Figure 2.
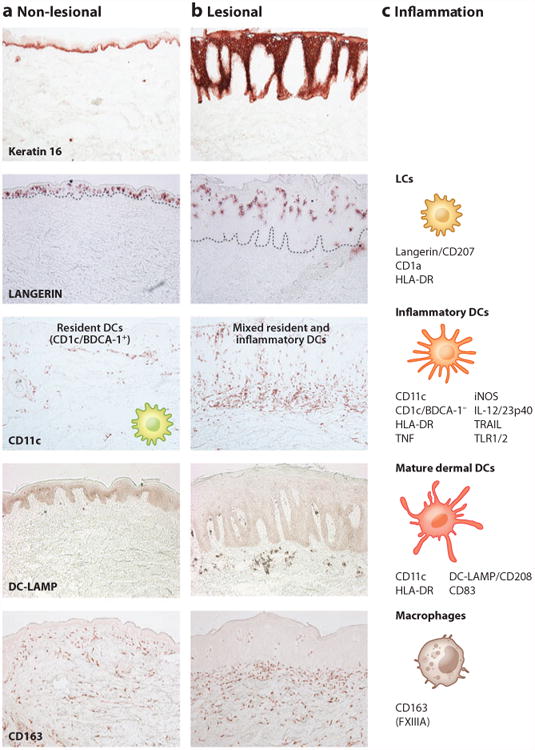
Immune cellular components of normal-appearing and inflamed psoriatic skin. Representative immunohistochemistry of (a) normal-appearing, nonlesional skin of psoriasis patients and (b) lesional psoriasis skin is shown, as is (c) a diagram of immune cellular components and their surface receptors during inflammation. Keratin 16 stains basal epidermis in nonlesional skin but stains full thickness epidermis in psoriasis. Langerin/CD207+ Langerhans cells (LCs) are found scattered in the lower epidermis in nonlesional skin and are found higher up in the thicker epidermis of psoriasis lesions. LCs are also identified by CD1a and HLA-DR. CD11c+ BDCA-1+ resident myeloid dendritic cells (DCs) are found in the upper dermis in nonlesional skin. During psoriatic inflammation, numbers of CD11c+ inflammatory DCs that are CD1c/BDCA-1− increase in the epidermis and dermis. These cells also express HLA-DR, TNF, iNOS, IL-12/23p40, TRAIL, and TLR1/2. Resident DCs are stable in number between nonlesional and lesional skin and are both CD11c+ and BDCA-1+. However, resident myeloid dermal DCs become more mature in psoriasis, as evidenced by expression of DC-LAMP/CD208. CD163+ macrophages are scattered throughout the dermis in nonlesional skin and increased approximately twofold in lesional skin. These CD163 + cells are also FXIIIA+, although CD163 is preferred as a marker. All images are 10 × magnification. (Additional abbreviations used in figure: BDCA, blood dendritic cell antigen; DC-LAMP, DC-lysosome-associated membrane protein; iNOS, inducible nitric oxide synthase; TLR, Toll-like receptor; TNF, tumor necrosis factor; TRAIL, tumor necrosis factor–related apoptosis-inducing ligand.)
