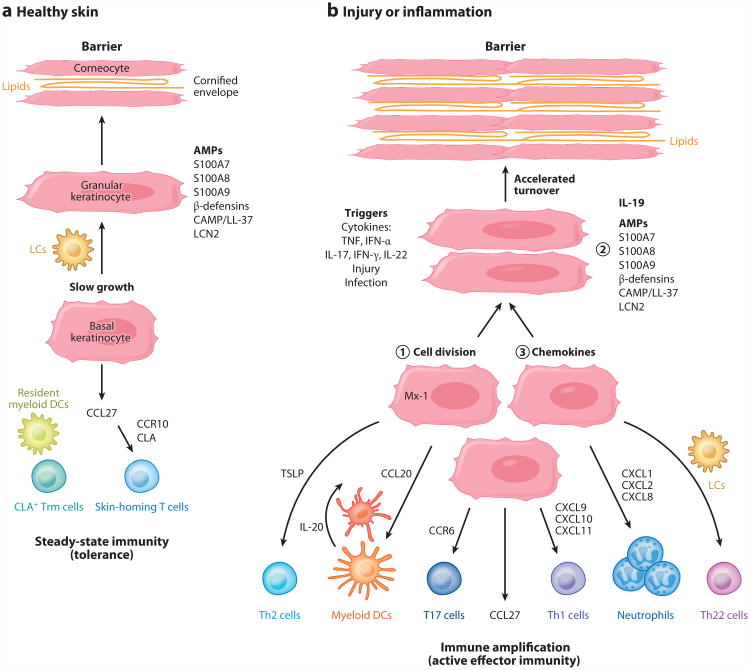
Figure 1.
Components of healthy and inflamed skin. (a) The epidermis is formed by slowly differentiating keratinocytes. In granular layer keratinocytes, antimicrobial peptides (AMPs) may be stored, including S100A7, S100A8, S100A9, β-defensins, cathelicidin (CAMP/LL-37), and lipocalin 2 (LCN2). The nucleus is lost as granular keratinocytes transition to corneocytes, and a cross-linked protein membrane structure termed the cornified envelope is formed, between which many layers of neutral lipids are deposited. This produces an effective water-impermeable barrier. The epidermis contains Langerhans cells (LCs) that are immature antigen-presenting cells, and the dermis contains resident myeloid dendritic cells (DCs). Although there are nonrecirculating cutaneous lymphocyte antigen (CLA)+ resident memory T cells (Trm cells) in the skin, keratinocytes constitutively synthesize CCL27 (CTACK), which is the major chemokine that attracts CCR10+ CLA+ skin-homing T cells into noninflamed skin for immune surveillance. These components maintain steady-state cutaneous immunity or, effectively, a state of tolerance. (b) The epidermis can also participate in innate or adaptive immune responses to triggers such as injury, infection, or cytokine stimulation. Keratinocytes may ① proliferate in response to cytokines such as IL-22 to accelerate loss of surface keratinocytes and eliminate pathogens, ② increase synthesis of innate effector molecules such as AMPs, and ③ direct migration of new T cell subsets and other immune effector cells into the skin through production of chemokines. (Additional abbreviations used in figure: IFN-α, interferon-α; TNF, tumor necrosis factor; TSLP, thymic stromal lymphopoietin; T17, IL-17-producing CD4+ and CD8+ T cells; Th, T helper cells.)