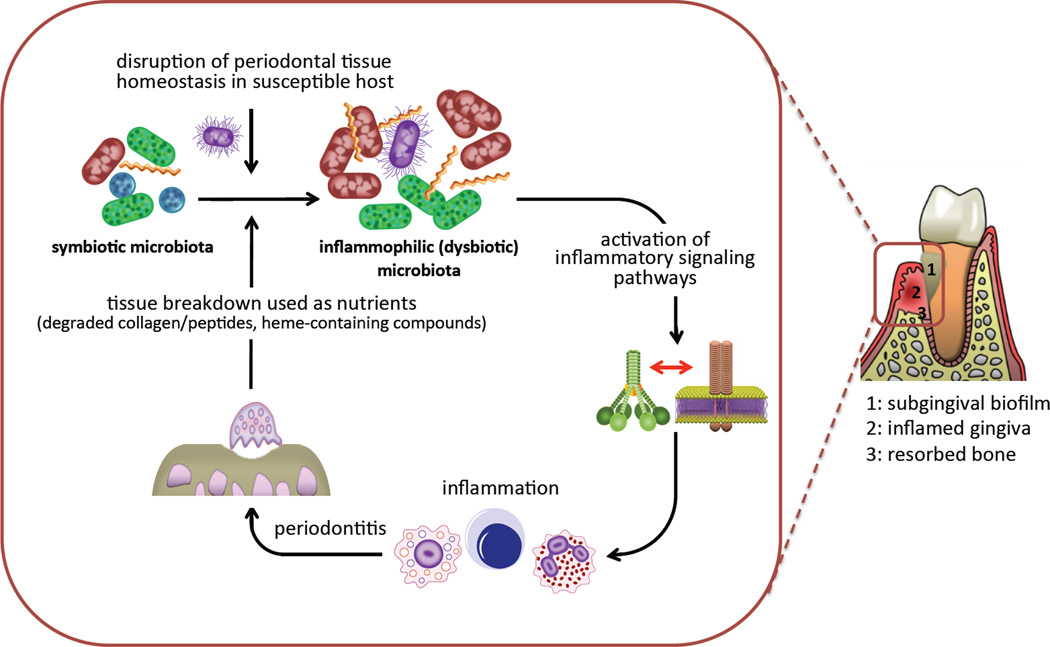
Figure 1. Inflammation and dysbiosis in periodontitis.
Various factors including defects in the immuno-inflammatory status of the host and/or the presence of keystone pathogens can tip the balance from a symbiotic periodontal microbiota to a dysbiotic state. The inflammation caused by the dysbiotic microbiota depends in great part on crosstalk signaling between complement and pattern-recognition receptors and exerts two major and interrelated effects: it causes inflammatory destruction of periodontal tissue (including bone loss, the hallmark of periodontitis) which in turn provides tissue breakdown-derived nutrients for the bacteria. The latter further promotes dysbiosis and escalates tissue destruction, thereby generating a self-perpetuating pathogenic cycle. Therefore, the periodontitis-associated dysbiotic communities are ‘inflammo-philic’ (= loving or attracted to inflammation) in that they appear to have evolved to not only endure inflammation but also to take advantage of it for enhancing their adaptive fitness.