Abstract
Background
Determining the costs of healthcare delivery is a key step for providing efficient nutrition-based care. This analysis tabulates the costs of delivering home parenteral nutrition (HPN) interventions and clinical assessments through encrypted mobile technologies to increase patients’ access to healthcare providers, reduce their travel expenses, and allow early detection of infection and other complications.
Methods
A traditional cost-accounting method was used to tabulate all expenses related to mobile distance HPN clinic appointments, including (1) personnel time of multidisciplinary healthcare professionals, (2) supply of HPN intervention materials, and (3) equipment, connection, and delivery expenses.
Results
A total of 20 mobile distance clinic appointments were conducted for an average of 56 minutes each with 45 patients who required HPN infusion care. The initial setup costs included mobile tablet devices, 4G data plans, and personnel's time as well as intervention materials. The initial costs were on average $916.64 per patient, while the follow-up clinic appointments required $361.63 a month, with these costs continuing to decline as the equipment was used by multiple patients more frequently over time. Patients reported high levels of satisfaction with cost savings in travel expenses and rated the quality of care comparable to traditional in-person examinations.
Conclusion
This study provides important aspects of the initial cost tabulation for visual assessment for HPN appointments. These findings will be used to generate a decision algorithm for scheduling mobile distance clinic appointments intermittent with in-person visits to determine how to lower costs of nutrition assessments. To maximize the cost benefits, clinical trials must continue to collect clinical outcomes.
Keywords: parenteral nutrition, nutrition, home nutrition support, reimbursement, outcomes research/quality, nutrition support practice
Introduction
A distance care delivery mode is being investigated to improve how to increase patient access to healthcare professionals, detect nutrition and infusion concerns as early as possible, and reduce costs and travel to specialist appointments at a distance.1-3 Telehealth and telecare are well established for medical consultation, health assessment and monitoring, and homecare management at a distance.2,4-6 Mobile health (mHealth) is “the delivery of healthcare services via mobile communication devices.”7 mHealth clinics might be most advantageous to healthcare providers and their patients requiring home parenteral nutrition (HPN) infusion care. mHealth is expected to reduce medical expenditures in HPN infusion care,8,9 as patients are able to have communication, consultation, and HPN education in their home environments.1-3
mHealth has advantages of encrypted connectivity from multiple and various locations, including healthcare professionals’ offices, patients’ homes, and patients’ out-of-town vacation locations. mHealth allows patients and family members to interact with healthcare providers without travel and receive visual assessments for detecting potential infections, nutrition depletion symptoms, and other costly and serious complications of their HPN infusion care.3,10,11
National data have also shown that the annual reimbursement for HPN-related health services across clinical settings varies and costs approximately $2.3 billion across the United States.6,12,13 Based on Medicare and Medicaid reports, reimbursement per patient receiving direct care from healthcare professionals annually ranges from $100,000–$250,000, with the addition of $75,000–$122,000 to purchase supplies and daily HPN infusion solutions.14,15 Notably, HPN patients report nonreimbursed healthcare expenditures of $4716 yearly.16 HPN-related clinic visits include, on average, 36 annually with a variety of health-care professionals. In addition, Medicare patients spend a 20% copay for traditional in-person clinic visits.12,16,17
With these facts in mind, cost savings are a key issue in the HPN population receiving this very expensive area of medical care. mHealth is considered a promising alternative or supplement to integrate with traditional in-person clinic visits so that patients can receive timely care and diagnoses from healthcare providers at a distance.2,18
Base costs of delivering mHealth HPN interventions by healthcare providers at a distance should be identified for further investigation of cost-effectiveness studies. Thus, the purpose of this analysis was to determine the costs of implementing mobile distance clinic appointments for initial and follow-up appointments when using mobile tablets and interactive encrypted videoconferencing. A traditional costing accounting method was used to estimate costs.
Materials and Methods
Mobile Distance Clinic Appointments for HPN Care Delivery
To date, 45 patients requiring long-term HPN infusion care for nonmalignant bowel disease participated in this study.11 A total of 20 mobile distance clinic appointments were conducted with an average of 56 minutes each. In this study, the modes of delivering a mobile distance clinic appointment included (1) mobile tablets with an unlimited data plan, (2) video teleconferencing program software, (3) an encryption equipment program for Health Insurance Portability and Accountability Act (HIPAA) security, and (4) encrypted email accounts and firewalled websites.
During the mobile distance clinic appointments, multiple multidisciplinary professionals provided a series of HPN educational interventions regarding (1) problem-solving HPN infusion care, (2) infection and depression prevention, (3) fatigue reduction, and (4) peer and family support. In addition, patients were individually assessed through a medical history report and clinical examination, including visual assessment. Healthcare professionals assessed patients’ general health and nutrition status and symptoms of current illness by asking structured medical history questions. A subsequent visual physical assessment and observations were completed using real-time video and photos of the patient's HPN infusion catheter site, abdominal wounds, fistulas, ostomy output container, and abdominal scars.11 The mobile tablets had an Internet connection to the Oley Foundation for HPN care and the National Caregiving Alliance and other family caregiving resources.
Considerations for Implementing a Mobile Tablet Appointment
When considering a mobile device, the multidisciplinary research team, including the telehealth center director and a telehealth system coordinator, compared several types of mobile tablets and their features, including pixels/resolution, speed, size, and weight, as well as cost. In addition, the proposed use with HPN patients was determined. Overall, in this study, a mobile tablet was to (1) have a high-resolution screen for increasing visualization of the patient's HPN infusion catheter site, abdominal wounds, fistulas, ostomy output container, and abdominal scars and (2) be easy to carry and operate. Our selected mobile tablet device, the iPad mini, was the only device available at the time that allowed both ease of use and the highest resolution on a small screen.
We provided 4G unlimited data plans to standardize the Internet connection using the medical center–contract provider. This standardized provision of the 4G data plan has several advantages: (1) the medical center 4G data plan costs are less expensive than personal plans, (2) our mobile distance clinic appointment can be available anywhere regardless of their locations, and (3) the HPN patient will not be restricted to one environment with limited connectivity. The 4G data plan has advantages over using home Wi-Fi. First, all eligible HPN patients can be included in this study because we did not exclude anyone without an Internet connection. Second, study participants were less likely to experience technical challenges during videoconferencing through multiple Wi-Fi systems with different configuration and firewalls.
The clinic visit protocol was tested within the week prior to the scheduled visit. A few Internet disconnections were resolved with the troubleshooting assistance of a telehealth system coordinator. However, this was a very rare event because we provided a 4G unlimited data plan. These advantages are critically important for HPN clinical trials for increasing the generalizability of our findings in considering persons with lower social economic status, computer skills, and technology use.19
Study participants were not required to provide a deposit for obtaining the mobile tablet. Instead, they needed to sign a mobile tablet loan and user agreement form, which was developed by the telemedicine team on campus and was approved by the university human subjects committee and our university legal department. The loan agreement includes information about “what is responsible mobile tablet use,” including (1) not storing health data related to this study, (2) not storing personal information such as Social Security numbers or credit card information, and (3) not obtaining illegal downloaded materials. We did not “lock down” the mobile tablet but allowed participants to download software and add apps. However, our agreement clearly states the user must be mindful of the Internet connection and should “beware of giving personal information out online.” In addition, it states that researchers should “follow standard security measures related to the mobile tablet using code numbers and no names.”
Health data related to this study or personal information were collected only through an encrypted connection. Primary communication with identifiable information occurred through 2 encrypted university systems: (1) the telemedicine bridge hosting videoconferencing software program for group clinic appointments and (2) a research electronic data capture web-based application for data collection/exchange.
Cost Analysis Method
This descriptive cost analysis was conducted using a traditional cost-accounting method that tabulates the expenditure data of intervention materials, health professionals’ time, and equipment about the mobile tablet and connection software.20,21 Traditional tabulation lists the actual cost spending in a spreadsheet. This method has advantages in showing how costs are allocated to generate actual production. It is the first necessary process to enhance further complex analysis of the specific content of a cost of production report.21 The costs of materials and labor were categorized directly into the products of (1) intervention materials and (2) implementing the health-care service assessments and interventions through mobile tablets and interactive encrypted videoconferencing (see the equation below).
Amortization with multiple cases would occur as equipment has been used by different patients over time. In accounting, amortization refers to expensing the acquisition costs minus the residual value of equipment and any intangible assets.21,22 Amortization is a systematic approach to estimate useful economic life of equipment and to reflect total consumption, expiry, obsolescence, or other decline in value as a result of repeated use or the passage over time.22
Data Collection
Costs for the setup stage were based on (1) costs of mobile tablet equipment, (2) connection fees for monthly data plans, (3) costs of shipping the tablets, (4) photocopying educational handouts, and (5) delivering intervention materials. The clinic appointments and the digital version of the intervention materials were provided via mobile tablets with an unlimited 4G data plan for a wireless Internet connection. Relevant accessories included a protective cover, a screen-protecting film, and device warranty. Few materials were consumed for the intervention, including copying, printing, and mailing intervention materials. Encryption equipment was used to ensure HIPAA privacy during the mobile distance clinic appointments. Supply costs for each specific activity were documented with an expenditure log and invoices that a project manager recorded whenever the cost occurred. Costs for the implementation stage were based on the time spent by a health counselor, an advanced practice psychiatric nurse specialist, and a telemedicine and tele-health system coordinator involved in setting up the mobile distance clinic appointments. All personnel costs were based on their hourly wages reflecting the hours spent on each mobile distance clinic appointment.23-25 The time spent by the interventionists was recorded for each mobile distance clinic appointment using time logs (see details in Table 1).
Table 1.
Cost per Patient for 1 Mobile Distance Home Parenteral Nutrition Clinic Appointment.
| Categories | Items | Detailed Description | Cost per Unit | Unit | Subtotal Cost per Item | Subtotal Cost by Category | Included in Fixed Cost | Included in Maintenance Cost |
|---|---|---|---|---|---|---|---|---|
| Equipment cost | Mobile tablet | $329 | 1 | $329 | $590.62 | X | ||
| Mobile tablet protective covers | $27 | 1 | $27 | X | ||||
| Mobile tablet screen protecting film | $7.95 | 1 | $7.95 | X | ||||
| Videoconference program software | $100 | 1 | $100 | X | ||||
| Encryption equipment | Assured HIPAA privacy | $126.67 | 1 | $126.67 | X | |||
| Supply costs | Monthly data plan for Internet connection | As negotiated by University Center for Telehealth and Telemedicine | $40.81 | 1 | $40.81 | $82.18 | X | |
| Mobile tablet warranty | Monthly cost is $4.15, calculated from total $99 per device for 2-year warranty | $4.15 | 1 | $4.15 | X | |||
| Booklets for device training guide and intervention | Requiring paper, printing, and binding for | $19.21 | 1 | $37.22 | X | |||
| (1) Intervention | $17.93 | 1 | ||||||
| (2) Mobile tablet training guide booklet | $0.08 | 1 | ||||||
| (3) Manila envelope | ||||||||
| Delivery costs | Delivery protective box | Delivering mobile tablet device and booklets | $8.72 | 1 | $8.72 | $53.84 | X | |
| Shipping cost | Ranging from $17.21–$25.83 depending on delivery region | $22.56 | 2 | $45.12 | X | |||
| Personnel cost | Interventionist 1 | Health counselor | $70/h | 1 | $70 | $190 | X | |
| Interventionist 2 | Psychiatric nurse specialist | $70/h | 1 | $70 | X | |||
| Technician | Telehealth system coordinator | $50/h | 1 | $50 | X | |||
| Total cost | $916.64 |
HIPAA, Health Insurance Portability and Accountability Act.
Ethical Considerations
The study was approved by the human subjects committee of our institution. Written informed consents were obtained for all study participants.
Results
Total Cost Estimates
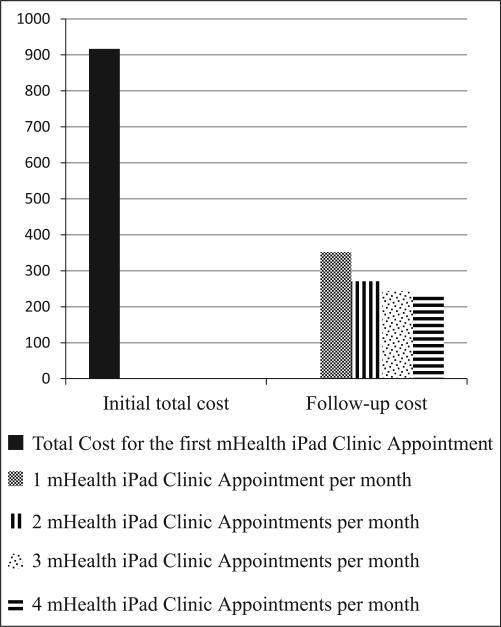
The total cost of $916.64 was spent to set up the initial mobile distance clinic appointment, providing multidisciplinary HPN infusion care interventions, history taking, and a visual assessment for 1 patient (see Figure 1). A total of 60.55% in total costs ($555.01) was spent as the fixed cost, which was required regardless of the number of clinic appointments or time spent (see details in Table 1).
Figure 1.
Results of cost equation.
The total equipment cost of the intervention was $590.62. Most of the cost was spent for purchasing a set of devices ($463.95) for one-time purchase of mobile tablets, device protection accessories, and videoconferencing software. To ensure HIPAA privacy, encryption equipment was purchased ($30,000) specifically for the mobile tablet. Cost amortization over multiple cases was applied to determine a per-use equipment charge.22 Three amortized mobile distance clinic appointments with 1 patient required $380 for encryption; thus, per-visit cost for encryption was $126.67. This cost is similar to the expense found in a previous study for patients who received 1 in-person specialty care visit.16
The supply costs spent were $82.18 for the Internet connection, device maintenance, and interventional materials, including (1) $40.81 for the data plan for the Internet connection, (2) $4.15 for the monthly fee for the device protection warranty, and (3) $37.22 for 2 hard-copy intervention booklets requiring paper, printing, and binding. These 2 booklets provided information about the device training guide and HPN infusion care. Delivery fees were, on average, $53.84, although the care delivery cost varied depending on delivery regions (range, $43.14–$60.38).
Each mobile distance clinic appointment took an average of 56 minutes (approximately 1 hour). The personnel costs for 2 interventionists and 1 telehealth system coordinator were $190 per hour for providing a mobile distance clinic appointment. These costs align with reimbursement of actual clinical in-person appointments; one of the interventionists was a nurse practitioner who has her own national provider identifier number required for billing and insurer reimbursement.
Per-Session Cost
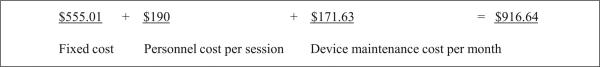
While $916.64 was required for having the initial mobile distance clinic appointment, the cost of the follow-up appointment decreased to $361.63 a month. Since the second mobile distance clinic appointment, personnel cost per session and device maintenance cost per month were required. This cost per session would decrease based on the frequency of repeated clinic appointments using the same equipment. As with in-person visits, it is likely that these distance appointments will become less lengthy across time, thus decreasing personnel costs. Thus, it is estimated that patients requiring HPN infusion care could cost $351.63 for 1 mobile distance clinic appointment a month, $270.82 for 2 mobile distance clinic appointments a month, $243.88 for 3 mobile distance clinic appointments a month, and $230.41 for 4 mobile distance clinic appointments a month (see Figure 2).
Figure 2.
Cost tabulation of initial setup and follow-up of mobile distance clinic appointments (unit: U.S. dollar).
Discussion
Overall Patient Rating of Mobile Distance Clinic Appointments
To date in this study, patients have expressed high levels of satisfaction with the interventions and care delivery using the mobile tablet. For example, patients stated, “I can hear fine,” “It is very convenient,” “The quality of care is similar to an in-person clinic visit and these are highly satisfying,” “Nurses are able to understand me well,” and “I can talk openly about my personal concerns.” Easier access to healthcare providers was reported as beneficial, such as, “I do not have to leave my vacation or college.”
Overall Summary of Analysis of Findings
These cost findings were the foundation and the first step in conducting a full economic evaluation of this innovative program of mobile distance clinic appointments. The mobile distance clinic appointments, similar to in-person clinics, require a large total initial cost for setup and distribution of the device. In the maintenance phase, at least $351.63 is required for 1 monthly follow-up mobile distance clinic appointment. However, the costs would decrease when patients have more frequent mobile distance clinic appointments. Mobile distance clinic appointments could be more cost-effective when patients use mobile tablets for long-term care, frequent visits, and supportive peer interactions, while reducing long-distance trips to see their healthcare providers.6
Benefits Reducing Patients’ Expenses
Some emergency visits and even hospitalizations could be prevented by early symptom detection through mHealth care delivery. Patients with mHealth are able to report their symptoms at the onset, while healthcare providers are able to complete visual and auditory physical examinations to assess critical patient problems.6,18 For example, 1 patient in our current HPN clinical trial used a mobile tablet to send a photograph to his physician, who observed the early signs of HPN infusion site infection. Another patient in our HPN clinical trial saved a 60-mile round trip by sending photos of her urine 24-hour container for measuring her fluid balance. In addition, mHealth and mobile tablets were used in the following ways by patients in their HPN infusion care: (1) the mobile tablet camera to better see their infusion site during daily HPN care; (2) the mobile tablet web browser to connect to the Oley Foundation website; (3) applications (apps) to track supplies, medications, and urinary and ostomy fluids; (4) apps to monitor and record weekly laboratory values; (5) email to communicate with supportive peers; and (6) media players to watch educational videos or movies while waiting to see healthcare providers.
Opportunity Benefit
Saving cost, time, and travel makes mHealth an important care delivery mode.6 The mobile distance clinic appointments of this study were able to help patients save on expenses of in-person clinic visits such as transportation expenses and time conflicts with work schedules. It is difficult to quantify the benefit because this study is the only recent research on medically related travel expenses and relevant costs for those receiving HPN infusion care in the United States.26 This cost-benefit would also be maximized when patients with HPN infusion care live in rural areas, at a distance from their usual care providers or HPN care specialist, or are disabled and require special transportation services or assistance from family or others.2,6 Thus, satisfaction with reducing travel is an extra benefit from mHealth, although it does not generate actual revenue.1,13,27 Our analysis provides important cost information for clinicians, researchers, and policy makers.
Implications for Research
Compared with standard care, the clinical effectiveness of technological interventions for patient instruction, medical and dietary review, and general assessment has been verified, but few studies have reported information on costs of care delivery for HPN infusion.3,8,16 In the published literature on HPN infusion care, there is limited information about cost data and economic analyses from the patient's perspective or in the home setting vs acute care facilities.3,8,9 Thus, these cost findings of mobile clinic appointments are able to fill gaps in the literature, providing basic information on the costs required to implement mobile distance clinic appointments with multiple multidisciplinary professionals for patients requiring HPN infusion care.
Decisions regarding the selecting of a specific device should be based on thoughtful evaluation considering the purposes of the intervention, mobile and computer device characteristics, and cost.28 This decision is critically important as equipment costs directly influence the clinical efficacy of interventions and cost-effectiveness. Multidisciplinary collaboration with telehealth experts in selecting devices is crucial because mHealth technologies are one of the most rapidly changing in the field.29
Our traditional tabulated data provide the costs of the technology, allowing us to conduct further complex cost analysis when patient outcome data are completed. Further cost analysis will be conducted to investigate the cost-effectiveness of mobile distance clinical appointments compared with traditional in-person clinic visits at the end of study. Other cost analysis should consider facility costs, any reduction in clinical visits as needed, and cost savings from reduced travel.28 Any early identification of infection as well as any other significant comorbidity can be analyzed as clinical efficiency. Specifically, a geographic information system program30 will be used to generate travel distance data among patients’ homes, their primary care providers, and HPN specialists.
Implications for Clinical Practice
This study provides foundational information to formulate a clinical decision tree to decide cost-benefit when clinicians schedule cost-effectiveness HPN infusion care planning that integrates traditional in-person clinic visits and mobile distance clinic appointments.6,31 The mobile distance HPN clinic appointment is beneficial for providing critical and timely examination points for visualizing a wound, reviewing an intravenous (IV) or ostomy exit site, and assessing HPN technique at home. Also, vital signs and other measurements can be taken with peripheral finger sensors and other attachments to mobile tablets, although these will add equipment expense.
However, mobile assessment cannot replace in-person visits totally. Some clinical cases require traditional in-person clinic visits. For example, some IV sites cannot be fully assessed visually, such as infection exudate, swelling, and odors. In addition, laboratory abnormalities and prodromal symptoms can be missed, similar to in-person visits. Thus, we need to know how to mix 2 modes of care delivery to increase the cost-benefit ratio, considering how often and how long patients need to see care providers of HPN infusion care.4 Every patient lives in a different geographical region and has different conditions requiring clinic visits. Thus, travel costs are an important consideration in determining the costs vs benefits.6
A mobile distance clinic appointment consists of a series of HPN-related assessments, homecare education, communication, and consultation. Currently, International Classification of Diseases, Tenth Revision codes 99213 or 99214 have been used for obtaining reimbursement for outpatient clinic visits.32 Both the mobile distance clinic appointments and traditional in-person clinic visits require Medicare-certified nurse practitioners or medical physicians for reimbursement. This analysis can add economic data to the ongoing deliberations about regulations and reimbursement regarding mobile distance clinic appointments.
Implications for Healthcare Policy
Emerging mHealth and distance telehealth studies may demonstrate significant cost savings for health systems through reduced utilization of emergency departments and inpatient services.28 Such data would make it possible for policy makers and insurance payers to support the cost of distance care. As mobile devices become even more ubiquitous and standardized, health-care systems such as large medical centers, medical homes, and government health services may identify cost-effectiveness, efficacy, and enhanced engagement of patients through mHealth use. In addition, the satisfaction of patients and family members in combination with ongoing technology development will influence the accelerating use of mHealth use.33
Currently, it is early for third-party payers to consider reimbursement for implementation costs for an intervention. However, as in-home or clinical telehealth gains reimbursement by state and insures due to cost savings, this mHealth approach is likely to follow this recent trend in policy.34 Notably, 2013 private-sector investment of $678 million in mHealth development indicates the high expectations of use in medical homes, joint practices, and outpatient clinics.35 Expenses typically follow after a new approach, concept, or efficacy is empirically verified.18,28,29
Study Limitations
Two limitations were identified in this analysis. First, personnel time was based on the length of time for each mobile clinic appointment. However, some personnel time was not tabulated, such as the time for preparation for the visit or writing up the assessment results after visits. Personnel costs are one of the major components of the total cost (20.73%). Therefore, this personnel information should be included in future cost calculations.26 Second, there is the loss of equipment components. All mobile tablets loaned to the patients have been returned from our study participants. However, several accessories such as mobile tablet chargers and protective covers were not returned and needed to be replaced. Our further analysis will tabulate the cost for replacing missing equipment and supplies at the end of the clinical trial.
Conclusion
Distance connections use allows healthcare professionals to provide nutrition care interventions and assessments of long-distance HPN patients. This new approach using mobile distance clinic appointments has saved travel expenses for those who must travel long distance. This mobile care delivery aligns with future directions of healthcare and may minimize the needs for traditional in-person clinic visits for in-person examinations. Patients reported high levels of satisfaction with cost savings in travel expenses and rated the quality of care comparable to traditional in-person examinations.
Clinical Relevancy Statement.
Mobile distance clinic appointments can increase access to care and facilitate early detection of clinical problems in home parenteral nutrition (HPN) patients. Distance connections use allows for improvement in healthcare provision by uniting healthcare professionals with patients in overcoming distance barriers and by improving outpatient nutrition care, interventions, and assessments of HPN patients. This cost data of mobile care delivery system will affect healthcare policy and future nutrition care at home.
Acknowledgments
The authors extend their appreciation to all families who participated in this study for their time and participation in mobile healthcare interventions.
Financial disclosure: The project described was part of a larger study supported by the National Institute of Biomedical Imaging and Bioengineering (NIBIB), R01 EB015911, C. Smith, principal investigator. In addition, this study is partially supported by NIH/CTSA grant number UL1TR000001Trail Blazer award from University of Kansas Medical Center Frontiers: The Heartland Institute for Clinical and Translational Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Biomedical Imaging and Bioengineering or the National Institutes of Health. Financial support for the publication of the supplement in which this article appears was provided by Abbott Nutrition.
References
- 1.Chambers A, Hennessy E, Powell-Tuck J. Longitudinal trends in quality of life after starting home parenteral nutrition: a randomised controlled study of telemedicine. Clin Nutr. 2006;25(3):505–514. doi: 10.1016/j.clnu.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Saqui O, Chang A, McGonigle S, et al. Telehealth videoconferencing: improving home parenteral nutrition patient care to rural areas of Ontario, Canada. JPEN J Parenter Enteral Nutr. 2007;31(3):234–239. doi: 10.1177/0148607107031003234. [DOI] [PubMed] [Google Scholar]
- 3.Smith CE, Curtas S, Kleinbeck SV, et al. Clinical trial of interactive and videotaped educational interventions to reduce catheter-related infection, reactive depression, and rehospitalizations for sepsis in patients receiving home parenteral nutrition. JPEN J Parenter Enteral Nutr. 2003;27(2):137–145. doi: 10.1177/0148607103027002137. [DOI] [PubMed] [Google Scholar]
- 4.Yadrich DM, Fitzgerald SA, Werkowitch M, Smith CE. Creating patient and family education web sites: assuring accessibility and usability standards. Comput Inform Nutr. 2012;30(1):46–54. doi: 10.1097/NCN.0b013e3182343eac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fitzgerald SA, Yadrich DM, Werkowitch M, Piamjariyakul U, Smith CE. Creating patient and family education web sites: design and content of the home parenteral nutrition family caregivers web site. Comput Inform Nutr. 2011;29(11):637–645. doi: 10.1097/NCN.0b013e31822bef7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winkler M, Smith CE. Clinical, social, and economic impacts of home parenteral nutrition dependence in short bowel syndrome. JPEN J Parenter Enteral Nutr. 2014;38(1)(suppl):32S–37S. doi: 10.1177/0148607113517717. [DOI] [PubMed] [Google Scholar]
- 7.Torgan C. [May 20, 2014];The mHealth summit: local & global converge. 2009 http://www.caroltorgan.com/mhealth-summit/ Published November 6, 2009.
- 8.Doig GS, Chevrou-Severac H, Simpson F. Early enteral nutrition in critical illness: a full economic analysis using US costs. ClinicoEcon Outcomes Res. 2013;5:429–436. doi: 10.2147/CEOR.S50722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simpson F, Doig GS. Parenteral vs enteral nutrition in the critically ill patient: a meta-analysis of trials using the intention to treat principle. Intensive Care Med. 2005;31(1):12–23. doi: 10.1007/s00134-004-2511-2. [DOI] [PubMed] [Google Scholar]
- 10.Gilroy R. Presented at: Clinical Nutrition Week. Savannah, GA: Jan 18-21, 2014. iPad mHealth approach to the clinical management of the HPN patient population. [Google Scholar]
- 11.O'Hanrahan T, Irving MH. The role of home parenteral nutrition in the management of intestinal failure: report of 400 cases. Clin Nutr. 1992;11(6):331–336. doi: 10.1016/0261-5614(92)90083-3. [DOI] [PubMed] [Google Scholar]
- 12.Kelly DG. The clinician's responsibility for the consumer's financial well-being. Nutr Clin Pract. 2006;21(6):539–541. doi: 10.1177/0115426506021006539. [DOI] [PubMed] [Google Scholar]
- 13.Detsky A, McLaughlin JR, Abrams HB, Whitwell J, L'Abbe K, Jeejeebhoy KN. A cost-utility analysis of the home parenteral nutrition program at Toronto general hospital 1970-1982. JPEN J Parenter Enteral Nutr. 1986;10(1):49–57. doi: 10.1177/014860718601000149. [DOI] [PubMed] [Google Scholar]
- 14.Nelson M. Today's CPE: Medicare reimbursement of home nutrition support. Today's Dietitian. 2007;9(1):12. [Google Scholar]
- 15.Howard L. Home parenteral nutrition: survival, cost, and quality of life. Gastroenterology. 2006;130(2)(suppl 1):S52–S59. doi: 10.1053/j.gastro.2005.09.065. [DOI] [PubMed] [Google Scholar]
- 16.Piamjariyakul U, Ross VM, Yadrich DM, Williams AR, Howard L, Smith CE. Complex home care: part I—utilization and costs to families for health care services each year. Nurs Econ. 2010;28(4):255–263. [PMC free article] [PubMed] [Google Scholar]
- 17.Piamjariyakul U, Smith CE. Utilization reports and evaluation. In: Montoney L, Gomez C, editors. Telemedicine in the 21st Century. Nova Science Publishers; Hauppauge, NY: 2008. pp. 41–53. [Google Scholar]
- 18.Bynum AB, Cranford CO, Irwin CA, Banken JA. Effect of telemedicine on patients’ diagnosis and treatment. J Telemed Telecare. 2006;12(1):39–43. doi: 10.1258/135763306775321407. [DOI] [PubMed] [Google Scholar]
- 19.Osborne H. Health Literacy: From A to Z. 2nd ed. Bartlett Learning; Burlington, MA: 2011. [Google Scholar]
- 20.Puxty A. Traditional costing and use of systems approach. Management Accounting. 1980;58(7):28–45. [Google Scholar]
- 21.Capenski LC. Healthcare Finance: An Introduction to Accounting and Financial Management. 4th ed. Health Administration Press; Ann Arbor, MI: 2007. [Google Scholar]
- 22.Lev B, Sougiannis T. The capitalization, amortization, and value-relevance of R & D. J Account Econ. 1996;21(1):107–138. [Google Scholar]
- 23.Andersen MR, Hager M, Su C, Urban N. Analysis of the cost-effectiveness of mammography promotion by volunteers in rural communities. Health Educ Behav. 2002;29(6):755–770. doi: 10.1177/109019802237942. [DOI] [PubMed] [Google Scholar]
- 24.Urban N, Self S, Kessler L, et al. Analysis of the costs of a large prevention trial. Control Clin Trials. 1990;11(2):129–146. doi: 10.1016/0197-2456(90)90006-n. [DOI] [PubMed] [Google Scholar]
- 25.Lairson DR, Huo J, Ricks KA, Savas L, Fernández ME. The cost of implementing a 2-1-1 call center-based cancer control navigator program. Eval Program Plann. 2013;39:51–56. doi: 10.1016/j.evalprogplan.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 26.Reardon T. Research findings and strategies for assessing telemedicine costs. Telemed J E Health. 2005;11(3):348–369. doi: 10.1089/tmj.2005.11.348. [DOI] [PubMed] [Google Scholar]
- 27.Ross VM, Smith CE. National clinical guidelines and home parenteral nutrition. Nutr Clin Pract. 2011;26(6):656–664. doi: 10.1177/0884533611423264. [DOI] [PubMed] [Google Scholar]
- 28.Mistry H, Garnvwa H, Oppong R. Critical appraisal of published systematic reviews assessing the cost-effectiveness of telemedicine studies. Telemed e-Health. 2014;20(7):609–618. doi: 10.1089/tmj.2013.0259. [DOI] [PubMed] [Google Scholar]
- 29.Bashshur RL, Shannon GW, Smith BR, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed e-Health. doi: 10.1089/tmj.2014.9981. [published online June 26, 2014] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.ESRI (Environmental Systems Resource Institute) ArcMap 10.1. ESRI; Redlands, CA: 2009. [Google Scholar]
- 31.Smith CE, Puno F, Werkowitch M, Cofer A, Whitman R, Pingleton S. Website algorithms for home nursing care & physiologic measures via the Internet. Gerotechnol J. 2005;3(4):195–210. [Google Scholar]
- 32.World Health Organization [June 19, 2014];International Classification of Diseases (ICD), Tenth Revision. 2010 http://apps.who.int/classifications/icd10/browse/2010/en.
- 33.Lin H, Hsu Y, Hsu M, Cheng C. Case study: development of a telehealth-care decision support system for patients discharged from the hospital. Telemed e-Health. 2014;20(8):748–759. doi: 10.1089/tmj.2013.0261. [DOI] [PubMed] [Google Scholar]
- 34.American Telemedicine Association. State Telemedicine Policy Center [July 19, 2014];2014 http://www.americantelemed.org/policy/state-telemedicine-policy#.U9fGepB0wqQ.
- 35.Healthcare IT News. Health IT attracting huge investments [July 25, 2014];2014 http://www.healthcareitnews.com/news/health-it-attracting-huge-investments.