Abstract
The development of effective treatments for African Americans and other ethnic minorities is essential for reducing health disparities in substance use. Despite research suggesting that Motivational Enhancement Therapy (MET) may reduce substance use among African Americans, the findings have been inconsistent. This research examined the extent to which readiness-to-change (RTC) affects response to MET among African American substance users. The study was a secondary analysis of the 194 African American substance users participating in a multisite randomized clinical trial evaluating MET originally conducted within the National Drug Abuse Treatment Clinical Trials Network. The participants were randomly assigned to receive either three sessions of MET or Counseling-As-Usual (CAU) followed by the ordinary treatment and other services offered at the five participating outpatient programs. Participants were categorized as either high or lower on RTC based on their scores on the University of Rhode Island Change Assessment. The participants reported their substance use at baseline and throughout the 16 weeks after randomization. Among the high RTC participants, those in MET tended to report fewer days of substance use per week over time than participants in CAU. However, among the lower RTC participants, the CAU group tended to report fewer days of substance use over time than MET participants. In contrast to previous thinking, the findings suggest that MET may be more effective for high than lower RTC African American participants.
Keywords: readiness-to-change, African Americans, motivational enhancement therapy, substance use treatment
The limited number of substance abuse treatments with demonstrated efficacy for African Americans is a barrier to reducing health disparities (Burlew et al., 2011; Marsh, Cao, Guerrero, & Shin, 2009; Shaya, Gbarayor, Yang, Agyeman-Duah, & Saunders, 2007; Wells, Klap, Koike, & Sherbourne, 2001). This shortcoming raises even more concerns as a growing body of literature suggests that evidence-based interventions for one group may not be particularly effective with other groups (Calsyn et al., 2012; Covey et al., 2008, 2010; Robbins et al., 2002; Winhusen et al., 2008). Nevertheless, some promising evidence suggests that Motivational Enhancement Therapy (MET) may be effective for African Americans (Hettema, Steele, & Miller, 2005; Montgomery, Burlew, Kosinski, & Forcehimes, 2011; Montgomery, Burlew, Wilson, & Hall, 2011; Winhusen et al., 2008). However, the inconsistent findings raise the possibility that some third factor may influence the relationship between MET participation and treatment outcomes. This research examined whether readiness-to-change (RTC) affects response to MET treatment.
Motivational Interviewing/Motivational Enhancement Therapy
Motivational interviewing (MI) is a brief intervention aimed at reducing addictive and other maladaptive behaviors by building motivation to change and strengthening commitment to change (Miller & Rollnick, 2002; Rollnick, Miller, & Butler, 2008). MET adapts MI by incorporating personal assessment feedback within the overall clinical style of MI. Both interventions utilize the following basic strategies: expressing empathy, developing discrepancy between current maladaptive behaviors and future goals, avoiding argumentation, rolling with resistance and supporting self-efficacy. MI/MET strategies include collaboration (vs. an authoritarian approach), evocation (eliciting rather than imparting wisdom or insight), and a respect for the client’s autonomy (instead of giving directives).
Several recent meta-analyses support MI/MET efficacy (Burke, Arkowitz, & Minchola, 2003; Hettema et al., 2005; Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010; Vasilaki, Hosier, & Cox, 2006). However, the outcomes of the motivational interventions in two meta-analyses were better than no treatment controls but not better than other active treatments (Burke et al., 2003; Lundahl et al., 2010). Based on the inconsistent findings across studies, Hettema et al. recommended more studies to identify moderator variables that may influence the efficacy of motivational interventions. Past research suggesting that treatment response may vary depending on the readiness for change (Callaghan et al., 2005; Carbonari & DiClemente, 2000; Cox, Pothos, & Hosier, 2007; DiClemente, 1999; Li, Ding, Lai, Lin, & Luo, 2011) combined with past assumptions that MET may be most effective for individuals ambivalent about change (Hettema et al., 2005) raise the possibility that RTC, a potential moderator of the relationship between treatment type and outcome, may help to explain the inconsistent findings on MI/MET efficacy.
Stage-of-Change and Readiness-to-Change
The stage-of-change concept is grounded in the Transtheoretical Model (TTM) of Change. The underlying assumption is that behavior change proceeds in a progression of distinct stages: precontemplation (i.e., no perceived need for change), contemplation (i.e., some ambivalence about changing), preparation (i.e., resolved ambivalence enough to consider changing), action (i.e., taking steps toward change), and maintenance (i.e., implementing strategies to maintain behavior change) (DiClemente, Schlundt, & Gemmell, 2004; Erol & Erdogan, 2008). Each stage specifies tasks and goals to be achieved (DiClemente et al., 2004; Erol & Erdogan, 2008).
The University of Rhode Island Change Assessment (URICA) is a commonly used RTC measure in research on substance abuse (Field, Adinoff, Harris, Ball, & Carroll, 2009; Napper et al., 2008; Pantalon, Nich, Frankforter, & Carroll, 2002) and other behaviors (Dozois, Westra, Collins, Fung, & Garry, 2004; Edwards et al., 2006; Tambling & Johnson, 2012). The scale includes items corresponding to the theoretical stages of change. However, previous research did not support the preparation stage so the URICA items only assess agreement with the characteristic attitudes of the other four stages. The Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity) research identified a higher order factor structure and, ultimately, a continuous RTC scale (Project MATCH Research Group, 1997). This continuous readiness measure is conceptualized as a pragmatic assessment of the willingness and motivation to engage in a particular behavior.
Previous research suggests the role of RTC may vary depending on the specific outcome. That research demonstrates that RTC is associated with higher treatment adherence (Pantalon & Swanson, 2003) and retention (Blanchard, Morgenstern, Morgan, Labouvie, & Bux, 2003; O’Toole, Pollini, Ford, & Bigelow, 2006). However, the findings in studies investigating the relation of RTC to substance use outcomes are inconsistent. Blanchard et al. (2003) did not find a relationship between RTC and substance use outcomes. In addition, RTC was not related to marijuana use outcomes over time in three treatment studies of marijuana dependence for adults (Callaghan et al., 2008).
MI/MET has been described as more effective for individuals ambivalent about change (e.g., in the precontemplation or contemplation stages of change) (Bien, Miller, & Tonigan, 1993; Brown & Miller, 1993; Hettema et al., 2005; Rollnick et al., 2008) than for individuals already committed to change. However, the actual empirical findings have left the nature of the relationship unclear. Several previous studies examined whether the response to MI/MET varied with the level of RTC. For instance, Maisto et al. (2001) found that the response to MET (e.g., decrease in alcohol use) did not vary with RTC. However, Leontieva and colleagues found that the response to MET did vary with RTC. Specifically, individuals in the action stage (“ready to change”) participating in a motivational intervention were more likely than individuals in the precontemplation (“not ready to change”) stage to display decreases in their alcohol use (Leontieva et al., 2005). Further, although another study (Field et al., 2009) reported that RTC was associated with better substance use outcomes among MET participants, the relationship between RTC and substance use outcomes was the same for participants in both MET and standard treatment. In another study, Heather, Rollnick, Bell, and Richmond (1996) divided their sample into not ready to change and ready to change subgroups and conducted separate analyses for the two groups. Among the individuals classified as not ready to change, those assigned to a motivational intervention reduced their alcohol use more than individuals assigned to a skill-based comparison group. However, among individuals classified as ready to change, the outcomes for the motivational intervention group were no better than the skills-based group. Clearly, more research is warranted to determine the benefits of MET for more motivated individuals.
MIs for African Americans
The findings for African Americans were inconsistent in several meta-analyses addressing MET efficacy. Lundahl et al. (2010) reported an inverse relationship between the number of African Americans in the sample and the overall mean MI/MET effect size in their meta-analysis of 119 studies. However, Hettema et al. (2005) concluded from their meta-analysis of 72 studies that the effects of MI may be more positive for ethnic minorities than Caucasians.
The research examining the role of stage-of-change or RTC among African American substance users specifically is particularly limited. Neither of the two studies described earlier on the relationship of RTC to outcomes (Blanchard et al., 2003; Field, Duncan, Washington, & Adinoff, 2007) examined the findings specifically for African Americans. Yet, Huey and Polo (2008) caution against generalizing the findings across ethnic groups without first examining findings for a specific ethnic group.
Our literature review identified only two RTC studies on African American substance users. Both are fairly dated. Schorling (1995) reported a relationship between stage-of-change and African American attitudes about smoking cessation. Voorhees et al., (1996) demonstrated that African American participants in a multimodal culturally relevant intervention progressed further along a stage of change continuum to quit smoking than African American participants in the self-help intervention. Yet, to our knowledge, no previous research has investigated the RTC influence on African American response to MI/MET. The absence of research on the influence of RTC on MI/MET efficacy represents another gap in the knowledge base.
Addressing several noteworthy gaps in the current research may begin to explain the inconsistencies in the findings for African Americans. First, the meta-analyses and other reviews examined MI/MET interventions across a range of behaviors including diet (Martins & McNeil, 2009; Resnicow et al., 2001), physical activity (Befort et al., 2008; Resnicow et al., 2005), risky sexual behaviors (Carey et al., 2000; Rutledge, 2007), and increasing medication adherence (Ogedegbe et al., 2006). Yet, few previous studies examine MI outcomes specifically for African American substance users (Longshore & Grills, 2000; Montgomery et al., 2011). Second, the few studies evaluating MI/MET efficacy for reducing substance use among African Americans or other ethnic minorities either used a culturally tailored version of MI (Longshore & Grills, 2000) or combined African Americans with other ethnic minorities for the analyses (Winhusen et al., 2008). The third gap is that, despite the call by Hettema et al. (2005) for moderator variable studies, few moderator variable studies with African American samples are available. RTC is one potential moderator underexamined for African Americans.
The Present Study
The present study is a secondary analysis of a multisite randomized clinical trial (CTN-0004) evaluating MET and originally conducted within the Clinical Trials Network (CTN). Results from the original trial revealed a relationship between higher RTC scores and better treatment outcomes. However, the RTC relationship was the same for both MET and the control group (Field et al., 2009).
This CTN-0004 data set is ideal for examining RTC as a moderator of MI/MET effects for African Americans because the sample included 194 African Americans from five community treatment programs. Moreover, the study used the URICA to assess RTC. A secondary analysis of the data set revealed some interesting outcome differences between the African American subgroup and the overall sample (Montgomery, Burlew, Kosinski, et al., 2011). The overall findings revealed no retention differences between participants in MET and those in standard treatment. However, an analysis of the African Americans in the sample revealed higher retention rates among women in MET than those in standard treatment. No differences were observed among men. Those differences in other areas raise the possibility that RTC may also play a different role in the response to MET among African Americans than other groups.
This study addresses the gaps in the literature by adding RTC as a variable in a study of the treatment outcomes among African American substance users participating in a generic (i.e., not culturally tailored) version of MET. The objective of this research is to examine the extent to which RTC affects response to MET among African Americans. Our specific research question is whether highly motivated African American substance users respond differently to MET than other African American substance users.
Method
Participants
The inclusion criteria for CTN-0004 required participants to be (1) seeking outpatient treatment for any substance use disorder; (2) acknowledging substance use within 28 days prior to the study; (3) at least 18 years of age; (4) willing to participate in the protocol; and (5) able to understand and provide written informed consent. Participants who self-identified as African American or Black were included in the present study. Participants not medically or psychiatrically stable enough to participate in outpatient treatment and/or individuals seeking detoxification, methadone maintenance treatment, or residential treatment only were ineligible.
The sample for this secondary analysis included the 194 African American participants in CTN 0004. The mean age of the sample was 37.5 years (SD = 9.9). Approximately one fourth (24.7%) of the sample was women. Participants reported using alcohol (26.3%), cocaine (25.8%), marijuana (18.0%), two or more drugs (24.2%), or other drugs (5.6%) as their primary drug of choice. Approximately, one fourth (27.3%) of the participants were court mandated. Further details are provided elsewhere (Montgomery et al., 2011).
The participants were enrolled in one of the five participating community based treatment programs (CTPs). The CTPs met the following eligibility criteria: (1) program offered outpatient, non-methadone maintenance treatment; (2) patient flow sufficient to enroll target number of participants (i.e., 100 participants per CTP, with 50 participants per treatment group); and (3) at least six clinicians were willing to participate in the protocol. Further information on the CTN study is available in Ball et al. (2007), the CTN-0004 protocol (Carroll et al., 2001), and a recent publication focusing on the African Americans in the sample (Montgomery et al., 2011).
The participating clinicians were randomly assigned to deliver either MET or Counseling-as-Usual (CAU). However, clinicians with prior MI/MET training were ineligible to participate. Instead, clinicians were required to be willing to learn a manualized version of MET (if assigned to MET) and to permit clinical supervisors to review audiotaped sessions.
Measures
The measures used to assess each variable in the secondary analyses are described below.
Self-reported substance use
The Substance Use Calendar (SUC), a self-report measure of substance use, assesses the use of marijuana, cocaine, alcohol, methamphetamine, benzodiazepines, opioids, and other illicit drugs. The SUC is an adaptation of the Time Line Follow Back (TLFB) (Sobell & Sobell, 1992). Fals-Stewart, O’Farrell, Freitas, McFarlin, and Rutigliano (2000) established the reliability and validity of the TLFB. Both the SUC and the TLFB first probe participants for significant events to increase their memory of their activities during the period. Then, participants are asked to recall any substance use during the period.
Stage of change
The URICA, a 32-item self-report measure, assesses readiness-to-change (DiClemente et al., 2004). The readiness composite of the URICA is derived by subtracting the precontemplation score from the sum of contemplation, action, and maintenance scales. RTC scores on the URICA can range from −16 to 112. The concurrent validity of this continuous readiness measure has been reported as just as good as using motivational subtypes (Blanchard et al., 2003) to classify stage-of-change.
Demographic information
The demographic form developed for the original study included self-report information on age, gender, ethnicity, and primary drug type.
Procedures
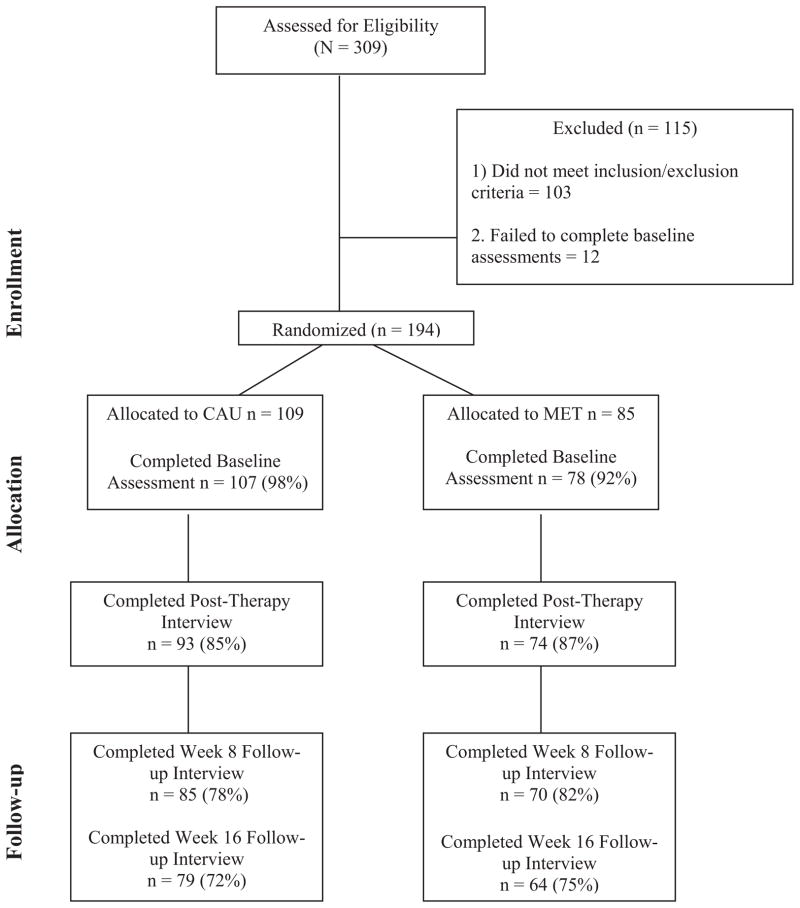
The consort diagram in Figure 1 describes the steps in the original study and the eligibility, enrollment, randomization, and treatment and follow-up rates for African American participants. Individuals enrolling in outpatient substance abuse treatment at each of the five CTPs were referred to the research assistant trained to introduce the study and to obtain written consent. Ineligible and uninterested participants were returned immediately to standard treatment. Research assistants collected baseline information from consented participants and then randomly assigned participants to either CAU or MET via urn randomization (Stout, Wirtz, Carbonari, & DelBoca, 1994). The variables in the original study for urn randomization included gender, race, primary drug, referral type (mandated or voluntary), and employment status.
Figure 1.
CONSORT diagram of eligibility, enrollment, randomization, treatment, and follow-up rates. CAU = Counseling as Usual; MET = Motivational Enhancement Therapy. Note. The highest number of participants providing data at any time point was recorded as the total n for each time point. The number in parentheses beside the n is the percent of the total randomized to the specific treatment.
The participants received either three sessions of MET or CAU followed by the ordinary treatment and other services offered in their outpatient program. Research assistants attempted to schedule weekly meetings with the participants during the 4-week active phase and then recontacted the participants to collect additional information 8 and 16 weeks after randomization. At each assessment, the research assistants collected information on substance use and other participant information included in the original study.
CAU
A CAU protocol was implemented to standardize the CAU treatment at the various CTPs. The treatment included three sessions (45–55 min each) during the course of the 4-week active phase. Trained clinicians inquired about substance use and psychosocial functioning in these sessions. In addition, the counselor addressed any questions regarding the requirements of the treatment program, discussed treatment goals including abstinence, provided early case management and substance use counseling, and encouraged attendance at all treatment activities at the clinic including 12-step meetings (Ball et al., 2007). The supervisor scheduled monthly meetings with the clinicians to review treatment progress. Also, audiotaped CAU sessions were later rated for adherence and competence.
MET
The MET treatment was also delivered in three sessions (45–55 min each) during the 4-week active phase. MET clinicians followed the protocol in a MET manual (Farentinos & Obert, 2000) developed for this study. The manual describes “three carefully planned sessions, with the first session focused on reviewing an individualized Personal Feedback Report (i.e., summarizes objective and personal information on participants’ substance use), and the second two focused on discussing plans for changing substance use” (Carroll et al., 2001, p. 12). The clinician’s goal was to enhance the client’s own motivation and commitment to change.
Drs. William Miller and Theresa Moyers trained the local expert MET trainers who subsequently trained and supervised the MET study clinicians. The local expert trainers provided 16 hr of didactic training to the study clinicians and then supervised the clinicians conducting practice sessions with outpatients not participating in the main study. The local experts, after rating the clinicians on adherence, ultimately certified the clinicians as competent to provide MET before assigning any study cases to the clinicians. Supervisors continued to monitor the clinicians after certification by reviewing one tape per week and providing biweekly supervision. The local expert provided additional training and supervision if the clinician’s adherence drifted below the initial certification level. Further details on both treatments are available in an article by Ball et al. (2007) and in the CTN-0004 protocol (Carroll et al., 2001).
Data Analysis Plan
The outcome measure was the self-reported number of days of primary substance use per week for each of the 16 study weeks. RTC scores in the upper quartile (at least 90.5) were classified as high RTC in this study. All other scores (lower than 90.5) were classified as lower RTC scores. Longitudinal analysis with linear mixed modeling (LMM) was performed with days of primary substance use per week as the outcome (the dependent variable) and treatment assignment, RTC, time, and interactions as the independent variables. A random intercept in the model accounted for the correlation of outcome over time for each patient. Because the relationship between outcome and time relationship was not linear, a parsimonious final model considered time trajectories modeled by two slopes. The first slope includes the 1-week period from baseline through Week 1. The second slope includes the remainder of study period, that is, from the beginning of Week 2 all the way through end of Week 16. A single model estimated the treatment effect in each RTC group, as well as the interaction of RTC and treatment. The corresponding p values resulted from specification of appropriate contrasts. p values of .05 or less were considered significant with no adjustment for multiplicity of comparisons. However, to reduce the potential of a false significant result, the main comparison (interaction between treatment and level of readiness) was prespecified. Not all patients had substance use information for each of the 16 weeks. However, LMM, a likelihood-based method, is valid under the missing at random (MAR) assumption that missingness is unrelated to any unobserved variable. Although verifying the MAR assumption with observed data may not be possible, this assumption is commonly used in the literature (Xu & Blozis, 2011). Statistical Analysis Software was used to perform the analyses.
Results
Sample Characteristics
The overall RTC scores at baseline (M =81.6, SD =13.1) suggested the level of motivation was generally high. The participants reported their highest days of use per week at baseline (mean equal to 2.5 days). The mean days of use per week after baseline ranged from a low of 0.41 at week 1 to a high of 0.73 at week 15. The mean days of use per week at week 16 was 0.70. The general trend toward more substance use across time starting from use at week 1 (0.41 days per week) to week 16 (0.70 days per week) was statistically significant (p =.02).
Main Findings
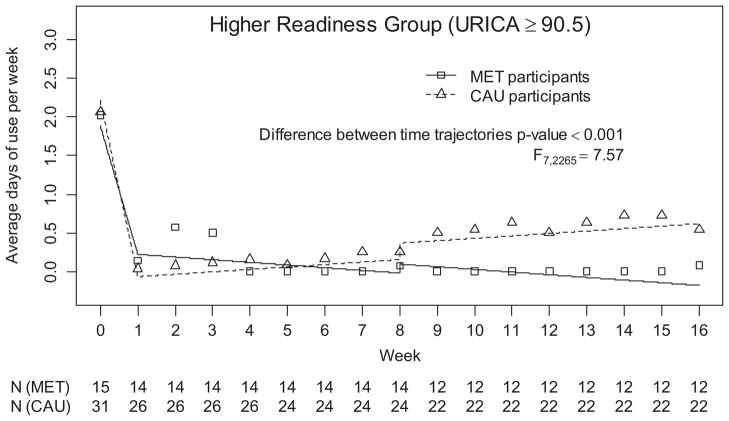
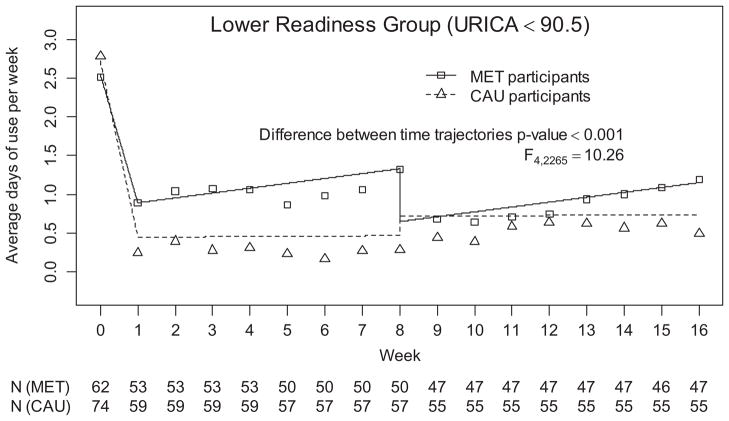
The pattern of change in average days of primary drug use over time for the high and lower RTC groups appears in Figures 2 and 3, respectively. In both figures, the squares represent the observed average weekly primary substance use for the MET participants and the triangles display the same information for the CAU participants. The lines correspond to the fitted model. The relationship of treatment type to primary substance use differed for the high and lower RTC participants, interaction, F(3, 2265), p =.009, =3.89. The pattern of change over time is presented in Figure 2 for the high-RTC participants and in Figure 3 for the lower-RTC participants. The high-RTC participants tended to report fewer days of substance use per week over time in MET than CAU especially during the longer term follow-up period, F(7, 2265) =7.57, p <.001. However, the lower-RTC participants tended to report fewer days of substance use over time in CAU than MET participants, especially during weeks 1–8, F(4, 2265) =10.26, p <.001.
Figure 2.
Average days of primary substance use per week for high-readiness participants by treatment across time. MET =Motivational Enhancement Therapy; CAU =Counseling as Usual. Symbols display observed average days of weekly use. Lines reflect the fitted model. Number (N) of participants with available data for each week is listed under the plot separately for each treatment type.
Figure 3.
Average days of primary substance use per week for lower-readiness participants by treatment across time. CAU =Counseling as Usual; MET =Motivational Enhancement Therapy. Lines reflect the fitted model. Symbols display observed average days of weekly use. Number (N) of participants with available data for each week is listed under the plot separately for each treatment type.
Discussion
This study contributes to the public health need for more empirical evidence on effective substance abuse treatments for African Americans. This study extends existing research by examining the role of RTC on the response to a generic version of MET and CAU specifically among African Americans. The research question was whether RTC affects response to MET among African American substance users.
The pattern of change in response to MET varied depending on RTC. Specifically, among the high-RTC group, MET participants had better outcomes (i.e., reported fewer days of substance use per week) over time than CAU participants. This difference was particularly evident at the long-term follow-up. However, the opposite pattern was evident for the lower-RTC group. Lower-RTC participants in CAU actually reported fewer days of substance use over time than MET participants. Although high-RTC participants in MET had better outcomes than lower-RTC participants in a study by Field et al. (2009), the present study builds on that study in two ways. First, the sample was predominately White in the previous study, so it is unclear if the findings apply to the ethnic minorities in the study. The present study addressed that limitation by examining outcomes specifically among African Americans. Moreover, the Field et al. study did not specifically investigate whether high-RTC in MET had better outcomes than high-RTC in TAU.
The findings partially support the Transtheoretical Model of Change. One corollary of this theory is that the most appropriate treatment may vary depending on an individual’s motivation for change. Nevertheless, our findings are inconsistent with previous assumptions that MET is better suited for those ambivalent about change (Heather et al., 1996; Hettema et al., 2005). Instead, our findings suggest that MET may be more appropriate for more motivated African American substance users than those who are ambivalent about change.
One disclaimer seems appropriate before fully supporting this conclusion. Participant scores on the readiness and the precontemplation scales suggest the participants were fairly motivated overall. Therefore, as might be expected in a treatment seeking group, the sample included few precontemplators. Accordingly, one might argue that our findings support the efficacy of MET for high RTC over moderate RTC participants. The findings may be different in a sample with a higher proportion of low RTC participants.
Our findings suggest an alternative explanation for the inconsistent findings in the previous evaluations of African American response to MET. Specifically, the findings raise the possibility that the failure to consider RTC may explain (at least in part) the inconsistencies in previous research on the response to MET (Hettema et al., 2005; Lundahl et al., 2010). More research is needed to address this issue.
This research had several strengths. First, the study addressed an important gap in the literature on the role of RTC in the substance abuse treatment among African Americans. As mentioned earlier, we only identified two previous RTC studies with African Americans and both were completed two decades ago. Second, the study was a secondary analysis of a larger, multisite randomized clinical trial. The extensive training of the MET therapists and the use of only certified therapists was a third strength. Finally, the longitudinal analysis addressed substance use over time rather than substance use solely at a particular point in time.
All secondary analyses impose some limitations on the design. In this case, the reliance on self-report on the substance use calendar may be perceived as a limitation. The accuracy of self-report data is a long-standing issue in substance use research (Carroll, 1995). The fact that approximately one fourth of the participants were court mandated raises the concern that individuals may be reluctant to disclose their drug use. We were only able to use self-report because the original study only collected urine data during the 4-week active period of the intervention and not during the follow-up periods. However, the high concordance rate (86%) between self-reports of drug use and the urine screens collected during the 4-week active phase of the intervention in the parent study (Ball et al., 2007) increases our confidence in the self-report findings. Moreover, previous research on the consistency between self-report data and physiological also supports the validity of self-report data (Shillington, Cottler, Mager, & Comp-ton, 1995; Vitale, van de Mheen, van de Wiel, & Garretsen, 2006). The second limitation is that our findings were restricted to the first 16 weeks after enrollment. However, future research might examine whether these positive findings persist 6 months after treatment, 1 year, or longer. Third, as mentioned earlier, future research might examine whether the outcomes for MET and CAU differ when individuals closer to the precontemplation stage are better represented. Finally, this study examined the response of African Americans to a generic version of MET. Because a culturally tailored version of MET yielded even more favorable outcomes for African Americans than this generic version in an earlier study (Longshore & Grills, 2000), future research should consider the role of RTC in studies evaluating the efficacy of culturally tailored versions of MET.
Future research might address several additional issues. First, the finding of the association between RTC and response to MET raises other interesting questions about substance abuse treatment for African Americans. One important question is the pathway explaining the effect of MET on outcomes for highly motivated African Americans. For example, research supports change talk (i.e., talk in favor of making a behavior change; Apodaca & Longabaugh, 2009) as a pathway that might explain the positive relationship between MET and treatment outcomes. Additional analyses of the sample used in this study revealed that the therapists’ attempts to elicit higher levels of change talk were associated with fewer days of self-reported primary substance use over time among participants (Montgomery, Burlew, & Lewis, 2012). Future research might address this issue by further examining whether change talk, particularly client change talk, and variables in other stage of change studies such as self-efficacy (DiClemente, Prochaska, & Gibertini, 1985), barriers to change (Sørensen & Gill, 2008), or social support (Vallis et al., 2003) mediate the relationship between treatment type and substance use outcomes differently for high- versus lower-RTC African Americans. The present study was not large enough to examine for gender differences after we had already divided the sample into high- and lower-RTC groups. However, because previous research suggests that African American men and women may respond differently to MET (Montgomery et al., 2011), future research might examine whether the relationship between RTC and response to MET might be different for African American men and women. Finally, we were particularly interested in whether highly motivated participants may respond differently to MET than other participants. Therefore, we assigned those who were in the upper quartile into one group and everyone else to a second group. However, future researchers may examine whether the relationship between treatment type and outcome varies with alternative ways of splitting the sample.
Although RTC was associated with better outcomes in the overall CTN-0004 sample, the relationship between RTC and treatment outcomes was the same for MET and CAU participants. The difference between the role of RTC in this African American subgroup and the overall CTN-0004 sample (Field et al., 2009) supports our previous recommendations to examine the results for specific ethnic groups rather than assuming findings obtained in the general population are generalizable to specific ethnic groups (Burlew, Feaster, Brecht, & Hubbard, 2009). Our finding is consistent with a growing number of substance abuse treatment studies demonstrating that various ethnic groups may respond differently to both behavioral (Montgomery et al., 2011; Robbins et al., 2002; Winhusen et al., 2008) and medication (Covey et al., 2008, 2010) substance use therapies.
Summary
This research examined the extent to which highly motivated African American substance users respond differently than other African American substance users to MET. Participants in this study were classified as either high-RTC (upper quartile) or lower-RTC (all others). The findings revealed different patterns of change over time for the high- and lower-RTC participants. Among the high-RTC participants, those in MET tended to report fewer days of substance use per week over time than participants in CAU. However, among the lower-RTC participants, the CAU group tended to report fewer days of substance use over time than MET participants. In contrast to previous thinking, the findings suggest that MET may be more effective for high-than lower-RTC African American participants.
Acknowledgments
This research was supported by the National Institute of Drug Abuse (NIDA) Grant 5U10DA013732-13. NIDA had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or the decision to submit the paper for publication.
Contributor Information
Ann Kathleen Burlew, Department of Psychology, University of Cincinnati.
LaTrice Montgomery, Department of Psychology, University of Cincinnati.
Andrzej S. Kosinski, Department of Biostatistics and Bioinformatics, Duke University School of Medicine/Duke Clinical Research Institute
Alyssa A. Forcehimes, Department of Psychology, University of New Mexico/Center on Alcoholism, Substance Abuse and Addictions
References
- Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2009;104:705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball SA, Martino S, Nich C, Frankforter TL, Van Horn D, Crits-Cristoph P, Carroll KM, et al. Site matters: Multisite randomized trial of Motivational Enhancement Therapy in community drug abuse clinics. Journal of Consulting and Clinical Psychology. 2007;75:556–567. doi: 10.1037/0022-006X.75.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Befort CA, Nollen N, Ellerbeck EF, Sullivan DK, Thomas JL, Ahluwalia JS. Motivational interviewing fails to improve outcomes of a behavioral weight loss program for obese African American women: A pilot randomized trial. Journal of Behavioral Medicine. 2008;31:367–377. doi: 10.1007/s10865-008-9161-8. [DOI] [PubMed] [Google Scholar]
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: A review. Addiction. 1993;88:315–335. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Blanchard KA, Morgenstern J, Morgan T, Labouvie E, Bux D. Motivational subtypes and continuous measure of readiness for change: Concurrent and predictive validity. Psychology of Addictive Behaviors. 2003;17:56–65. doi: 10.1037/0893-164X.17.1.56. [DOI] [PubMed] [Google Scholar]
- Brown JM, Miller R. Impact of Motivational Interviewing on participation and outcome in residential alcoholism treatment. Psychology of Addictive Behaviors. 1993;7:211–218. doi: 10.1037/0893-164X.7.4.211. [DOI] [Google Scholar]
- Burke BL, Arkowitz H, Minchola M. The efficacy on Motivational Interviewing: A meta-analysis of clinical controlled trials. Journal of Consulting and Clinical Psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Burlew AK, Feaster D, Brecht M, Hubbard R. Measurement and data analysis in research addressing health disparities in substance abuse. Journal of Substance Abuse Treatment. 2009;36:25–43. doi: 10.1016/j.jsat.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burlew K, Larios S, Suarez-Morales L, Holmes B, Venner K, Chavez R. Increasing ethnic minority participation in substance abuse clinical trials: Lessons learned in the National Institute on Drug Abuse’s Clinical Trial Network. Cultural Diversity & Ethnic Minority Psychology. 2011;17:345–356. doi: 10.1037/a0025668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan RC, Hathaway A, Cunningham JA, Vettese LC, Wyatt S, Taylor L. Does stage-of-change predict dropout in a culturally diverse sample of adolescents admitted to inpatient substance-abuse treatment? A test of the Transtheoretical Model. Addictive Behaviors. 2005;30:1834–1847. doi: 10.1016/j.addbeh.2005.07.015. [DOI] [PubMed] [Google Scholar]
- Callaghan RC, Taylor L, Moore BA, Jungerman FS, Vilela FA, Budney AJ. Recovery and URICA stage-of-change scores in three marijuana treatment studies. Journal of Substance Abuse Treatment. 2008;35:419–426. doi: 10.1016/j.jsat.2008.03.004. [DOI] [PubMed] [Google Scholar]
- Calsyn DA, Burlew AK, Hatch-Maillette M, Wilson J, Beadnell B, Wright L. Real Men Are Safe–culturally adapted: Utilizing the Delphi process to revise Real Men Are Safe for an ethnically diverse group of men in substance abuse treatment. AIDS Education and Prevention. 2012;24:117–131. doi: 10.1521/aeap.2012.24.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calsyn DA, Hatch-Maillette M, Tross S, Doyle SR, Crits-Cristoph P, Song YS, Berns SB, et al. Motivational and skills training HIV/STI sexual risk reduction groups for men. Journal of Substance Abuse Treatment. 2009;37:138–150. doi: 10.1016/j.jsat.2008.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonari JP, DiClemente CC. Using transtheoretical model profiles to differentiate levels of alcohol abstinence success. Journal of Consulting and Clinical Psychology. 2000;68:810–817. doi: 10.1037/0022-006X.68.5.810. [DOI] [PubMed] [Google Scholar]
- Carey MP, Braaten LS, Maisto SA, Gleason JR, Forsyth AD, Durant LE, Jaworski BC, et al. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women. Health Psychology. 2000;19:3–11. doi: 10.1037/0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- Carroll KM. Methodological issues and problems in the assessment of substance use. Psychological Assessment. 1995;7:349–358. doi: 10.1037/1040-3590.7.3.349. [DOI] [Google Scholar]
- Carroll K, Ball S, Crits-Cristoph P, Farentinos C, McLellan T, Morgenstern J, Woody G, et al. Clinical Trial Network (CTN) OOO4 Protocol: Motivational Enhancement Treatment to improve treatment engagement and outcome in individuals seeking treatment for substance abuse. Bethesda, MD: National Institute of Drug Abuse; 2001. [Google Scholar]
- Covey LS, Botello-Harbaum M, Glassman AH, Masmela J, LoDuca C, Salzman V, Fried J. Smokers’ response to combination bupropion, nicotine patch and counseling treatment by race/ethnicity. Ethnicity and Disease. 2008;18:59–64. [PubMed] [Google Scholar]
- Covey LS, Hu M, Winhusen T, Weissman J, Berlin I, Nunes E. Orosmethylphenidate or placebo for adult smokers with Attention Deficit Hyperactivity Disorder: Racial/ethnic differences. Drug and Alcohol Dependence. 2010;110:156–159. doi: 10.1016/j.drugalcdep.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox WM, Pothos EM, Hosier SG. Cognitive-motivational predictors of excessive drinkers’ success in changing. Psychopharmacology. 2007;192:499–510. doi: 10.1007/s00213-007-0736-9. [DOI] [PubMed] [Google Scholar]
- DiClemente CC. Motivation for change: Implications for substance abuse treatment. Psychological Science. 1999;10:209–213. doi: 10.1111/1467-9280.00137. [DOI] [Google Scholar]
- DiClemente CC, Prochaska JO, Gibertini M. Self-efficacy and the stages of self-change of smoking. Cognitive Therapy and Research. 1985;9:181–200. doi: 10.1007/BF01204849. [DOI] [Google Scholar]
- DiClemente CC, Schlundt D, Gemmell L. Readiness and stages of change in addiction treatment. The American Journal on Addictions. 2004;13:103–119. doi: 10.1080/10550490490435777. [DOI] [PubMed] [Google Scholar]
- Dozois DJA, Westra HA, Collins KA, Fung TS, Garry JKF. Stages of change in anxiety: Psychometric properties of the University of Rhode Island Change Assessment. Behaviour Research and Therapy. 2004;42:711–729. doi: 10.1016/S0005-7967(03)00193-1. [DOI] [PubMed] [Google Scholar]
- Edwards TA, Houry D, Kemball RS, Harp SE, McNutt LA, Straus H, Kaslow NJ, et al. Stages of change as a correlate of mental health symptoms in abused, low-income African American women. Journal of Clinical Psychology. 2006;62:1531–1543. doi: 10.1002/jclp.20310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erol S, Erdogan S. Application of a stage based motivational interviewing approach to adolescent smoking cessation: The Transtheoretical Model-based study. Patient Education and Counseling. 2008;72:42–48. doi: 10.1016/j.pec.2008.01.011. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The Timeline Followback reports of psychoactive substance use by drug-abusing patients. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037/0022-006X.68.1.134. [DOI] [PubMed] [Google Scholar]
- Farentinos C, Obert JL. CTN motivational enhancement treatment manual. 2000 Unpublished manuscript. [Google Scholar]
- Field CA, Adinoff B, Harris TR, Ball SA, Carroll KM. Construct, concurrent and predictive validity of the URICA: Data from two multi-site clinical trials. Drug and Alcohol Dependence. 2009;101:115–123. doi: 10.1016/j.drugalcdep.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field CA, Duncan J, Washington K, Adinoff B. Association of baseline characteristics and motivation to change among patients seeking treatment for substance dependence. Drug and Alcohol Dependence. 2007;91:77–84. doi: 10.1016/j.drugalcdep.2007.05.009. [DOI] [PubMed] [Google Scholar]
- Heather N, Rollnick S, Bell A, Richmond R. Effects of brief counseling among male heavy drinkers identified on general hospital wards. Drug and Alcohol Review. 1996;15:29–38. doi: 10.1080/09595239600185641. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller W. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Huey SJ, Polo A. Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child and Adolescent Psychology. 2008;37:262–301. doi: 10.1080/15374410701820174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leontieva L, Horn K, Haque A, Helmkamp J, Ehrlich P, Williams J. Readiness to change problematic drinking assessed in the emergency department as a predictor of change. Journal of Critical Care. 2005;20:251–256. doi: 10.1016/j.jcrc.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Li L, Ding Y, Lai W, Lin C, Luo W. Motivational profiles of clients seeking methadone maintenance therapy in China. Drug and Alcohol Dependence. 2011;118:335–340. doi: 10.1016/j.drugalcdep.2011.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longshore D, Grills C. Motivating illegal drug use recovery: Evidence for a culturally congruent intervention. Journal of Black Psychology. 2000;26:288–301. doi: 10.1177/0095798400026003002. [DOI] [Google Scholar]
- Lundahl B, Kunz C, Brownell C, Tollefson D, Burke B. A meta-analysis of Motivational Interviewing: Twenty-five years of empirical studies. Research on Social Work Practice. 2010;20:137–160. doi: 10.1177/1049731509347850. [DOI] [Google Scholar]
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro R, Kelley M. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. Journal of Studies on Alcohol. 2001;62:605–614. doi: 10.15288/jsa.2001.62.605. [DOI] [PubMed] [Google Scholar]
- Marsh JC, Cao D, Guerrero E, Shin HC. Need-service matching in substance abuse treatment: Racial/ethnic differences. Evaluation and Program Planning. 2009;32:43–51. doi: 10.1016/j.evalprogplan.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins RK, McNeil DW. Review of Motivational Interviewing in promoting health behaviors. Clinical Psychology Review. 2009;29:283–293. doi: 10.1016/j.cpr.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing. 2. New York, NY: Guilford Press; 2002. [Google Scholar]
- Montgomery L, Burlew AK, Kosinski A, Forcehimes A. Motivational Enhancement Therapy for African American substance users: A randomized clinical trial. Cultural Diversity & Ethnic Minority Psychology. 2011;17:357–365. doi: 10.1037/a0025437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery L, Burlew AK, Lewis D. The influence of change talk and decisional balance on treatment outcomes among African American substance users. 2012 Manuscript in preparation. [Google Scholar]
- Montgomery L, Burlew K, Wilson J, Hall R. Promising evidence-based treatments for African-Americans: Motivational Interviewing/Motivational Enhancement Therapy. In: Columbus AM, editor. Advances in psychology research. New York, NY: Nova Science Publishers; 2011. [Google Scholar]
- Napper LE, Wood MM, Jaffe A, Fisher DG, Reynolds GL, Klahn JA. Convergent and discriminant validity of three measures of stage of change. Psychology of Addictive Behaviors. 2008;22:362–371. doi: 10.1037/0893-164X.22.3.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogedegbe G, Schoenthaler A, Richardson T, Lewis L, Belue R, Espinosa E, Charlson ME, et al. An RCT of the effect of motivational interviewing on medication adherence in hypertensive African Americans: Rationale and design. Contemporary Clinical Trials. 2007;28:169–181. doi: 10.1016/j.cct.2006.04.002. [DOI] [PubMed] [Google Scholar]
- O’Toole TP, Pollini RA, Ford D, Bigelow G. Physical health as a motivator for substance abuse treatment among medically ill adults: Is it enough to keep them in treatment? Journal of Substance Abuse Treatment. 2006;31:143–150. doi: 10.1016/j.jsat.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Pantalon MV, Nich C, Frankforter T, Carroll K. The URICA as a measure of motivation to change among treatment-seeking individuals with concurrent alcohol and cocaine problems. Psychology of Addictive Behaviors. 2002;16:299–307. doi: 10.1037/0893-164X.16.4.299. [DOI] [PubMed] [Google Scholar]
- Pantalon MV, Swanson A. Use of the University of Rhode Island Change Assessment to measure motivational readiness to change in psychiatric and dually diagnosed individuals. Psychology of Addictive Behaviors. 2003;17:91–97. doi: 10.1037/0893-164X.17.2.91. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Resnicow K, Jackson A, Wang T, De AK, McCarty F, Dudley W, Baranowski T. A motivational interviewing intervention to increase fruit and vegetable intake though Black churches: Results of the Eat for Life trial. American Journal of Public Health. 2001;91:1686–1693. doi: 10.2105/AJPH.91.10.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins MS, Kumar S, Walker-Barnes C, Feaster D, Briones E, Szapocznik J. Ethnic differences in comorbidity among substance-abusing adolescents referred to outpatient therapy. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:394–401. doi: 10.1097/00004583-200204000-00011. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Miller WR, Butler CC. Motivational Interviewing in health care: Helping patients change behavior. New York, NY: Guilford Press; 2008. [DOI] [Google Scholar]
- Rutledge SE. Single-session motivational enhancement counseling to support change toward reduction of HIV transmission by HIV positive persons. Archives of Sexual Behavior. 2007;36:313–319. doi: 10.1007/s10508-006-9077-8. [DOI] [PubMed] [Google Scholar]
- Schorling JB. The stages of change of rural African-American smokers. American Journal of Preventive Medicine. 1995;11:170–177. [PubMed] [Google Scholar]
- Shaya FT, Gbarayor CM, Huiwen KY, Agyeman-Duah M, Saunders E. A perspective on African American participation in clinical trials. Contemporary Clinical Trials. 2007;28:213–217. doi: 10.1016/j.cct.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Shillington AM, Cottler LB, Mager DE, Compton WM., III Self-report stability for substance use over 10 years: Data from the St. Louis Epidemiologic Catchment Study. Drug and Alcohol Dependence. 1995;40:103–109. doi: 10.1016/0376-8716(95)01176-5. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana; 1992. pp. 41–72. [DOI] [Google Scholar]
- Sørensen M, Gill DL. Perceived barriers to physical activity across Norwegian adult age groups, gender and stages of change. Scandinavian Journal of Medicine & Science in Sports. 2008;18:651–663. doi: 10.1111/j.1600-0838.2007.00686.x. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, DelBoca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol Supplement. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Tambling RB, Johnson LN. An exploratory factor analysis of the URICA among couple therapy participants. The Family Journal. 2012;20:63–69. doi: 10.1177/1066480711429537. [DOI] [Google Scholar]
- Vallis M, Ruggiero L, Greene G, Jones H, Zinman B, Rossi S, Prochaska JO, et al. Stages of change for healthy eating in diabetes: Relation to demographic, eating-related, health care utilization and psychosocial factors. Diabetes Care. 2003;26:1468–1474. doi: 10.2337/diacare.26.5.1468. [DOI] [PubMed] [Google Scholar]
- Vasilaki EI, Hosier S, Cox W. The efficacy of Motivational Interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol and Alcoholism. 2006;41:328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Vitale SG, van de Mheen H, van de Wiel A, Garretsen H. Substance use among emergency room patients: Is self-report preferable to biochemical markers? Addictive Behaviors. 2006;31:1661–1669. doi: 10.1016/j.addbeh.2005.12.011. [DOI] [PubMed] [Google Scholar]
- Voorhees CC, Stillman F, Swank R, Heagerty P, Levine D, Becker D. Heart, body, and soul: Impact of church-based smoking cessation interventions on readiness to quit. Preventive Medicine. 1996;25:277–285. doi: 10.1006/pmed.1996.0057. [DOI] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse and mental health care. The American Journal of Psychiatry. 2001;158:2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- Willoughby FW, Edens JF. Construct validity and predictive utility of the stages of change for alcoholics. Journal of Substance Abuse. 1996;8:275–291. doi: 10.1016/S0899-3289(96)90152-2. [DOI] [PubMed] [Google Scholar]
- Winhusen T, Kropp F, Babcock D, Hague D, Erickson SJ, Renz C, et al. Smoza E. Motivational enhancement therapy to improve treatment utilization and outcome in pregnant substance users. Journal of Substance Abuse Treatment. 2008;35:161–173. doi: 10.1016/j.jsat.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu S, Blozis SA. Sensitivity analysis of mixed models for incomplete longitudinal data. Journal of Educational and Behavioral Statistics. 2011;36:237–256. doi: 10.3102/1076998610375836. [DOI] [Google Scholar]