1.7 (1.5–2.1) | 0.2 (0.2–0.3) | 3.6 (3.4–3.8) | 5.3 (5.1–5.4) | 1.2 (1.1–1.4) | 2.0 (1.8–2.1) | 3.2 (2.1–4.4) | 1.4 (1.0–1.9) | na | na | 5.4 (5.2–5.5) * | 3.7 (3.2–4.1) * |
| Tuscany | 1.6 (1.4–2.0) | 0.3 (0.2–0.4) | 3.6 (3.4–3.8) | 5.3 (5.1–5.4) | 1.2 (1.1–1.4) | 2.0 (1.8–2.1) | 3.2 (2.0–4.5) | 1.4 (1.0–1.8) | na | na | na | na |
| Hungary | na | na | 1.4 (0.5–2.5) | 4.5 (3.7–5.2) | na | na | 5.1 (4.5–5.7) | 2.2 (1.7–2.8) | 10.6 (10.0–11.0) | 6.1 (5.7–6.3) | 4.9 (4.9–5.0) | 3.5 (3.4–3.6) |
| Czech R | 12.1 (9.2–14.9) | 2.7 (2.0–3.7) | 4.1 (2.4–5.7) | 5.7 (4.3–7.0) | 0.0 (0.0–0.6) | 1.6 (1.1–2.4) | na | na | 7.7 (6.2–9.1) | 4.1 (3.5–4.7) | na | na |
| Poland | 13.4 (12.2–14.3) | 2.6 (2.1–3.1) | 1.0 (0.6–1.6) | 5.9 (5.3–6.4) | na | na | 5.2 (4.9–5.5) | 2.1 (1.9–2.6) | 12.7 (11.6–13.6) | 5.1 (4.4–5.7) | na | na |
| Lithuania | 8.2 (6.7–9.5) | 2.1 (1.4–3.0) | 1.3 (0.4–2.3) | 2.0 (1.6–2.4) | 3.4 (2.6–4.2) | 6.8 (6.0–7.9) | na | na | na | na | na | na |
| Estonia | 8.4 (6.7–10.4) | 3.1 (2.0–4.5) | 0.1 (0.0–0.1) | 5.6 (4.0–7.1) | 1.5 (1.1–2.8) | 2.8 (1.5–4.3) | na | na | na | na | na | na |
| All # | 6.8 | 2.2 | 2.7 | 5.3 | 2.4 | 2.8 | 3.9 | 2.2 | 9.2 | 4.9 | 3.3 | 3.4 |
* economically inactive include unemployed.
na: data not available.
# Median value for all populations included in the analysis.
Normal font style: PAF less than 3%.
Bold font style: PAF between 3 and 10%.
Bold italic font style: PAF at least 10%.
As indicated by their non-overlapping 95% CIs, the observed differences in PAFs between countries are often unlikely to be due to random error. For example, reducing smoking prevalence to the level of the high educated will prevent a considerably larger fraction of deaths among the low educated in the North, West and Centre/East than in the South. This is due to the fact that inequalities in smoking prevalence are larger in the former than in the latter regions (see supporting information: Table S6 in File S1).
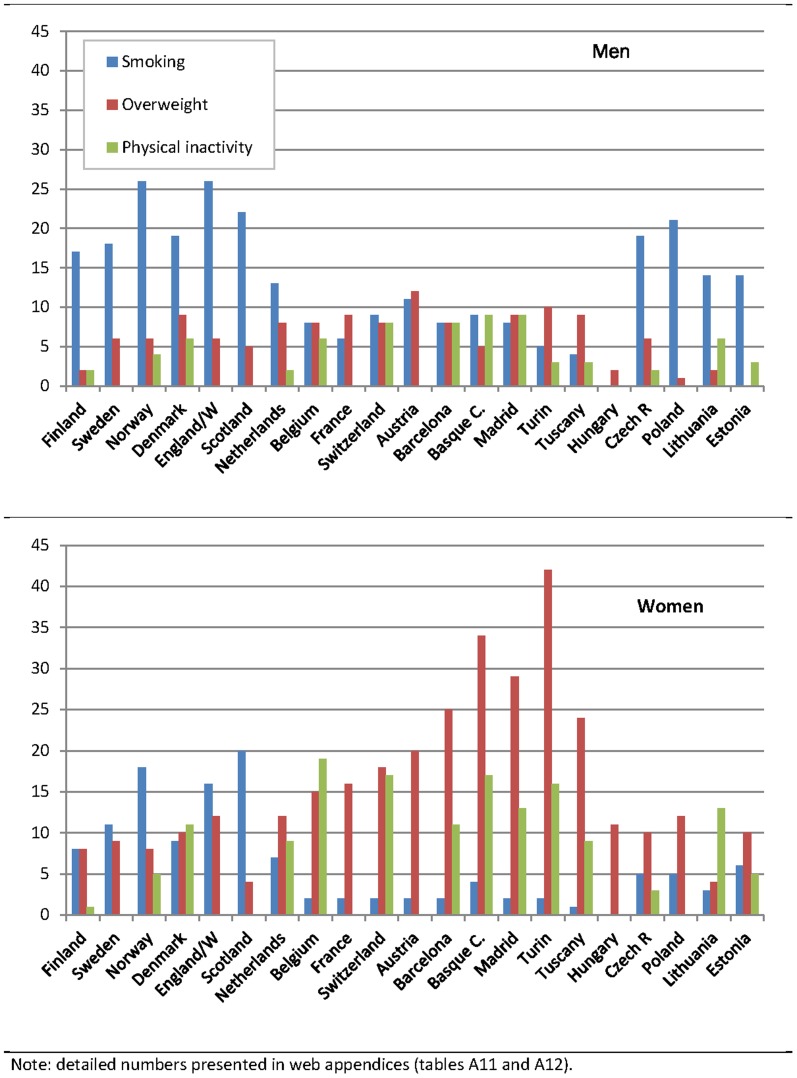
We present the impact of upward levelling and best practice scenarios on absolute inequalities in mortality in tables 3 and 4, respectively. Both tables visualize the potential impact across risk factors by use of colours ranging from yellow (none or minor impact) through light green to dark green (major impact). Reductions in relative inequalities for the same scenarios are presented in Figure 1 and Figure 2.
Table 3. Potential reduction of absolute educational inequalities in all-cause mortality between low and high educated (in deaths per 100,000 person-years), upward levelling scenario, by risk factor, country and sex.
| Behavioural risk factors | Social and economic risk factors | |||||||||||
| Smoking | Over-weight | Physical inactivity | Social participation | Low income | Economic inactivity | |||||||
| Population | M | W | M | W | M | W | M | W | M | W | M | W |
| Finland | 102 | 21 | 15 | 20 | 11 | 2 | 16 | 23 | 121 | 26 | 114 | 44 |
| Sweden | 76 | 28 | 25 | 22 | na | na | 17 | 25 | 83 | 22 | 59 * | 39 * |
| Norway | 152 | 55 | 37 | 25 | 25 | 15 | 33 | 29 | 101 | 35 | 113 * | 56 * |
| Denmark | 105 | 30 | 49 | 32 | 30 | 34 | 60 | 28 | 96 | 32 | na | na |
| England/W | 108 | 38 | 23 | 30 | na | na | 41 | 27 | 84 | 33 | 58 | 39 |
| Scotland | 125 | 74 | 28 | 15 | na | na | na | na | 111 | 39 | na | na |
| Netherlands | 54 | 12 | 36 | 23 | 10 | 17 | 20 | 16 | 84 | 25 | na | na |
| Belgium | 36 | 4 | 34 | 29 | 29 | 38 | 41 | 9 | 91 | 26 | na | na |
| France | 33 | 4 | 51 | 27 | na | na | 49 | 27 | 105 | 28 | na | na |
| Switzerland | 49 | 4 | 45 | 29 | 40 | 27 | na | na | 92 | 23 | 98 * | 28 * |
| Austria | 59 | 4 | 66 | 38 | na | na | 31 | 40 | na | na | 96 | 51 |
| Barcelona | 24 | 2 | 26 | 24 | 25 | 11 | 46 | 8 | na | na | na | na |
| Basque C. | 25 | 3 | 13 | 21 | 25 | 10 | 46 | 8 | na | na | 47 | 50 |
| Madrid | 26 | 2 | 28 | 27 | 28 | 11 | 52 | 8 | na | na | 58 * | 36 * |
| Turin | 14 | 1 | 30 | 21 | 10 | 8 | 27 | 6 | na | na | 75 * | 29 * |
| Tuscany | 13 | 1 | 28 | 21 | 10 | 8 | 26 | 6 | na | na | na | na |
| Hungary | na | na | 37 | 47 | na | na | 137 | 23 | 284 | 63 | 453 | 133 |
| Czech R | 216 | 22 | 69 | 45 | 26 | 14 | na | na | 137 | 33 | na | na |
| Poland | 273 | 22 | 19 | 48 | na | na | 106 | 17 | 258 | 41 | na | na |
| Lithuania | 200 | 16 | 30 | 21 | 83 | 69 | na | na | na | na | na | na |
| Estonia | 237 | 38 | 4 | 67 | 41 | 35 | na | na | na | na | na | na |
| All # | 68 | 14 | 30 | 27 | 26 | 14 | 41 | 20 | 101 | 32 | 96 | 50 |
Notes: na: data not available.
# Median value of all populations included in the analysis.
*Economically inactive include unemployed.
M = men, W = women.
Normal font style: reduction of mortality rate difference between low and high educated by 0–19 deaths per 100,000.
Bold font style: reduction of mortality rate difference between low and high educated by 20–79 deaths per 100,000.
Bold italic font style: reduction of mortality rate difference between low and high educated by at least 80 deaths per 100,000.
Table 4. Potential reduction of absolute educational inequalities in all-cause mortality between low and high educated (in deaths per 100,000 person-years), best practice scenario, by risk factor, country and sex.
| Behavioural risk factors | Social and economic risk factors | |||||||||||
| Smoking | Over-weight | Physical inactivity | Social participation | Low income | Economic inactivity | |||||||
| Population | M | W | M | W | M | W | M | W | M | W | M | W |
| Finland | 55 | 18 | ref | 0 | ref | ref | −12 | 5 | 20 | 1 | 12 | ref |
| Sweden | 33 | 58 | 0 | 0 | na | na | 0 | 1 | 14 | 6 | ref* | ref* |
| Norway | 83 | 80 | 1 | 0 | 72 | 73 | 14 | 1 | 48 | 26 | 13* | 13* |
| Denmark | 204 | 101 | 5 | 0 | 15 | 23 | 16 | 1 | 70 | 39 | na | na |
| England/W | 68 | 79 | 34 | 17 | na | na | 7 | 1 | 21 | 12 | ref | 40 |
| Scotland | 92 | 120 | 24 | ref | na | na | na | na | 27 | 10 | na | na |
| Netherlands | 76 | 52 | 0 | 0 | 41 | 39 | ref | 0 | 14 | 2 | na | na |
| Belgium | 97 | 32 | 0 | 0 | 31 | 40 | 4 | ref | 27 | 11 | na | na |
| France | ref | 4 | 3 | 0 | na | na | 17 | 7 | 13 | 6 | na | na |
| Switzerland | 87 | 25 | 0 | 0 | 15 | 17 | na | na | 19 | 10 | 0* | 18* |
| Austria | 3 | 5 | 10 | 0 | na | na | 16 | 13 | na | na | 17 | 54 |
| Barcelona | 18 | −2 | 9 | 3 | 59 | 32 | 32 | 4 | na | na | na | na |
| Basque C. | 11 | 3 | 2 | 0 | 52 | 23 | 31 | 3 | na | na | 5 | 45 |
| Madrid | 14 | −4 | 10 | 3 | 62 | 33 | 36 | 4 | na | na | 1* | 25 * |
| Turin | 11 | ref | 0 | 0 | 40 | 18 | 19 | 0 | na | na | 34 * | 21 * |
| Tuscany | 12 | 0 | 0 | 39 | 26 | 18 | 2 | na | na | na | na | |
| Hungary | na | na | 35 | 7 | na | na | 138 | 21 | 25 | 13 | 293 | 130 |
| Czech R | 114 | 31 | 35 | 16 | 140 | 105 | na | na | ref | ref | na | na |
| Poland | 226 | 39 | 29 | 14 | na | na | 153 | 48 | 14 | 8 | na | na |
| Lithuania | 193 | 1 | −14 | −6 | 121 | 112 | na | na | na | na | na | na |
| Estonia | 256 | 42 | −8 | 37 | 159 | 124 | na | na | na | na | na | na |
| All # | 76 | 32 | 2 | 0 | 52 | 33 | 17 | 3 | 20 | 10 | 14 | 50 |
Notes: na: data not available.
Median value of all populations included in the analysis.
*Economically inactive include unemployed (England/Wales and Finland is reference country for men and women respectively). Sweden is reference of countries with unemployed included in the active, both among men and women.
M = men, W = women.
Normal font style: reduction of mortality rate difference between low and high educated by 0–19 deaths per 100,000.
Bold font style: reduction of mortality rate difference between low and high educated by 20–79 deaths per 100,000.
Bold italic font style: reduction of mortality rate difference between low and high educated by at least 80 deaths per 100,000.
Figure 1. Potential reduction of relative educational inequalities in all-cause mortality between low and high educated (in %), upward levelling scenario according to smoking, overweight and physical activity by country and sex.
Figure 2. Potential reduction of relative educational inequalities in all-cause mortality between low and high educated (in %), upward levelling scenario according to social participation, low income and economic inactivity by country and sex.
Upward levelling scenarios
A complete elimination of inequalities in risk factors, by upward levelling of the prevalence of risk factors to the level currently seen in the highest education group, often results in a substantial reduction of absolute inequalities in mortality (table 3). However, this depends on the chosen risk factor and varies substantially between countries.
In most countries one can expect a notable decrease of inequalities in mortality among men, often by more than 80 deaths per 100 000 person years, if differences in smoking between educational groups would disappear, particularly in the North and Centre/East. However, the potential reduction is much smaller among women: outside the Nordic countries, the reduction of inequalities is often less than 20 deaths per 100 000 person years. Among men, elimination of inequalities in overweight or physical inactivity often has a smaller effect than elimination of inequalities in smoking, but among women overweight is often more important than smoking.
Among the social and economic risk factors, low income and economic inactivity are more important for tackling inequalities in mortality than lack of social participation, and also are often more important than smoking. Elimination of inequalities in low income would reduce inequalities in mortality by more than 80 deaths per 100 000 person years among men in all countries with available data. Upward levelling of the proportion of economically inactive people, in countries for which these data are available, also substantially reduces inequalities in mortality, particularly among Hungarian men and women (by 453 and 133 deaths per 100 000 person years, respectively).
The results for relative inequalities in mortality sometimes lead to a rather different picture of variation between countries (Figure 1 and Figure 2). The main reason is that relative inequalities in mortality do not vary between countries in the same pattern as absolute inequalities in mortality. For example, due to high average mortality rates absolute inequalities in mortality are particularly large in the Centre/East. As a result the reduction of the mortality Rate Difference is sometimes (e.g., in the case of smoking) largest here (table 3) but the reduction of the mortality Rate Ratio (Figure 1) is not. On the other hand, due to low average mortality rates the reduction of absolute inequalities is often small in the South (table 3) even if the reduction of relative inequalities is large (e.g., in the case of overweight (Figure 1) and economic inactivity (Figure 2)).
Best practice scenarios
Except from being a more realistic scenario, the best practice scenario differs from the upward levelling scenario in that the “best practice group” no longer stems from the same country (i.e., the highest educated group in each country), but from another country, and that the risk factor exposure among all educational levels is changed, not only that among the lower educated. This explains why best practice scenarios sometimes have larger effects than upward levelling scenarios. It should also be noted that the best practice scenarios sometimes have "negative" effects, in the sense that inequalities in mortality go up instead of down. This is the case when countries have a high average risk factor prevalence, and therefore could not be selected as best practice country, but at the same time have smaller inequalities in risk factor prevalence than the best practice country.
When we compare tables 3 and 4, the first thing to note is that best practice scenarios have a much smaller impact on inequalities in mortality than upward levelling scenarios for overweight, social participation, low income and economic inactivity (women only), but not for smoking and physical inactivity. These best practice scenarios suggest that substantial reductions (more than 20 or even 80 deaths per 100 000 person years) of absolute inequalities in mortality can realistically be achieved in many countries through smoking and physical inactivity, both among men and women (table 4). The distribution of income across educational groups is very similar across European countries. Therefore, reducing income inequalities to the level of the best practice country (the Czech Republic) will have only a minor impact on inequalities in mortality.
Still, small reductions of absolute inequalities may go together with sizable reductions in relative inequalities when average mortality levels are high, as in the case of Central/Eastern Europe (see supporting information: Table S9 in File S1).
Discussion
Our study has a number of important strengths, based on its wide geographical coverage and the application of straightforward quantitative methods. It explores a novel approach to identify entry-points for policies to tackle health inequalities, but in the implementation of this approach we encountered several limitations that all indicate a need for further research.
First, the scope of this study was limited by data availability. We could only include one indicator of socioeconomic position, and due to restrictions with regard to available data and/or available scientific knowledge we were unable to include the full range of potentially relevant risk factors in our analysis. Not all behavioural risk factors could be included, alcohol consumption being the prime example of a risk factor known to contribute importantly to inequalities in mortality in many European countries [3], [44], [45] but for which no reliable survey data are available. Specific material living conditions, such as those related to housing, work or environmental pollution, could not be included either. With the exception of social participation, psychosocial risk factors such as those relating to psychosocial stress [46], [47] were largely absent from the analysis as well.
Also, we only studied risk factors one-by-one, because available methods for combining them assume mutual independence [48] which would not be guaranteed in our case, e.g. because ‘downstream’ risk factors, such as smoking, are nested within the ‘upstream’ ones, such as low income. In an additional analysis reported elsewhere, we combined smoking and obesity, and showed that the combined effect of eliminating inequalities in both risk factors considerably exceeded the effects of each apart [42], [43]. This implies that the full potential for reducing inequalities in mortality may well be even larger than the separate estimates for the six single risk factors in our analysis suggest.
Second, while we have undertaken major harmonization efforts some potential comparability problems remain, e.g. related to the fact that mortality data for some countries are based on unlinked cross-sectional studies [49] and that data from a few countries could only be obtained from regions. However, educational differences in mortality in Turin and Tuscany are of the same magnitude as differences in Italy altogether [50], and the same applies to the Spanish regions and the whole of Spain [51]. We also compared the overall mortality rates in corresponding ages and corresponding years for men and women obtained from our regional data to national data available in the Human Mortality Database (HMD) (http://www.mortality.org/). The rates corresponded well to the national averages. We thus believe that our results on educational differences in disability-free life expectancy are not crucially affected by the use of regional mortality data instead of national data. Furthermore, the comparability of our economic inactivity data was clearly suboptimal because temporary unemployed were classified with the inactive in Norway, Sweden, Switzerland, and Madrid, and with the active in all other populations. This implies that the causal effect of economic activity on mortality will be different between these two groups of countries. However, different RRs were applied for these groups and we could also not find any systematic differences in reduction of mortality inequalities between countries with different classifications of the unemployed (table 3). Furthermore, the reasons for economic inactivity may vary between countries. The most common reason for economic inactivity among men is long term illness or disability, which could give rise to reverse causation [52]–[54], but they could also be studying for a qualification, staying at home to look after their family, or be retired [55]. The latter is less likely to be the case in our data given the restricted age range in our analyses. Among women, the main reason is that they look after their family, which is particularly common in the South. Despite these potential comparability problems, the data that we have used represent the best available data, and our main results are consistent with patterns that have been reported before on the basis of cause-specific mortality analyses [3].
A third group of limitations relates to the assumptions and uncertainties of the counterfactual estimations. It is of course debatable whether just by reducing the level of one risk factor to the level of the higher educated, this would prevent the number of deaths among the lower educated that we report here. Some of the assumptions underlying the method may be controversial [43]. We assume causality from risk factors to mortality (which is relatively unproblematic because we relied on systematic reviews that have tried to filter out the causal relationship between risk factors and mortality) but also from education to risk factors which is more uncertain. We also assume that the relative risks for the risk factors are the same for all countries, as there are no high-quality literature reviews on the impact of risk factors for each country available. Fortunately, an increasing body of evidence suggests that, when the metric of exposure is comparable, the relative risks are similar across populations in different world regions [56]. We further assume that the relative risks of the risk factors are the same for all educational groups. With respect to smoking, the Whitehall II study has suggested that smoking may be more harmful for those placed lower in the social hierarchy [57], but there is no systematic data on how the impact of proximate risk factors differs by socioeconomic group [43].
Furthermore, the exposure data have not always been collected for a point in time that allowed a lag-time before mortality effects occur. Take smoking as an example. Whether or not we have systematically under- or overestimated the potential for reducing inequalities in mortality by taking too recent prevalence data depends on whether changes in prevalence of smoking by education have occurred during this lag-time which, for some of the effects of smoking, may be 20 years or more. We know that in countries which are far advanced in the smoking epidemic inequalities in smoking behaviour have been increasing over time, especially among women [58]. However, in a study reported elsewhere we replaced current by historical smoking prevalence rates from the early 1980s for England and France. We found that in the upward levelling scenario the potential reduction of relative inequalities in mortality remained almost the same for English men and French men and women, while it declined from 16% to 8% among English women, suggesting that among the latter we may have overestimated the potential for reducing inequalities in mortality [59]. However, as this is an extreme case (not all risk factors have such long lag-times, and not all risk factors have equally dynamic distributional changes over time), most of our results are unlikely to be seriously affected by this problem.
Our analysis shows that in Europe smoking is the single most important ‘downstream’ risk factor for educational inequalities in mortality among men, and overweight is the most important among women. For smoking, this is in line with individual-level studies which have generally found important contributions of smoking to inequalities in mortality [4], [6]–[8], but it is important to note that most high-quality studies come from a small number of countries, and that our study therefore considerably expands the knowledge-base. We found substantial regional variations in the importance of smoking, in line with previous findings from the 1990s [3]: educational inequalities in smoking were and still are more important in the Centre/East (particularly among men) and in the North, and less important (or even “reverse”) in the South, probably because of differences in the progression of the smoking epidemic [17], [58], [60].
The relative importance of other ‘downstream’ risk factors than smoking has been less frequently studied, but previous studies have shown that overweight and obesity and physical inactivity contribute to the explanation of inequalities in mortality [4], [6]–[8]. We have taken this one step further by expanding geographic coverage and introducing a comparative perspective. Due to the fact that overweight and physical inactivity are more strongly socially patterned among women in the South than among women elsewhere in Europe [23], [61], perhaps because of traditional gender roles [61], these two risk factors are relatively important entry-points for policy in that part of the subcontinent.
Our findings for social and economic risk factors illustrate that distal or ‘upstream’ risk factors, particularly low income and economic inactivity, are also important entry-points for policies to tackle health inequalities. The role of upstream risk factors, such as income inequalities, economic activity status, and other aspects of socio-economic inequalities in generating health inequalities has been well documented [2], [35], [62], [63]. Welfare states provide a variety of social transfers (such as housing related benefits, unemployment, pensions, and sickness and disability benefits) as well as key services (most notably health care or social services), which may help to modify the impact of upstream risk factors on health [36], [64], [65]. The principles underpinning welfare states and the generosity of social transfers and entitlements vary extensively between welfare state regimes [65], and these variations may partly account for differences in the patterning of health inequalities [66], [67]. A causal effect of these upstream factors on mortality is less well established, however, so caution must be exercised in interpreting our findings. In the absence of experimental evidence on the impact of levelling income on inequalities in health, it is important to note that while inequalities in mortality are not smaller in countries with smaller income inequalities [3], [68], they are smaller in countries with smaller inequalities in smoking [3], [69], [70]. Further study is therefore necessary to corroborate our findings.
The upward-levelling scenarios demonstrated that there is a great theoretical potential for reducing inequalities in mortality in most European countries, for example by tobacco control policies, income redistribution, housing policies, labour market policies and social policies particularly aimed at those with less resources [66], [67]. The best practice scenarios often produced considerably smaller reductions in mortality inequalities than the upward levelling scenarios, but these were still substantial in many countries for smoking and physical inactivity. This suggests that achieving the theoretical potential may be feasible in some areas, but that in other areas more investments are needed in the development of effective interventions and policies to reduce inequalities in health. The results of the best-practice scenarios should also be interpreted in light of the fact that European countries are characterized by a large diversity of political histories [71], which may hinder policy learning and policy transfers between countries.
In any event, our study shows that each country needs its own tailored strategy for tackling health inequalities, and our study methods can be used to identify each country's main priorities for action. We did not find one country that had the smallest inequalities in all determinants of health inequalities. Instead, most countries can serve as an example for others, and inequalities in mortality could probably be reduced substantially if countries were willing and able to more systematically exchange experiences with tackling health inequalities.
Supporting Information
File includes Tables S1–S12. Table S1: Characteristics of the mortality data. Table S2: Rate ratios (from the EURO-GBD-SE mortality data set) for the association between education and all-cause mortality. Table S3: Relative risks for the impact of risk factors on all-cause mortality. Table S4: Sources of prevalences. Table S5: Prevalences of smoking. Table S6: Prevalences of overweight. Table S7: Prevalences of physical inactivity. Table S8: Prevalences of social participation. Table S9: Prevalences of lower income quartiles. Table S10: Prevalences of economic inactivity. Table S11: Potential reduction (in %) of relative educational inequalities in all-cause mortality between low and high educated, upward levelling scenario, by risk factor, country and sex. Table S12: Potential reduction (in %) of relative educational inequalities in all-cause mortality between low and high educated, best practice scenario, by risk factor, country and sex.
(DOCX)
Acknowledgments
The project partners are grateful to the European Commission for providing financial support and for using the project outputs as the basis for developing further initiatives. This article is based on data from the EURO-GBD-SE project. We are grateful to members of the EURO-GBD-SE consortium for providing access to data from mortality registries and national health surveys. The authors would like to thank Statistics Lithuania for providing high quality aggregated census-linked dataset for Lithuania. We are also grateful to Dalia Ambrozaitiene (Statistics Lithuania) and Vlada Stankuniene (Institute for Demographic Research (LSRC), Lithuania) for their expert advice on the Lithuanian mortality data.
Members of the EURO-GBD-SE consortium who have contributed to this analysis (in alphabetical order): Annibale Biggeri, Universita' Degli Studi Firenze, Tuscany, Italy; Mathias Bopp, Institute of Social and Preventive Medicine, University of Zurich, Switzerland; Carme Borrell, Agencia de Salut Publica de Barcelona, Barcelona, Spain; Bo Burström, Stockholm University, Stockholm, Sweden; Giuseppe Costa, Azienda Sanitaria Locale TO3 Regione Piemonte, Turin, Italy; Espen Dahl, Norwegian Institute of Public Health, Oslo, Norway; Patrick Deboosere, Vrije Universiteit Brussel, Brussels, Belgium; Stefaan Demarest, Scientific Institute of Public Health, Brussels, Belgium; Chris Dibben, University of St. Andrews, Scotland, United Kingdom; Dagmar Dzurova, Charles University, Prague, Czech Republic; Ola Ekholm, University of Southern Denmark, Copenhagen, Denmark; Santiago Esnaola, Basque Government, Department of Public Health, Vitoria-Gasteiz, Spain, Spain; Johan Fritzell, Centre for Health Equity Studies, Stockholm University, Stockholm, Sweden; Suzanne Fry, Office of National Statistics, England and Wales, United Kingdom; Satu Helakorpi, National Institute for Health and Welfare, Helsinki, Finland; Ken Judge, University of Bath, Bath, United Kingdom; Florence Jusot, Université Paris-Dauphine, Paris, France; Ramune Kalediene, Kaunas University of Medicine, Lithuania; Johannes Klotz, Statistics Austria, Austria; Jurate Klumbiene, Kaunas University of Medicine, Lithuania; Katalin Kovacs, Hungarian Central Statistical Office, Budapest, Hungary; Anita Lange, Statistics Denmark, Denmark; Mall Leinsalu, Tervise Arengu Instituut, Department of Biostatistics and Epidemiology, Tallinn, Estonia; Rita Lindbak, Norwegian Institute of Public Health, Oslo, Norway; Enrique Regidor, Universidad Complutense de Madrid, Madrid, Spain; Frederique Ruchon, Institute for research and information in health economics, Paris, France; Jitka Rychtarikova, Charles University, Prague, Czech Republic; Maica C. Rodríguez-Sanz, Agencia de Salut Publica de Barcelona, Barcelona, Spain; Bjørn Heine Strand, Norwegian Institute of Public Health, Division of Epidemiology, Oslo, Norway; Mare Tekkel, National Institute for Health Development, Estonia; Herman Van Oyen Scientific Institute of Public Health, Brussels, Belgium; Bogdan Wojtyniak, National Institute of Hygiene, Warsaw, Poland.
Data Availability
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. We have collected and combined data from three sources. 1) Our mortality data have been retrieved from national statistical offices in Finland, Sweden, Norway and Denmark, Scotland, England and Wales, Netherlands, Belgium, France, Switzerland, Barcelona, Basque Country and Madrid, Turin, Tuscany, Czech Republic, Poland, Hungary, Lithuania and Estonia. The original data can only be retrieved from each country directly. We have presented the sources of mortality data in appendix table A1 of our article. The second source of data was on self-reported morbidity and risk factors. These were collected from National Health Surveys (NHS), Health Examination Surveys (HES) and international surveys, some of which are publically available (such as the European Social Survey). We have presented the sources of morbidity data in appendix table A4 of the article. The third source of data were relative risks for the impact of smoking, overweight, physical inactivity and lack of social participation on mortality were collected from large reviews and meta-analyses. We have given reference to these studies in our own article. Further detailed descriptions of the sources, questionnaires, distributions etc can be found in the final report of the EURO-GBD-SE project (www.euro-gbd-se.eu).
Funding Statement
The project was funded by the European Commission, through the Public Health Programme, grant agreement 20081309, and the Netherlands Organisation for Health Research and Development (ZonMw), project number 121020026. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Commission on Social Determinants of Health (2008) Closing the gap in a generation. Health equity through the social determinants of health. Geneva: World Health Organization. [DOI] [PubMed]
- 2. Mackenbach JP, Kunst AE, Cavelaars AE, Groenhof F, Geurts JJ (1997) Socioeconomic inequalities in morbidity and mortality in western Europe. The EU Working Group on Socioeconomic Inequalities in Health. Lancet 349: 1655–1659. [DOI] [PubMed] [Google Scholar]
- 3. Mackenbach JP, Stirbu I, Roskam A-JR, Schaap MM, Menvielle G, et al. (2008) Socioeconomic Inequalities in Health in 22 European Countries. New England Journal of Medicine 358: 2468–2481. [DOI] [PubMed] [Google Scholar]
- 4. Laaksonen M, Talala K, Martelin T, Rahkonen O, Roos E, et al. (2008) Health behaviours as explanations for educational level differences in cardiovascular and all-cause mortality: a follow-up of 60 000 men and women over 23 years. European Journal of Public Health 18: 38–43. [DOI] [PubMed] [Google Scholar]
- 5. Marmot MG (2003) Understanding social inequalities in health. Perspect Biol Med 46: S9–23. [PubMed] [Google Scholar]
- 6. Schrijvers CT, Stronks K, van de Mheen HD, Mackenbach JP (1999) Explaining educational differences in mortality: the role of behavioral and material factors. Am J Public Health 89: 535–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stringhini S, Dugravot A, Shipley M, Goldberg M, Zins M, et al. (2011) Health behaviours, socioeconomic status, and mortality: further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Medicine 8: e1000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. van Oort FV, van Lenthe FJ, Mackenbach JP (2005) Material, psychosocial, and behavioural factors in the explanation of educational inequalities in mortality in The Netherlands. J Epidemiol Community Health 59: 214–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health (2003) Tackling health inequalities: a Program for Action. London: Department of Health.
- 10.Swedish National Institute of Public Health (2005) The 2005 Public Health Policy Report. Stockholm: Swedish National Institute of Public Health.
- 11.Norwegian Ministry of Health and Care Services (2007) National strategy to reduce social inequalities in health. Report No. 20 (2006–2007) to the Storting. Oslo: Norwegian Ministry of Health and Care Services.
- 12.Ministry of Social Affairs and Health (2008) National Action Plan to Reduce Health Inequalities 2008–2011. Helsinki: Ministry of Social Affairs and Health.
- 13.Acheson D, Barker D, Chambers J, Graham H, Marmot M, et al.. (1998) Independent inquiry into inequalities in health. London: The Stationery Office.
- 14. Mackenbach JP, Stronks K (2002) A strategy for tackling health inequalities in the Netherlands. BMJ 2: 1029–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Doll R, Peto R, Boreham J, Sutherland I (2004) Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ 328: 1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Flegal K, Kit BK, Orpana H, Graubard BI (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 309: 71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL (2006) Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. The Lancet 367: 1747–1757. [DOI] [PubMed] [Google Scholar]
- 18. Nocon M, Hiemann T, Müller-Riemenschneider F, Thalau F, Roll S, et al. (2008) Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil 15: 239–246. [DOI] [PubMed] [Google Scholar]
- 19. Cavelaars AEJM, Kunst AE, Mackenbach JP (1997) Socio-economic Differences in Risk Factors for Morbidity and Mortality in the European Community: An International Comparison. Journal of Health Psychology 2: 353–372. [DOI] [PubMed] [Google Scholar]
- 20. Cavelaars AJEM, Kunst AE, Geurts JJM, Crialesi R, Grötvedt L, et al. (2000) Educational differences in smoking: international comparison. BMJ 320: 1102–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demarest S, Roskam AJ, Cox B, Regidor E, Van Oyen H, et al.. (2007) Socio economic inequalities in leisure time physical activity. In: Kunst AE, Mackenbach JP, editors. Tackling health inequalities in Europe: An integrated approach. Rotterdam: Department of Public Health, Erasmus MC. [Google Scholar]
- 22. Huisman M, Kunst AE, Mackenbach JP (2005) Educational inequalities in smoking among men and women aged 16 years and older in 11 European countries. Tobacco Control 14: 106–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roskam A-JR, Kunst AE, Van Oyen H, Demarest S, Klumbiene J, et al. (2010) Comparative appraisal of educational inequalities in overweight and obesity among adults in 19 European countries. International Journal of Epidemiology 39: 392–404. [DOI] [PubMed] [Google Scholar]
- 24. Katikireddi SV, Higgins M, Smith KE, Williams G (2013) Health inequalities: the need to move beyond bad behaviours. Journal of Epidemiology and Community Health [DOI] [PubMed] [Google Scholar]
- 25. Link BG, Phelan J (1995) Social Conditions As Fundamental Causes of Disease. Journal of Health and Social Behavior 35: 80–94. [PubMed] [Google Scholar]
- 26. Phelan JC, Link BG, Tehranifar P (2010) Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. Journal of Health and Social Behavior 51: S28–S40. [DOI] [PubMed] [Google Scholar]
- 27. Akinwale B, Lynch K, Wiggins R, Harding S, Bartley M, et al. (2011) Work, permanent sickness and mortality risk: a prospective cohort study of England and Wales, 1971–2006. Journal of Epidemiology and Community Health 65: 786–792. [DOI] [PubMed] [Google Scholar]
- 28. Bartley M, Plewis I (2002) Accumulated labour market disadvantage and limiting long-term illness: data from the 1971–1991 Office for National Statistics' Longitudinal Study. International Journal of Epidemiology 31: 336–341. [PubMed] [Google Scholar]
- 29. Holt-Lunstad J, Smith TB, Layton JB (2010) Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med 7: e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. House JS, Landis KR, Umberson D (1988) Social relationships and health. Science 241: 540–545. [DOI] [PubMed] [Google Scholar]
- 31. Lindahl M (2005) Estimating the effect of income on health and mortality using lottery prizes as an exogenous source of variation in income. Journal of Human Resources 40: 144–168. [Google Scholar]
- 32. Martikainen P, Valkonen T (1999) Bias related to the exclusion of the economically inactive in studies on social class differences in mortality. International Journal of Epidemiology 28: 899–904. [DOI] [PubMed] [Google Scholar]
- 33. Möller H, Haigh F, Harwood C, Kinsella T, Pope D (2013) Rising unemployment and increasing spatial health inequalities in England: further extension of the North–South divide. Journal of Public Health 35: 313–321. [DOI] [PubMed] [Google Scholar]
- 34. Roelfs DJ, Shor E, Davidson KW, Schwartz JE (2011) Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Social Science and Medicine 72: 840–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bartley M, Owen C (1996) Relation between socioeconomic status, employment, and health during economic change, 1973–93. BMJ 313: 445–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Eikemo TA, Bambra C, Joyce K, Dahl E (2008) Welfare state regimes and income-related health inequalities: a comparison of 23 European countries. The European Journal of Public Health 18: 593–599. [DOI] [PubMed] [Google Scholar]
- 37. Gesthuizen M, van der Meer T, Scheepers P (2008) Education and Dimensions of Social Capital: Do Educational Effects Differ due to Educational Expansion and Social Security Expenditure? European Sociological Review 24: 617–632. [Google Scholar]
- 38. Daly MC, Duncan GJ, McDonough P, Williams DR (2002) Optimal indicators of socioeconomic status for health research. Am J Public Health 92: 1151–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lhachimi SK (2011) Dynamic Population Health Modeling for Quantitative Health Impact Assessment: Methodological Foundation and Selected Application. Rotterdam: Erasmus University.
- 40.Thun MJ, Day-Lally C, Myers DG, Calle EE, Flanders WD, et al.. (1997) Trends in Tobacco Smoking and Mortality From Cigarette Use in Cancer Prevention Studies I (1959 Through 1965) and II (1982 Through 1988). In: Bethesda MD, editor. Changes in cigarette-related disease risks and their implication for prevention and control Smoking and Tobacco Control Monograph 8: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute. pp. 305–382.
- 41. Martikainen P, Valkonen T (1996) Excess mortality of unemployed men and women during a period of rapidly increasing unemployment. Lancet 348: 909–912. [DOI] [PubMed] [Google Scholar]
- 42.Eikemo TA, Mackenbach JP (2012) The potential for reducing health inequalities in Europe. EURO-GBD-SE Final Report. Rotterdam: Department of Public Health, University Medical Centre Rotterdam.
- 43. Hoffmann R, Eikemo TA, Kulhanova I, Dahl E, Deboosere P, et al. (2013) The potential impact of a social redistribution of specific risk factors on socioeconomic inequalities in mortality: illustration of a method based on population attributable fractions. Journal of Epidemiology and Community Health 67: 56–62. [DOI] [PubMed] [Google Scholar]
- 44. Makela P, Valkonen T, Martelin T (1997) Contribution of deaths related to alcohol use to socioeconomic variation in mortality: register based follow up study. BMJ 315: 211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, et al. (2009) Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet 373: 2223–2233. [DOI] [PubMed] [Google Scholar]
- 46. Elstad JI (1998) The Psycho-social Perspective on Social Inequalities in Health. Sociology of Health & Illness 20: 598–618. [Google Scholar]
- 47. Stronks K, van de Mheen H, Looman CW, Mackenbach JP (1998) The importance of psychosocial stressors for socio-economic inequalities in perceived health. Social Science and Medicine 46: 611–623. [DOI] [PubMed] [Google Scholar]
- 48. Murray C, Ezzati M, Lopez A, Rodgers A, Vander Hoorn S (2003) Comparative quantification of health risks: Conceptual framework and methodological issues. Population Health Metrics 1: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Shkolnikov VM, Jasilionis D, Andreev EM, Jdanov DA, Stankuniene V, et al. (2007) Linked versus unlinked estimates of mortality and length of life by education and marital status: evidence from the first record linkage study in Lithuania. Social Science and Medicine 64: 1392–1406. [DOI] [PubMed] [Google Scholar]
- 50. Marinacci C, Sebastiani G, Ferracin E, Grippo F, Pappagallo M, et al. (2011) La distanza tra gli Italiani attraverso le disuguaglianze geografiche e socioeconomiche [Distance among Italians through geographic and socioeconomic inequalities]. Epidemiologia&Prevenzione 35: 2–9. [PubMed] [Google Scholar]
- 51. Reques L, Giraldez-Garcia C, Miqueleiz E, Belza MJ, Regidor E (2014) Educational differences in mortality and the relative importance of different causes of death: a 7-year follow-up study of Spanish adults. J Epidemiol Community Health [DOI] [PubMed] [Google Scholar]
- 52. Elstad JI, Krokstad S (2003) Social causation, health-selective mobility, and the reproduction of socioeconomic health inequalities over time: panel study of adult men. Social Science & Medicine 57: 1475–1489. [DOI] [PubMed] [Google Scholar]
- 53. Lindholm C, Burstrom B, Diderichsen F (2001) Does chronic illness cause adverse social and economic consequences among Swedes? Scand J Public Health 29: 63–70. [DOI] [PubMed] [Google Scholar]
- 54.Lissau I, Rasmussen NK, Hesse NM, Hesse U (2001) Social differences in illness and health-related exclusion from the labour market in Denmark from 1987 to 1994. Scand J Public Health Suppl 55: 19–30. [PubMed]
- 55.Minton JW, Pickett KE, Dorling D (2012) Health, employment, and economic change, 1973–2009: repeated cross sectional study. [DOI] [PMC free article] [PubMed]
- 56.GBD Study Operations Manual (2009): Harvard University, University of Washington, John Hopkins University, University of Queensland, World Health Organization.
- 57. Marmot MG, McDowall ME (1986) Mortality decline and widening social inequalities. Lancet 2: 274–276. [DOI] [PubMed] [Google Scholar]
- 58. Giskes K, Kunst AE, Benach J, Borrell C, Costa G, et al. (2005) Trends in smoking behaviour between 1985 and 2000 in nine European countries by education. J Epidemiol Community Health 59: 395–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kulik MC, Hoffmann R, Judge K, Looman C, Menvielle G, et al.. (forthcoming) Smoking and the potential for reduction of inequalities in mortality in Europe. European Journal of Epidemiology. [DOI] [PubMed]
- 60. Proctor RN (2004) The global smoking epidemic: a history and status report. Clin Lung Cancer 5: 371–376. [DOI] [PubMed] [Google Scholar]
- 61. Beenackers M, Kamphuis CB, Giskes K, Brug J, Kunst AE, et al. (2012) Socioeconomic inequalities in occupational, leisure-time, and transport related physical activity among European adults: A systematic review. International Journal of Behavioral Nutrition and Physical Activity 9: 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D (1997) Social capital, income inequality, and mortality. American Journal of Public Health 87: 1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wilkinson RG, Pickett K (2009) The Spirit Level: Why More Equal Societies Almost Always Do Better. London: Allen Lane.
- 64. Bambra C, Eikemo TA (2009) Welfare state regimes, unemployment and health: a comparative study of the relationship between unemployment and self-reported health in 23 European countries. Journal of Epidemiology and Community Health 63: 92–98. [DOI] [PubMed] [Google Scholar]
- 65. Eikemo TA, Bambra C, Judge K, Ringdal K (2008) Welfare state regimes and differences in self-perceived health in Europe: A multilevel analysis. Social Science & Medicine 66: 2281–2295. [DOI] [PubMed] [Google Scholar]
- 66. Lundberg O, Yngwe MA, Stjarne MK, Elstad JI, Ferrarini T, et al. (2008) The role of welfare state principles and generosity in social policy programmes for public health: an international comparative study. Lancet 372: 1633–1640. [DOI] [PubMed] [Google Scholar]
- 67. Brennenstuhl S, Quesnel-Vallee A, McDonough P (2012) Welfare regimes, population health and health inequalities: a research synthesis. J Epidemiol Community Health 66: 397–409. [DOI] [PubMed] [Google Scholar]
- 68. Hoffmann R (2011) Socioeconomic inequalities in old-age mortality: a comparison of Denmark and the USA. Social Science and Medicine 72: 1986–1992. [DOI] [PubMed] [Google Scholar]
- 69. Huisman M, Kunst AE, Bopp M, Borgan JK, Borrell C, et al. (2005) Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet 365: 493–500. [DOI] [PubMed] [Google Scholar]
- 70. Mackenbach JP, Huisman M, Andersen O, Bopp M, Borgan JK, et al. (2004) Inequalities in lung cancer mortality by the educational level in 10 European populations. European Journal of Cancer 40: 126–135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File includes Tables S1–S12. Table S1: Characteristics of the mortality data. Table S2: Rate ratios (from the EURO-GBD-SE mortality data set) for the association between education and all-cause mortality. Table S3: Relative risks for the impact of risk factors on all-cause mortality. Table S4: Sources of prevalences. Table S5: Prevalences of smoking. Table S6: Prevalences of overweight. Table S7: Prevalences of physical inactivity. Table S8: Prevalences of social participation. Table S9: Prevalences of lower income quartiles. Table S10: Prevalences of economic inactivity. Table S11: Potential reduction (in %) of relative educational inequalities in all-cause mortality between low and high educated, upward levelling scenario, by risk factor, country and sex. Table S12: Potential reduction (in %) of relative educational inequalities in all-cause mortality between low and high educated, best practice scenario, by risk factor, country and sex.
(DOCX)
Data Availability Statement
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. We have collected and combined data from three sources. 1) Our mortality data have been retrieved from national statistical offices in Finland, Sweden, Norway and Denmark, Scotland, England and Wales, Netherlands, Belgium, France, Switzerland, Barcelona, Basque Country and Madrid, Turin, Tuscany, Czech Republic, Poland, Hungary, Lithuania and Estonia. The original data can only be retrieved from each country directly. We have presented the sources of mortality data in appendix table A1 of our article. The second source of data was on self-reported morbidity and risk factors. These were collected from National Health Surveys (NHS), Health Examination Surveys (HES) and international surveys, some of which are publically available (such as the European Social Survey). We have presented the sources of morbidity data in appendix table A4 of the article. The third source of data were relative risks for the impact of smoking, overweight, physical inactivity and lack of social participation on mortality were collected from large reviews and meta-analyses. We have given reference to these studies in our own article. Further detailed descriptions of the sources, questionnaires, distributions etc can be found in the final report of the EURO-GBD-SE project (www.euro-gbd-se.eu).