Abstract
Background:
Mothers play a key role as transmitters of oral health behavior for their children. Hence increasing their knowledge about positive attitude toward desirable oral health behaviors regarding their children will lead to the better oral health of the children.
Aim:
The aim was to evaluate the effectiveness of oral health education program among mothers with 6-18 months old children in the prevention of early childhood caries.
Materials and Methods:
A total of 480 mothers with 6-18 months old children were selected using cluster randomization of the primary health center. The allocated mothers were assigned into three groups: Motivation group (group A), traditional health education group (group B) and control group (group C). Clinical examination was carried out to record the dental decay of the child.
Statistical Analysis:
The data was analyzed using SPSS 13. Evaluation of statistical significance between groups was made using the Chi-square test, ANOVA and Kruskal-Wallis.
Results:
Mean number of decayed teeth was 0.23 + 0.58 in group A that was significantly less as compared to 0.39 + 0.79 and 1.17 + 1.32 in group B and C, respectively.
Conclusion:
Motivational intervention was more effective in reducing dental decay in the children as compared to the other two groups.
Keywords: Dental health education, mothers, motivation, nursing bottle caries, prevention of early childhood caries, programs
Introduction
Views about dental caries have changed in this generation; caries is now viewed as a process, not the outcome.[1] Caries in the infants and the young children has been recognized as a clinical syndrome, which was described in the first decades of the last century.
Early childhood caries (ECC) remains a sizeable and significant public health problem in developing countries and among individuals with lower socioeconomic group. The parents of these high-risk children often wait until caries in primary teeth is advanced and become symptomatic before bringing their children to the dentist. Treatment at that time is invasive, and parents tend to avoid subsequent treatment until their children's needs again become extreme.[1]
The most common approach in caries prevention is educating the parents, however, traditional health education may be insufficient to change parents’ behavior in relation to their high-risk children, as parents do not go to health professionals in a state of readiness to change patterns of behavior that are well established.[1]
Motivational interviewing (MI) is more focused and goal-directed.[2] MI approach, which has been used in many different settings, relies on a brief empathic counseling session where the client is helped to explore and verbalize the reasons for changing the health behavior and to find the reasons for changing themselves.[3] Applying the MI counseling approach helps uncover motivation and provides strategies to move patients from inaction to action and attempts to create an atmosphere in which the person can explore problems safely and face difficulty with realities.[1]
Hence, this study was undertaken with the aim to compare the two approaches, which include MI and traditional health education to prevent ECC in 6-18 months old children.
Materials and Methods
A parallel double-blind randomized intervention study was carried out after obtaining the ethical clearance from The Oxford College, Hospital and Research Center. The sample size was estimated on the basis of the following formula: N = Z2 pq/∆2, where Z = 1.96, P = 0.5, q = 1 - p and delta = margin of error, that is, 0.05. The appropriate sample size required for the study is 384. Estimating a drop out of 15-20% 480 sample size was determined.
A pilot study was undertaken on 10% of the study population. It served as a preliminary study to identify any organizational and technical problems. The face validity of the questionnaire was assessed through a bilingual expert and by distributing it among the mothers. Cronbachs α =0.75 showed acceptable internal consistency of the questionnaire.
The calibration of the examiner was done by examining and recording the findings using a self-designed proforma. The kappa co-efficient value for intra-examiner reliability with the respect to the caries index (0.75) was good.
The primary health centers in South Bangalore city were selected using simple random sampling and permission to carry out the study was taken from the District Health and Family welfare officer (Bangalore Nagar Zillah, E.D. Hospital) and the medical officer of the concerned primary health center. Total of 480 mothers who gave the consent and having 6-18 months old infants with healthy teeth were included in the study. Mothers of children with serious acute or chronic health condition that would disallow their full participation were excluded from the study.
The cohort of mothers was divided into three equal groups (160 each) by randomly assigning the health centers into the three groups of motivational (group A), educational (group B) and control group (group C). The block randomization was supervised by a dentist who was not involved in the clinical examination and interviews.
Information regarding the demographic backgrounds, feeding habits, oral hygiene practices was collected from all the mothers using a pretested structured proforma. After which 160 mothers each in group A and group B were educated through power point presentation and pamphlets, which laid emphasis on the importance of primary dentition, feeding and dietary habits, hygiene related to food preparation, oral hygiene practices and transmission and acquisition of oral bacteria. In group A reinforcement through two brief phone calls were made during the period of preparation for a change and while the change was occurring (at 2 weeks and 1 month after initial contact). They were called 2 times to the primary health center to reinforce change, solve any problem and to promote the maintenance of behavior change but if they failed to turn up home visits were made.
After 8 months, all the three groups were called to the primary health centers, and clinical examination of childs’ dentition was carried out as per the criteria and codes for caries by WHO + initial lesion,[4] by the examiner, who was not aware of the interventions. Unaware of these interventions mothers were again given questionnaire for assessing the changes in the dietary and oral hygiene habits. After the completion of the study mothers in group C also received education on caries prevention.
Statistical analysis
The data were analyzed by SPSS 13 (Statistical package for the social sciences for window version 13, SPSS Inc, Chicago, IL, U.S.A.) Evaluation of statistical significance between groups was made using the Chi-square test, ANOVA and Kruskal-Wallis test.
Results
From January 2009 to October 2009, 480 participants (160 in each group) were recruited. After 8 months of follow-up 387 children's were examined for caries (137 in group A, 128 in group B and 122 in group C). Comparison of the child's age revealed no statistically significant difference in the age distribution of all the three groups, (P = 0.373) at pre and post intervention [Table 1]. In all the three groups, there was male child predominance. Most of the mothers had primary education in all the three groups [Figure 1]. Statistically significant difference was seen among three groups with respect to socioeconomic status of the family [Figure 2].
Table 1.
Distribution of the subjects according to the age of the children
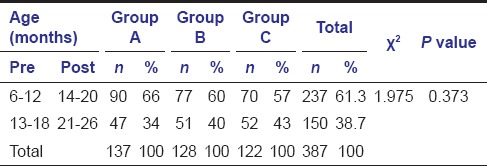
Figure 1.
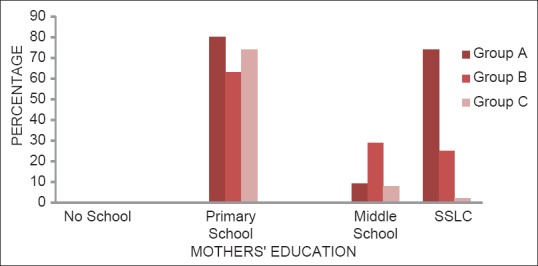
Distribution of the subjects according to mothers’ education
Figure 2.
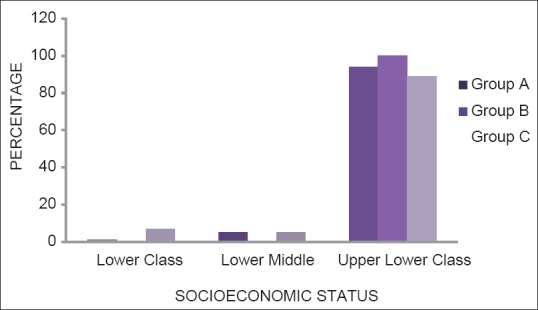
Distribution of the subjects according to the family's socioeconomic status
On comparing the feeding habits before and after, there was statistically significant difference within the groups [Table 2].
Table 2.
Distribution of the subjects according to the feeding habits in comparison to pre- and post-intervention within each group
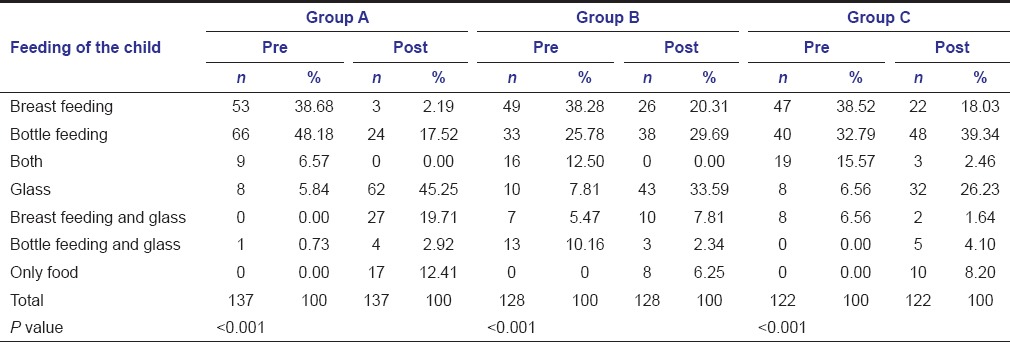
In group A and B bottle feeding at demand drastically decreased from 48.91% and 39.84% at baseline to 13.14% and 17.19% respectively at the end of the study. Whereas in group C, it was seen that there was a decrease in demand feeding of breast milk (63.11% vs. 18.03%) and increase in bottle feeding at demand (30.33% vs. 36.89%).
At the start of the study 7.30%, 11.72% and 10.66% of the mothers in group A, B and C respectively used other comforting practices to make their children sleep at night without giving any feed to them which increased to 56.93%, 33.59% and 36.07% mothers, respectively. Night feeding through bottle decreased in group A and B, but no decrease was observed in group C. Association within each group was statistically significant (P < 0.001).
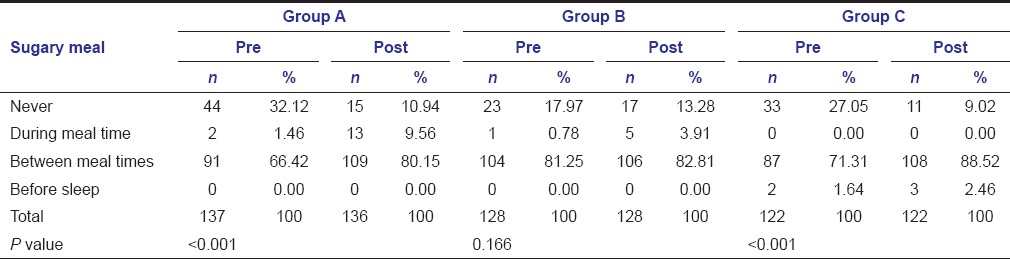
The consumption of sugary item between meals increased from 66.42% to 80.15% in group A and consuming sweet items in group C also increased from 71.31% to 88.52%. Thus, statistically significant association was observed within these two groups [Table 3].
Table 3.
Distribution of the subjects according to the time interval of sugar items-in comparison to pre- and post-intervention within each group
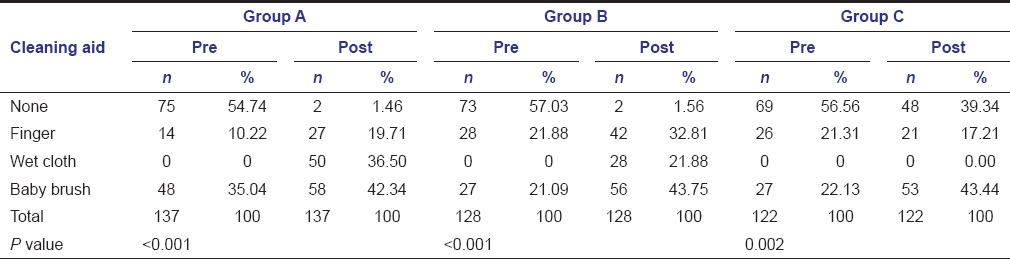
At baseline 48 (35.04%) of mothers in group A and 27 (21.09%) mothers in other two groups used tooth brush for cleaning child's teeth which is lower than 58 (42.34%) mothers in group A and 56 (43.75%) and 53 (43.44%) of mothers in group B and C at the end of the study. The difference was statistically significant [Table 4].
Table 4.
Distribution of the mothers according to the aid used for cleaning child's teeth-in comparison to pre- and post-intervention within each group
Mean number of decayed teeth in group A was 0.23 + 0.58 when compared to 0.39 + 0.79 and 1.17 + 1.32 in group B and C.
Around 7%, 15% and 25% of the subject in group A, B and C respectively required two or more surface filling. 8%, 9% and 30% of the subjects in group A, B and C respectively required preventive treatment.
Discussion
Since the 1960s, dentistry has become much more holistic and preventive in orientation. With increased awareness of the importance of interpersonal relationships, the integration of dental and general health, and improvement of self-care behaviors, the ability to maximize health seems tied to patients’ motivation. Health education does not appear to be sufficient. As a result of health professionals’ frequent failure in helping patients change their behavior, there is considerable frustration and skepticism among them regarding such attempts. MI may present an answer. It seek to “confront” clients with the reality, seeks to understand the person's frame of reference, particularly via reflective listening, expresses acceptance and affirmation, eliciting and selectively reinforcing the client's own self-motivational statements expressions of problem recognition, concern. It is a subtle balance of directive and client-centered components shaped by a guiding philosophy and understanding of what triggers change.[1]
In the present study, no statistical difference was seen between the age distribution of the subjects in all the three groups and also with a mean age of the children. This is in accordance to the study conducted by Kowash et al.[5] but not in accordance to the study conducted by Weinstein et al.[1] where control group had children belonging to older age group.
The present study showed male child predominance in all the group which was similar to the study conducted by Rong et al.,[6] but in contrast to the study conducted by Weinstein et al.[1] where there was no difference between the sexes in the two groups.
The dropout rate in the present study was 14.4% and 23.6% in group A and C respectively which was comparatively less than the study conducted by Rong et al.[6] where the dropout rate was 29% and 31% in the test and control group. These mothers could not be contacted during the post-intervention period due to change in their contact number and residential address.
Most of the mothers in the present study had only their primary education which is in accordance with the study conducted by Feldens et al.,[7] Vachirarojpisan et al.[8] and Kowash et al.[5] where the mothers were also less educated.
The present study showed a decrease in the breastfeeding on demand in all the three groups at the end of the study. But the increase in the bottle feeding on demand was seen in group C when compared to baseline. Decrease in the demand to feed through breast in all the groups can be attributed to the increasing age of the child. The education given on the harmful effect of the bottle feeding on demand might have been a reason for the decrease seen in the two groups (group A and B).
In the present study, 10.22% and 26.56% of the subjects in group A and B respectively continued to give bottle feed with milk at night when compared to 48.91% and 37.50% of the subjects who were bottle fed at baseline. There was a drastic reduction in the night feeding in the present study as compared to the study conducted by Vachirarojpisan et al.[8] where 43.7% (baseline) and 40.4% (follow-up) of the subjects were given bottles during the night.
In the present study, an increase in the intake of sugar item in between the meals was observed in all the three groups. This was similar to the findings observed by Holt et al.,[9] in his study where there was little difference in the three groups where the subjects regularly ate snacks in between meals. The intervention group in the present study showed a similar increasing trend of sugar intake in between meal, as it was observed in the study conducted by Vachirarojpisan et al.[8] Age might have played a role in decreased consumption of sweet items or drinks at baseline as parents were not likely to indulge their child in having sweet items at young age. No improvement in the intake of sweet drink or item was observed after 8 months follow-up which was also reported by Weber-Gasparoni et al.,[10] where mothers in both groups also did not significantly improve their children's consumption of sugared beverages between meals. This would be due to fact that sweet taste is a natural and primordial instinct of man.
In this study the children whose teeth were cleaned twice a day at baseline were 2.92%, 3.90% and 4.10% in group A, B and C as compared to 59.12%, 21.88% and 4.92% of children in groups A, B and C respectively at the end of the study. This is in contrast to the study conducted by Rong et al.[6] where 87.6%, 69.0% in the test group and control used to brush their teeth twice a day at the end of the study.
In the present study, health education has played a role in increasing the number of parents cleaning child's teeth, and use of appropriate aids whereas MI along with the above two variables has improved the practice and frequency of cleaning child's teeth, rinsing the child's mouth after feeding and use of nonfluoridated toothpaste. The use of nonfluoridated toothpaste in the present study was in contrast to the study conducted by Sgan-Cohen et al.,[11] Vachirarojpisan et al.,[8] and Weber-Gasparoni et al.[10] where mothers used fluoridated toothpaste to clean their child's teeth. This may be because the mothers here were advised not to use fluoridated tooth paste till the children were 6 years old.
About 7%, 10% and 30% of children in group A, B and C respectively had white spot lesion on the teeth. In group C subjects having, decayed teeth was 23% compared to 9% and 14% in group A and B respectively. This might be due to the fact that group C showed poorer feeding and oral hygiene practices along with high frequency of sugary intake.
The mean decayed, missing, and filled teeth (dmft) of the subjects in present study in group A, B and C was 0.23 + 0.58, 0.39 + 0.79 and 1.17 + 1.32 respectively. These findings are similar to findings by Davies et al.[12] Fracasso Mde et al.[13] and Wagner et al.[14] where mean dmft was less in the test group compared to the control group. The study conducted by Harrison et al.[15] also showed that prevalence of treated and untreated caries at the d2 level was 76% in controls versus 65% in tests.
The subjects who required one-surface filling was 3% in group C, 7%, 15% and 25% of the subjects in group A, B and C respectively needed two or more surface filling. Preventive care was required by 8%, 9% and 30% of the subject in group A, B and C respectively. The treatment demand in the group A and B in spite of education might be due to lack of dental visit of the child as the mothers in the family were dependent on the male members for the dental visits.
The variation in the responses might have been due to the difference in socioeconomic status, education of both parents in the three groups, which was comparatively better in group B; this might have played a role in better parenting practices along with traditional health education. The problem in validating responses to survey due to the potential bias caused by patients’ desire to satisfy the health care providers by providing answers they believe the providers expect to hear must be given its due consideration.
Conclusion
Motivational interviewing and traditional health education both brought about changes in the dietary factors and oral hygiene practices, MI was an effective mode to bring about the changes as it aimed to interact with the mothers and solve their problems at the appropriate time to promote adoption of helpful feeding and tooth care behaviors in their family, but this could not control the sugar intake of the children. Further research should be carried to estimate the cost-effectiveness of the intervention and to check whether the benefits are maintained up to school age.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Weinstein P, Harrison R, Benton T. Motivating parents to prevent caries in their young children: One-year findings. J Am Dent Assoc. 2004;135:731–8. doi: 10.14219/jada.archive.2004.0299. [DOI] [PubMed] [Google Scholar]
- 2. [Last accessed on 2010 Nov 12]. Available from: http://www.motivationalinterview.org/clinical/whatismi.html .
- 3.Arrow P, Raheb J, Miller M. Brief oral health promotion intervention among parents of young children to reduce early childhood dental decay. BMC Public Health. 2013;13:245. doi: 10.1186/1471-2458-13-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kassawara AB, Assaf AV, Meneghim Mde C, Pereira AC, Topping G, Levin K, et al. Comparison of epidemiological evaluations under different caries diagnostic thresholds. Oral Health Prev Dent. 2007;5:137–44. [PubMed] [Google Scholar]
- 5.Kowash MB, Pinfield A, Smith J, Curzon ME. Effectiveness on oral health of a long-term health education programme for mothers with young children. Br Dent J. 2000;188:201–5. doi: 10.1038/sj.bdj.4800431. [DOI] [PubMed] [Google Scholar]
- 6.Rong WS, Bian JY, Wang WJ, Wang JD. Effectiveness of an oral health education and caries prevention program in kindergartens in China. Community Dent Oral Epidemiol. 2003;31:412–6. doi: 10.1046/j.1600-0528.2003.00040.x. [DOI] [PubMed] [Google Scholar]
- 7.Feldens CA, Vítolo MR, Drachler Mde L. A randomized trial of the effectiveness of home visits in preventing early childhood caries. Community Dent Oral Epidemiol. 2007;35:215–23. doi: 10.1111/j.1600-0528.2006.00337.x. [DOI] [PubMed] [Google Scholar]
- 8.Vachirarojpisan T, Shinada K, Kawaguchi Y. The process and outcome of a programme for preventing early childhood caries in Thailand. Community Dent Health. 2005;22:253–9. [PubMed] [Google Scholar]
- 9.Holt RD, Winter GB, Fox B, Askew R. Effects of dental health education for mothers with young children in London. Community Dent Oral Epidemiol. 1985;13:148–51. doi: 10.1111/j.1600-0528.1985.tb00431.x. [DOI] [PubMed] [Google Scholar]
- 10.Weber-Gasparoni K, Warren JJ, Reeve J, Drake DR, Kramer KW, Marshall TA, et al. An effective psychoeducational intervention for early childhood caries prevention: Part II. Pediatr Dent. 2013;35:247–51. [PMC free article] [PubMed] [Google Scholar]
- 11.Sgan-Cohen HD, Mansbach IK, Haver D, Gofin R. Community-oriented oral health promotion for infants in Jerusalem: Evaluation of a program trial. J Public Health Dent. 2001;61:107–13. doi: 10.1111/j.1752-7325.2001.tb03374.x. [DOI] [PubMed] [Google Scholar]
- 12.Davies GM, Duxbury JT, Boothman NJ, Davies RM, Blinkhorn AS. A staged intervention dental health promotion programme to reduce early childhood caries. Community Dent Health. 2005;22:118–22. [PubMed] [Google Scholar]
- 13.Fracasso Mde L, Rios D, Provenzano MG, Goya S. Efficacy of an oral health promotion program for infants in the public sector. J Appl Oral Sci. 2005;13:372–6. doi: 10.1590/s1678-77572005000400011. [DOI] [PubMed] [Google Scholar]
- 14.Wagner Y, Greiner S, Heinrich-Weltzien R. Evaluation of an oral health promotion program at the time of birth on dental caries in 5-year-old children in Vorarlberg, Austria. Community Dent Oral Epidemiol. 2014;42:160–9. doi: 10.1111/cdoe.12072. [DOI] [PubMed] [Google Scholar]
- 15.Harrison RL, Veronneau J, Leroux B. Effectiveness of maternal counseling in reducing caries in Cree children. J Dent Res. 2012;91:1032–7. doi: 10.1177/0022034512459758. [DOI] [PubMed] [Google Scholar]


