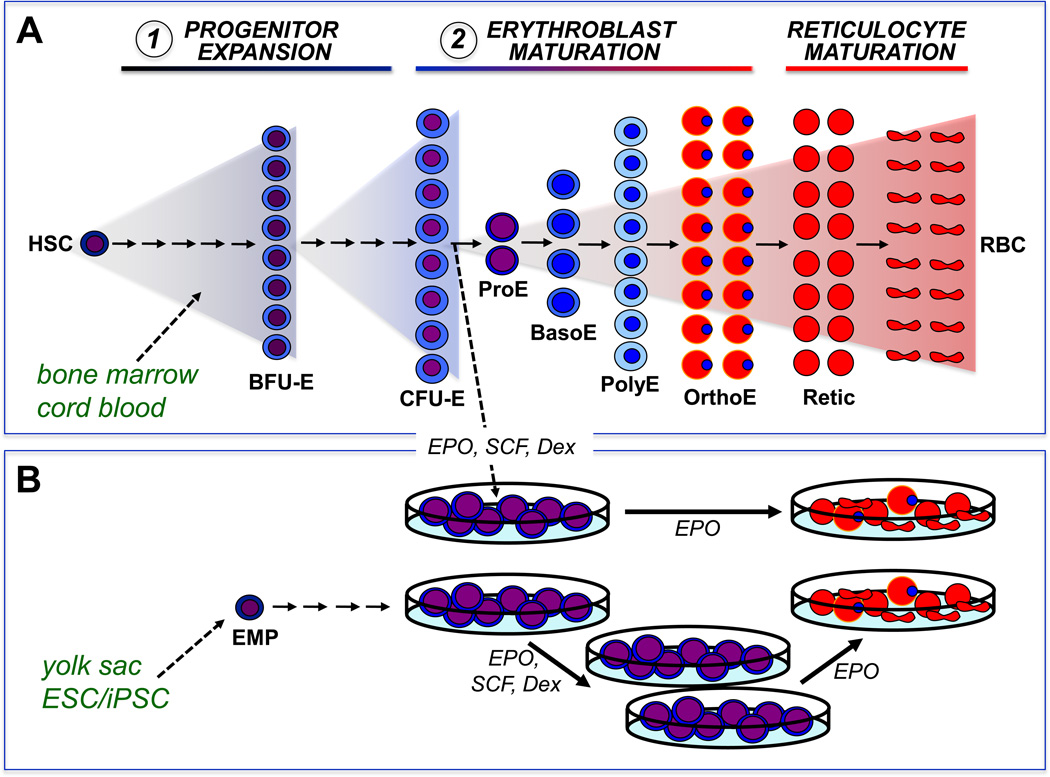
Figure 1.
Erythropoiesis is characterized by the progressive expansion of lineage-committed cells from progenitors, to morphologically identifiable precursors, that ultimately enucleate to form mature red blood cells (RBCs).
(A) In vivo, erythropoiesis proceeds from a small number of hematopoietic stem cells (HSC) that generate expanding numbers of lineage committed progenitors, termed burst-forming units erythroid (BFU-E) and colony-forming units erythroid (CFU-E). CFU-E subsequently generate erythroid precursors termed proerythroblasts (ProE), basophilic erythroblasts (BasoE), polychromatophilic erythroblasts (PolyE), and orthochromatic erythroblasts (OrthoE), that accumulate hemoglobin and condense their nucleus. Enucleation results in the generation of reticulocytes (Retic) that lose all internal organelles to become mature RBCs. Erythropoiesis has been modeled in vitro by using two or more steps of liquid culture. The first step is typically associated with the expansion of multipotential and lineage-specific erythroid progenitors, while the second step is associated with the terminal maturation of erythroblasts.
(B) In vitro, dexamethasone (Dex) synergizes with erythropoietin (EPO) and stem cell factor (SCF) to induce immature erythroblasts to undergo self-renewal cell divisions. When cultures are started from newborn or adult hematopoietic tissues, erythroblast self-renewal is ultimately restricted. In contrast, when cultures are initiated from yolk sac or early fetal liver or from differentiating embryonic stem cells that contain erythro-myeloid progenitors (EMP), erythroblasts can undergo extensive self-renewal in vitro. When the dexamethasone and SCF are removed from the cultures, these erythroblasts complete terminal maturation.