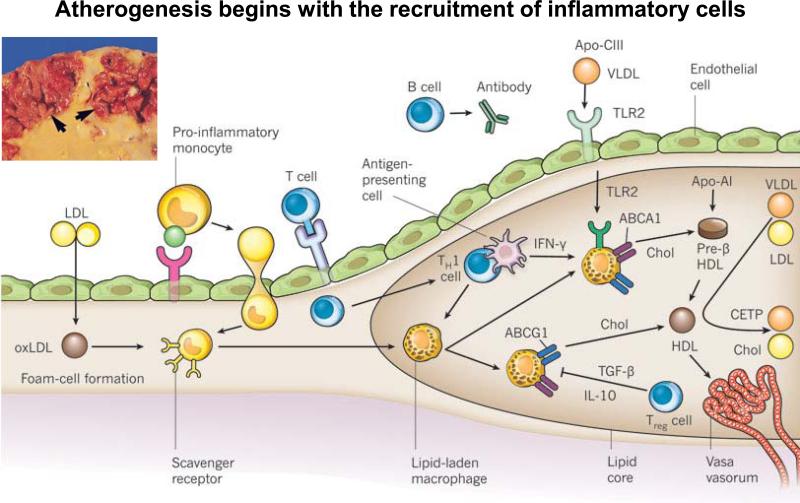
Figure 2.
Atherogenesis and inflammation, adapted with permission from Libby P. et al. Nature 2011:473, 317–325. Atherogenesis begins with the recruitment of inflammatory cells to the intima. Activated endothelial cells express leukocyte adhesion molecules that capture and recruit blood monocytes to the intima. These activated monocytes express scavenger receptors that permit the uptake of modified LDL particles, such as oxidized LDL (oxLDL). Cholesterol loading leads to the formation of foam cells, and ultimately leads to the mature lipid-laden macrophages of the plaque's core. These cells can produce pro-inflammatory mediators, reactive oxygen species, and tissue factor pro-coagulants that amplify local inflammation and promote thrombotic complications. Although fewer in number than the mononuclear phagocytes, T cells also enter the intima and send decisive regulatory signals. After antigen-specific activation, T helper 1 (TH1) cells secrete the signature cytokine interferon-g (IFN-g), which can activate vascular wall cells and macrophages, and magnify and sustain the inflammatory response in the intima. Regulatory T (Treg) cells produce interleukin-10 (IL-10) and transforming growth factor-β (TGF-β), two cytokines considered to exert anti-inflammatory actions.