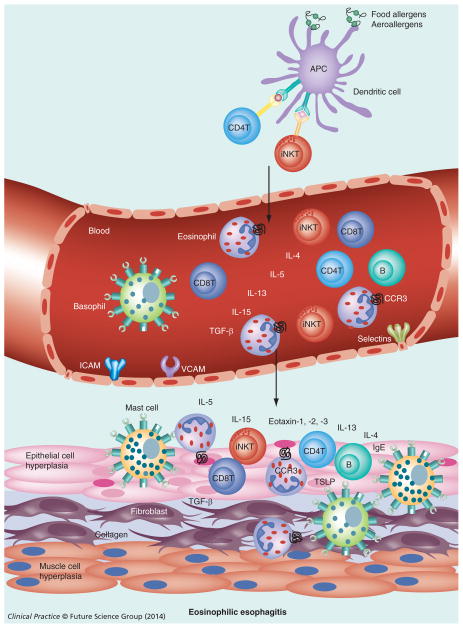
Figure 1. Allergen-induced esophageal eosinophilic esophagitis.
APCs process the allergens (food allergens/aeroallergens) and present antigens to T cells (iNKT cells in eosinophilic esophagitis, CD4 T cells in case of other allergic diseases). These T cells home to the esophagus via blood circulation and upon activation release Th2 cytokines (IL-4, IL-13 and IL-5) that induce IL-15 and eotaxin in the esophageal epithelium that attracts eosinophils into the epithelium (≥15 eosinophils/high-powered field).
Additionally, in response to allergens, iNKT cells, CD4+ T cells, CD8+ T cells, B cells, mast cells and basophils are also recruited to the esophagus. B cells synthesize IgE locally or systemically that may activate mast cells and basophils. Basophils and TSLP also contributes to EoE pathogenesis independently of IgE. Activated eosinophils and mast cells secrete TGF-β and other factors that induce esophageal remodeling, including fibrosis, collagen accumulation, muscle cell hyperplasia and epithelial cell hyperplasia that finally cause esophageal dysfunction and lead to eosinophilic esophagitis.
APC: Antigen-presenting cell; iNKT: Invariant natural killer T cell; TSLP: Thymic stromal lymphopoietin.