Abstract
Background
Outcome measures can be used in prosthetic practices to evaluate interventions, inform decision making, monitor progress, document outcomes, and justify services. Strategies to enhance prosthetists' ability to use outcome measures are needed to facilitate their adoption in routine practice.
Objective
To assess prosthetists' use of outcome measures and evaluate the effects of training on their confidence administering performance-based measures.
Design
Cross-sectional and single group pretest-posttest survey
Methods
Seventy-nine certified prosthetists (mean of 16.0 years of clinical experience) were surveyed about their experiences with 20 standardized outcome measures. Prosthetists were formally trained by the investigators to administer the Timed Up and Go and Amputee Mobility Predictor. Prosthetists’ confidence in administering the Timed Up and Go and Amputee Mobility Predictor was measured before and after training.
Results
The majority (62%) of prosthetists were classified as non-routine outcome measure users. Confidence administering the TUG and AMP prior to training was low-to-moderate across the study sample. Training significantly (p<0.0001) improved prosthetists' confidence administering both instruments.
Conclusion
Prosthetists in this study reported limited use of and confidence with standardized outcome measures. Interactive training resulted in a statistically significant increase of prosthetists' confidence in administering the TUG and AMP and may facilitate use of outcome measures in clinical practice.
II. Clinical Relevance
Frequency of outcome measure use in the care of persons with limb loss has not been studied. Study results suggest that prosthetists may not regularly use standardized outcome measures and report limited confidence in administering them. Training enhances confidence and may encourage use of outcome measures in clinical practice.
III. Background
Standardized outcomes measurement has long been advocated as a strategy for enhancing the quality of healthcare provided to those who require prosthetic services.1-3 When appropriately selected and administered, self-report and performance-based outcome measures can be used for a variety of purposes, including determining current level of function, predicting future ability, determining contribution of an intervention to function, informing clinical decisions, measuring changes over time, and fulfilling documentation requirements (i.e., to provide supporting evidence about patients' functional abilities for reimbursement purposes). Despite the value for use of outcome measures in prosthetic practices, it is unknown to what extent they are routinely administered or how they are commonly used.
Although standardized outcome measures have not historically been employed in prosthetics practice, prosthetists may soon be required to regularly administer outcome measures and document the results from such instruments in order to justify selected prosthetic interventions. Since 2013, the Centers for Medicare and Medicaid Services (CMS) have required enhanced documentation from providers of physical, occupational, and speech-language therapies describing Medicare beneficiaries' initial function and condition, furnished therapy services, and achieved outcomes.4, 5 To be considered for reimbursement, therapy providers must include non-payable G codes (and modifiers) on the claim forms to document the beneficiary's functional impairments and activity limitations at the outset of therapy, during treatment, and at discharge. G codes are functional classifiers, based on the World Health Organization's International Classification of Functioning, Disability, and Health (ICF)6, used to describe a patient's current impairment and associated activity limitations. In short, healthcare providers are now being required to document outcomes that demonstrate the functional value of the interventions selected. It is reasonable to assume that prosthetists may soon be required to provide G codes or similar documentation of outcomes assessment in the provision of prosthetic services.
Practitioners' lack of familiarity and experience with standardized outcome measures may be a barrier to their routine use in prosthetics practice.7-9 While contemporary prosthetic and orthotic educational standards10 require competency in clinical evaluation and documentation (skills which typically include standardized procedures for outcome assessment), academic programs have only recently adopted standardized outcomes measurement in their curricula. Therefore, a large majority of practicing prosthetists may be unfamiliar with appropriate use of outcome measures in clinical practice. This gap in knowledge and experience could be addressed by introducing outcome measure training through professional continuing education courses. Specifically, mixed-method education strategies, which have been shown to produce more effective learning than didactic or interactive methods alone,11 may be employed to enhance prosthetists' comfort with standardized measurement of patient outcomes. Such training may help overcome prosthetists' limited exposure to and familiarity with outcome measures. However, the effects of mixed-method training on prosthetists' confidence in administering outcomes measures have not been examined.
The purpose of this study was to assess prosthetists' routine use of outcome measures and to evaluate the effects of a training program on prosthetists' confidence in administering two common performance-based outcome measures. We hypothesized that the majority of prosthetists do not routinely use outcome measures when evaluating patients and that an interactive training program would significantly improve prosthetists' confidence in administering the trained outcome measures. Support of these hypotheses would indicate the presence of barriers to outcomes measurement with prosthetic patients and a strategy (i.e., training) to facilitate their use in clinical practices.
III. Methods
Study Design
This study was conducted to determine prosthetists' experience with performance-based and self-report outcome measures and to assess the impact of formal training on prosthetists' confidence in administering selected performance-based measures. Prosthetist participants agreed to attend a hands-on, interactive training program and complete pre- and post-training surveys. Participants were trained to appropriately administer two performance-based measures, the Timed Up and Go (TUG)12 and the Amputee Mobility Predictor (AMP).13 Both the TUG and AMP have been reported to be reliable and valid measures of mobility in persons with lower limb loss13, 14 and are recommended for use in clinical practice and research.15 Pre-training surveys were used to assess prosthetists' typical use of outcome measures in clinical practice. Pre-training and post-training surveys were used to measure confidence in administering the TUG and the AMP. The surveys were developed by the investigators for the purpose of this study.
Training sessions were conducted at prosthetic clinics across the United States. Clinics were identified by the study investigators through professional contacts. Participants were certified and licensed (if applicable) to provide prosthetic services and regularly engaged in the prosthetic care of persons with lower limb loss. All participants met a minimum requirement of providing at least five prosthetic prescriptions per year. Prosthetists were screened for eligibility by phone or email prior to participating in the study. All study procedures were reviewed and approved by the University of Washington and Miami Veterans Affairs Healthcare System institutional review boards.
Study Procedures
Pre-training Survey
Prosthetists completed a pre-training survey to collect basic demographic information (i.e., gender, race, ethnicity, degree and/or certification attained, years of clinical practice, additional training and education in another profession). Participants were also asked three questions pertaining to their use of outcome measures in clinical practice:
“Have you ever administered any of the following standardized outcome measures in your daily clinical practice outside of this study?”
“How frequently do you use standardized outcome measures to accomplish the following clinical tasks?”
“How confident are you in your current ability to administer the following outcome measures?”
Question 1 included a list of 20 performance-based (e.g., 6-Minute Walk Test16, Berg Balance Scale17) and self-report outcome measures (e.g., Prosthesis Evaluation Questionnaire18, Activities Specific Balance Confidence Scale19) that have been used to assess persons with lower limb loss. The list of measures (Table 1) was compiled by the investigators from various sources, including a recent review of lower limb prosthetic outcome measures15. Question 2 included six potential outcome measure applications (i.e., document patient status, inform clinical decisions, justify selection of interventions, monitor patients over time, communicate information to others, and predict patient outcomes). The applications included in the survey were adapted from intended uses of standardized measures described by Potter et al.20 Question 3 included reference to the Timed Up and Go (TUG)12 and the Amputee Mobility Predictor (AMP).13 Questions 1 and 2 were assessed on a 5-level ordinal scale with responses that described frequency of use (i.e., never, rarely, sometimes, often, and always). Question 3 was assessed on a 5-level ordinal scale with responses that described degree of confidence (i.e., not at all, a little bit, somewhat, quite a bit, and very much).
Table 1. Outcome measures polled in the pre-training survey.
| Outcome Measure Name |
|---|
| Amputee mobility predictor (AMP) |
| Patient Assessment Validation Evaluation Test (PAVET) |
| Distance Walk Test (DWT) (e.g., 10-Meter Walk Test) |
| Timed Walk Test (TWT) (e.g., 2-Minute Walk Test) |
| Prosthesis Evaluation Questionnaire (PEQ) |
| Activities Specific Balance Confidence Scale (ABC) |
| Timed Up and Go (TUG) |
| Prosthetic Profile of the Amputee (PPA) |
| Borg Rating of Perceived Exertion (RPE) |
| Functional Mobility of the Amputee (FMA) |
| Orthotic and Prosthetic Users Survey (OPUS) |
| Short-Form 8, 12, or 36 (SF-8, SF-12, or SF-36) |
| Step Activity Monitor (SAM) |
| Berg Balance Scale (BBS) |
| Houghton Questionnaire |
| Locomotor Capabilities Index (LCI) |
| Lower Extremity Functional Scale (LEFS) |
| Rivermead Mobility Index (RMI) |
| Nottingham Health Profile (NHP) |
| Trinity Amputation and Prostheses Experience Scales (TAPES) |
Training Program
Study investigators (i.e., certified and licensed prosthetists and physical therapists (PT)) conducted the training program. The training program combined didactic (e.g., presentation and period of question and answer) and interactive (e.g., role play and practice administering measures) instructional methods. Mixed methods courses have been shown to produce more effective learning than those based on either method alone.11 The investigators began each training session with a PowerPoint presentation that reviewed the clinical value of outcome measures, general principles of outcome measures as they apply to prosthetic patients, and the psychometric properties, administration methods, and scoring guidelines for the TUG and the AMP. The study investigators then demonstrated set-up, administration, and scoring on volunteer patients with lower limb amputation (if available), a training program participant, or a colleague. Following the demonstration, the prosthetists were required to practice administration, interpretation, and scoring of the measures under observation of study investigators. Study investigators gave the prosthetists verbal, tactile, and positional feedback, as needed, throughout the training. Instructional videos of both set-up and administration of the TUG and AMP were provided to prosthetists on tablet computers (Apple iPad, Cupertino, CA) and reviewed prior to the conclusion of the training. Prosthetists were also provided with written instructions on how to administer and score the TUG and AMP for later reference.
Post-training Survey
Immediately after training, prosthetists completed a brief survey that asked them to again rate their confidence in performing the TUG and AMP (i.e., Question 3, above). Results of the pre- and post-training surveys were compared to evaluate effectiveness of the training program in increasing prosthetists' confidence in administering the measures.
Analyses
Data were analyzed using SAS 9.3 statistical software (SAS Institute Inc., Cary, NC). Response frequencies and means were calculated for demographic information and survey results. The responses for Questions 1 and 2 were collapsed into two categories (i.e., “routine users” and “non-routine users”) for ease of interpretation. “Routine users” of outcome measures were defined as those prosthetists who indicated that they “often” or “always” used a measure. Conversely, “non-routine users” were defined as those who indicated that they “sometimes,” “rarely” or “never” used a measure. Routine and non-routine users' demographic characteristics, frequency of outcome measure use, and reasons for use of outcome measures were compared using the Chi Square test for categorical variables (e.g., frequency of outcome measure use) and the Wilcoxon signed-rank test for continuous variables (e.g., years of practice). Differences in prosthetists' pre- and post-training confidence scores (i.e., Question 3) were assessed using the Wilcoxon signed-rank test with a threshold for significance set at α = 0.05. This nonparametric test was used because responses to the confidence items were not normally distributed.
IV. Results
A total of 79 prosthetists from 37 clinics participated in the study (Table 2). Clinics were located in 12 states (Florida, Illinois, Massachusetts, Maryland, Michigan, New Hampshire, New Jersey, Oregon, Pennsylvania, Tennessee, Texas, and Washington). Prosthetists had a mean ± standard deviation (SD) age of 42.9 ± 9.8 years and had been in practice for 16.0 ± 10.6 years at the time of the survey. The majority of the participants (76%) had completed either a prosthetic certificate or a bachelor's degree in prosthetics. Few participants (5%) completed a Master's degree. Most were certified in both prosthetics and orthotics (65%).
Table 2. Characteristics of study participants.
| All Participants (n = 79) |
Routine Usersa (n = 30) |
Non-routine Usersb (n = 49) |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Gender | ||||||
| Male | 60 | 75.9% | 23 | 76.7 | 37 | 75.5 |
| Female | 19 | 24.1% | 7 | 23.3 | 12 | 24.5 |
| Race/Ethnicity | ||||||
| NH White | 68 | 86.1% | 27 | 90.0 | 41 | 83.7 |
| Asian | 7 | 8.9% | 2 | 6.7 | 5 | 10.2 |
| Hispanic | 3 | 3.8% | 1 | 3.3 | 2 | 4.1 |
| More than 1 race | 1 | 1.3% | 0 | 0 | 1 | 2.0 |
| Educationc | ||||||
| Certificate only | 23 | 29.1% | 12 | 40.0% | 11 | 22.4% |
| Bachelor's only | 37 | 46.8% | 9 | 30.0% | 28 | 57.1% |
| Certificate & Bachelors | 12 | 15.2% | 5 | 16.7% | 7 | 14.3% |
| Certificate & Masters | 4 | 5.1% | 3 | 10.0% | 1 | 2.0% |
| Certificate and Other | 3 | 3.8% | 1 | 3.3% | 2 | 4.1% |
| Clinical Certification | ||||||
| CP | 24 | 30.4% | 13 | 43.3 | 10 | 20.4 |
| CPO | 51 | 64.6% | 15 | 50.0 | 35 | 71.4 |
| Other | 4 | 5.1% | 1 | 3.3 | 3 | 6.1 |
| Other Clinical Experiencec | ||||||
| Physical or Occupational Therapy | 6 | 7.6% | ||||
| Exercise physiology, Personal Training or Athletic Training | 5 | 6.3% | ||||
| Other | 3 | 3.8% | ||||
CP: certified prosthetist; CPO: certified prosthetist/orthotist.
Participants answered Question 1 (any item) with “often” or “always.”
Participants answered Question 1 (all items) with “never,” “rarely,” or “sometimes.”
Participants may check more than 1 option (i.e., cumulative percent may be > 100%)
The majority of prosthetists (62%) were categorized as “non-routine” users, as they reported using none of the 20 surveyed outcome measures in their daily clinical practices. There were no statistically significant differences (p>0.05) between routine and non-routine outcome measure users in terms of age, years in clinical practice, gender, ethnicity, education, or certification. Measures most commonly administered by routine users included the AMP (22%), Patient Assessment Validation Evaluation Test (17%), and distance walk test (10%) (Figure 1).
Figure 1. Instruments and surveys used routinely (i.e., always or often) by participants in clinical practice. Measures not shown were not routinely used by any participants.
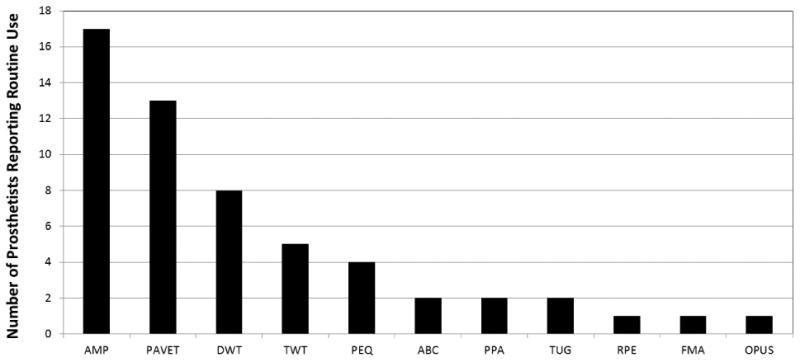
AMP = amputee mobility predictor, PAVET = patient assessment validation evaluation test, DWT = distance walk test, TWT = timed walk test, PEQ = prosthesis evaluation questionnaire, ABC = activities-specific balance confidence scale, PPA = prosthetic profile of the amputee, TUG = timed up and go, RPE = rating of perceived exertion, FMA = functional mobility of the amputee, OPUS = orthotic and prosthetic users survey
Routine users of outcome measures indicated that they used them for multiple reasons. Outcome measures were most commonly (77%) used to justify selection of prosthetic interventions and they were used least often (50%) to predict patient outcomes (Table 3).
Table 3. Participants' reasons for using outcome measures in clinical practice.
| I use standardized outcome measures to… | Routine Users (n = 30) |
Non-routine Users (n = 49) |
||
|---|---|---|---|---|
| n | % | n | % | |
| Justify selection of interventions | 23 | 76.7 | 6 | 12.2 |
| Document patient status | 22 | 73.0 | 5 | 10.2 |
| Inform clinical decisions | 19 | 63.3 | 6 | 12.2 |
| Monitor patients over time | 18 | 60.0 | 5 | 10.2 |
| Communicate information to others | 17 | 56.7 | 4 | 8.2 |
| Predict patient outcomes | 15 | 50.0 | 4 | 8.2 |
Routine users’ pre-training confidence in administration of the TUG and AMP was significantly higher (p = 0.016 and p = 0.0004, respectively) than non-routine users (Table 4). Results from the Wilcoxon signed-rank test indicate that confidence in administration of the TUG and AMP increased significantly (p < 0.0001) in both groups after formal training. No significant differences was found between routine and non-routine users in TUG confidence (median = 5 and 5, range = 4-5 and 3-5, p = 0.79) or in AMP confidence (median = 5 and 5, range 3-5 and 1-5, p = 0.31) after training.
Table 4.
Participants reported confidence (median and range) in the administration of the TUG and AMP.
| Measure | Timed Up and Go (TUG) | Amputee Mobility Predictor (AMP) | ||||
|---|---|---|---|---|---|---|
| Routine Users (n = 30) |
Non-routine Users (n = 48) |
All Participants (n = 78) |
Routine Users (n = 30) |
Non-routine Users (n = 48) |
All Participants (n = 78) |
|
| Pre-training | 3 (1-5) | 2 (1-5) | 2 (1-5) | 4 (1-5) | 2 (1-5) | 3 (1-5) |
| Post-training | 5* (4-5) | 5* (3-5) | 5* (3-5a) | 5* (3-5a) | 5* (1-5b) | 5* (1-5c) |
TUG: Timed Up and Go; AMP: Amputee Mobility Predictor.
Confidence is rated as 1 = “not at all,” 2 = “a little bit,” 3 = “somewhat,” 4 = “quite a bit,” and 5 = “very much.”
One respondent reported 3, all others reported 4–5.
One respondent reported 1, one reported 3, all others reported 4–5.
One respondent reported 1, all others reported 3–5.
Significantly different from pre-training confidence (p < 0.0001).
The majority of prosthetist participants (64%) improved two or more confidence categories after receiving TUG training. In the post-training survey, these prosthetists all reported that they were “quite a bit” or “very much” confident in administering the TUG. Another 21% of participants reported a one-category improvement in confidence and 16% reported no change. We observed similar improvements in prosthetists' confidence in administering the AMP, as 52% of prosthetists improved two or more confidence categories. Similar to the TUG, 26% reported a one-category improvement and 20% reported no change in confidence administering the AMP after training. Only 3% reported worse confidence after AMP training.
V. Discussion
The primary purpose of this study was to examine the frequency of use and the type of outcome measures used by prosthetists in clinical practice. Additionally, we aimed to assess the impact of a didactic and interactive training program on prosthetists' confidence in the administration of two performance-based outcome measures. We hypothesized that the majority of prosthetists do not routinely use outcome measures. We found that only a minority of prosthetists (38%) in this study were routine users of outcome measures in their clinical practices. These results are consistent with reports from other allied health fields (e.g., physical therapy, occupational therapy, and psychology) that have identified limited adoption of outcome measures into routine practices. Jette et al., reported that less than half (48%) of 498 practicing physical therapists (PTs) reported using standardized outcome measures in their clinical practice.9 Stapleton and McBrearty found that between 15% and 39% of 109 practicing occupational therapists (OTs) frequently or consistently used any of five common outcome measures.21 Hatfield and Ogles reported that among a national sample of 874 psychologists, only 37% (n = 324) reported using outcome measures in their clinical practice.8
The AMP and PAVET were the measures most frequently used by prosthetists enrolled into this study. A common trait between these measures is that both of them are intended to guide selection of appropriate prosthetic components. The AMP is a valid and reliable measure of current and future functional capabilities of persons with lower limb amputation.13 AMP scores have been show to significantly differ among persons classified by different Medicare Functional Classification Levels (MFCLs)12 and is recommended for use in determining a patient's appropriate MFCL.22 The PAVET is a proprietary, patient- and clinician-report survey developed by Hanger Orthopedic Group (Austin, TX) to assist clinicians in the evaluation of patients with transfemoral limb loss who may be candidates for microprocessor-controlled prosthetic knees. Evidence to support the reliability, validity, or responsiveness of the PAVET as a standardized outcome measure is currently unavailable. The reported frequency of use of the AMP and PAVET is therefore consistent with survey results which indicate that standardized outcome measurement is most often undertaken for justification purposes. As employers and payers increasingly require documentation of patient outcomes, it is expected that use of these (or similar) measures will grow.
A number of barriers to the routine use of outcome measures in clinical practice have been identified in the literature. Limited knowledge about (selecting, using, and interpreting) standardized outcome measures, insufficient time to administer measures in practice, low organizational priority, and lack of perceived value in outcome measurement have all been reported as barriers across numerous allied health disciplines.7, 9, 23, 24 These same barriers almost certainly exist in the field of prosthetics.
Recent changes to prosthetic and orthotic educational standards10, which now mandate outcome measurement education, are intended to promote greater familiarity and regular use of outcomes measures in clinical practice. However, changes to educational standards alone may not be sufficient to change prosthetists' frequency of outcome measure use in routine clinical practice. Therefore, complimentary or alternative methods of providing outcome measure education and experience are likely needed to promote their use. For example, providing practitioners with greater time and resources for administration, scoring, and analysis at the clinic level or fast-tracking reimbursement of prosthetic service claims that include pre- and post-intervention measurements made with approved instruments could facilitate prosthetists' routine use of outcome measures. Similarly, availability of measures that easily integrate data into patients' electronic medical records, such as those that can be administered and scored via a handheld computer, may also increase acceptance and adoption.
A secondary purpose of this study was to develop, implement, and test a focused training program designed to familiarize prosthetists with two performance-based outcome measures (i.e., the TUG12 and the AMP13). The training program developed for this study incorporated mixed didactic and interactive techniques, as recommended by Forsetlund et. al in a recent Cochrane review11. Mixed techniques, often utilized in academic instruction, were employed to provide both empirical knowledge (e.g., information of the measures' psychometric properties) as well as practical experience (e.g., opportunities to practice administration under the guidance of experienced trainers). The mixed-method training employed in this study was found to be an effective strategy for improving prosthetists' confidence in administering the TUG and AMP. In general, non-routine user's confidence improved two full categories after they received the training and routine user's confidence improved one full category. Furthermore, after training, the non-routine user's confidence in administering the TUG and AMP reached the routine user's confidence level. Similar techniques could be used to teach clinical prosthetists to administer, document, and interpret a range of different outcome measures. Such methods may be a means to address barriers to routine measurement in prosthetics and other professions.
Professional organizations, such as the International Society for Prosthetics and Orthotics (ISPO), American Academy of Orthotists and Prosthetists (AAOP), and American Orthotic and Prosthetic Association (AOPA) have advanced outcomes measurement in O&P by hosting interactive sessions at recent O&P conferences.25-27 The mixed method training provided in this study expanded on the content of these sessions to include periods of focused individual attention by the investigators and provision of various forms of feedback (e.g., verbal, tactile, and positional) that may be atypical in traditional conference sessions or workshops. Although mixed-method training may be impractical in larger settings, such as professional conferences, it may be useful for providing focused outcome measure training to practicing clinicians. Mixed-method outcome measure training workshops may also provide an ideal opportunity for prosthetists to obtain continuing education credits needed to maintain certification and/or licensure while gaining experience and familiarity with outcome measures they can use in their clinical practices.
Study Limitations
Convenience sampling was used to recruit the prosthetists in this study. Therefore, the generalizability of the observed results may be limited. Participants were generally motivated prosthetists who were interested in contributing to research, had experience with prior research projects, and/or wanted additional experience using outcome measures in their clinical practices. As such, we believe that this sample included prosthetists with a range of exposure to and experience with outcome measures and represents a reasonable snapshot of the profession at-large. However, it is possible that our sample may over- or under-represent the outcome measure experience of practicing prosthetists nationwide. Future research may include a larger study to examine if the frequency and use of outcome measures in prosthetic clinical practice reported in this study is representative of routine use across the profession.
The training results described in this study may also be limited to the selected outcome measures. The provided training focused on two performance-based measures, the TUG12 and the AMP.13 These instruments were selected because they are reliable and valid measures of prosthetic mobility and have been recommended for use in clinical care.15 It is acknowledged that the change in prosthetists' confidence observed after AMP and TUG training may not apply to other measures or other forms of measurement, like self-report. As well, it is unknown if the improvements in confidence observed in this study will lead to greater use of these measures in clinical practice. Seminal literature has demonstrated that improvement in confidence can lead to behavioral changes.28 However, a follow-up study would be needed to confirm whether the training provided promoted increased use of the studied measures. Similarly, prosthetists' confidence may change over time. Additional research is needed to determine if confidence is maintained after training (i.e., at 1 week, 1 month, or 1 year post-training).
Finally, a control group was not utilized to determine the effectiveness of the mixed method training approach used in this study. It is unknown if using just a didactic or interactive approach to training would be more or less effective as the combined approach used in this study. Although evidence strongly suggests that mixed-mode education is superior to single mode (i.e., interactive or didactic) education11, a between-groups study would be needed to confirm if it is similarly effective for training clinicians to administer outcome measures in their daily practices.
VI. Conclusion
Prosthetists participating in this study reported limited use of and comfort with outcome measures in clinical practice prior to training. A didactic and interactive training program that provided study participants with the knowledge and opportunity to practice administering the TUG and AMP while receiving performance feedback was found to significantly increase prosthetists' confidence in administering these measures. Study results suggest that training of prosthetists in the performance and interpretation of outcome measures can lead to greater confidence in administration and may facilitate increased use of outcome measures in routine clinical practice. Professional organizations and educators may consider using the mixed method training techniques utilized in this study to expose prosthetists to standardized outcome measures that may be suited to clinical practice.
Acknowledgments
This material is the result of work supported in part with resources and use of facilities at the Miami Veterans Affairs Healthcare System (MVAHS) and South Florida Veterans Affairs Foundation for Research and Education, Inc. (SFVAFRE).
Funding: Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child and Human Development of the National Institutes of Health under award number U01HD065340. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest: The authors declare that there is no conflict of interest.
Author contribution: The authors contributed equally in the preparation of this article.
References
- 1.Resnick L, Borgia M. Reliability of Outcome Measures for People with Lower-Limb Amputation: Distinguishing True Change from Statistical Error. Phys Ther. 2011;91(4):1–11. doi: 10.2522/ptj.20100287. [DOI] [PubMed] [Google Scholar]
- 2.Kohler F, Cieza A, Stucki G, Geertzen J, Burger H, Dillon MP. Developing Core Sets for persons following amputation based on the International Classification of Functioning, Disability and Health as a way to specify functioning. Prosthet Orthot Int. 2009;33(2):117–29. doi: 10.1080/03093640802652029. [DOI] [PubMed] [Google Scholar]
- 3.Gallagher P, Desmond D. Measuring quality of life in prosthetic practice: benefits and challenges. Prosthet Orthot Int. 2007;31(2):167–76. doi: 10.1080/03093640600988633. [DOI] [PubMed] [Google Scholar]
- 4.Resnik L. Medicare mandate for claims-based functional data collection: an opportunity to advance care, or a regulatory burden? Phys Ther. 2013;93(5):587–8. doi: 10.2522/ptj.2013.93.5.587. [DOI] [PubMed] [Google Scholar]
- 5.American Physical Therapy Association. Functional Limitation Reporting Under Medicare: APTA. 2013 cited 2013 December 12, 2013. [Google Scholar]
- 6.World Health Organization. International classification of functioning, disability and health: ICF. Geneva: WHO; 2001. [Google Scholar]
- 7.Duncan EA, Murray J. The barriers and facilitators to routine outcome measurement by allied health professionals in practice: a systematic review. BMC Health Serv Res. 2012;12:1–9. doi: 10.1186/1472-6963-12-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hatfield DR, Ogles BM. The Use of Outcome Measures by Psychologists in Clinical Practice. Professional Psychology: Research and Practice. 2004;35(5):485–91. [Google Scholar]
- 9.Jette DU, Halbert JI, Iverson C, Miceli E, Shan P. Use of Standardized Outcome Measures in Physical Therapy Practice: Perception and Applicability. Phys Ther. 2009;89:125–35. doi: 10.2522/ptj.20080234. [DOI] [PubMed] [Google Scholar]
- 10.National Commission on Orthotic and Prosthetic Education (NCOPE) Core curriculum for orthotists and prosthetists. Alexandria, VA: 2010. [Google Scholar]
- 11.Forsetlund L, Bjorndal A, Rashidian A, Jamtvedt G, O'Brien MA, Wolf F, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009;(2):Cd003030. doi: 10.1002/14651858.CD003030.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Podsiadlo P, Richardson S. The Timed ‘Up and Go”: A Test of Basic Functional Mobility for Frail and Elderly Persons. J Am Geriatr Soc. 1991;39:1452–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 13.Gailey RS, Roach KE, Applegate B, Cho B, Cunniffe B, Licht S. The Amputee Mobility Predictor: An Instrument to Assess Determinants of the Lower Limb Amputee's Ability to Ambulate. Arch Phys Med Rehabil. 2002;86:613–27. doi: 10.1053/apmr.2002.32309. [DOI] [PubMed] [Google Scholar]
- 14.Schoppen T, Boonstra A, Groothoff JW, de Vries J, Goeken L, Eisma W. The Timed “Up and Go” Test: Reliability and Validity in Persons with Unilateral Lower Limb Amputation. Arch Phys Med Rehabil. 1999;80(7):825–28. doi: 10.1016/s0003-9993(99)90234-4. [DOI] [PubMed] [Google Scholar]
- 15.Condie E, Scott H, Treweek S. Lower limb prosthetic outcome measures: a review of the literature 1995 to 2005. J Prosthet Orthot. 2006;18(1S):13–45. [Google Scholar]
- 16.Lin SJ, Bose NH. Six-Minute Walk Test in Persons with Transtibial Amputation. Arch Phys Med Rehabil. 2008;89(12):2354–59. doi: 10.1016/j.apmr.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Berg K, Wood-Dauphinnee S, Williams JI, Gayton D. Measuring balance in the elderly: Preliminary Development of an Instrument. Physiother Can. 1989;41:304–11. [Google Scholar]
- 18.Legro MW, Reiber GD, Smith DG, del Aguila M, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil. 1998;79(8):931–8. doi: 10.1016/s0003-9993(98)90090-9. [DOI] [PubMed] [Google Scholar]
- 19.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 20.Potter K, Fulk GD, Salem Y, Sullivan J. Outcome measures in neurological physical therapy practice: part I. Making sound decisions J Neuro Phys Ther. 2011;35(2):57–64. doi: 10.1097/NPT.0b013e318219a51a. [DOI] [PubMed] [Google Scholar]
- 21.Stapleton T, McBrearty C. Use of Standardised Assessments and Outcome Measures among a Sample of Irish Occupational Therapists working with Adults with Physical Disabilities. Br J Occup Ther. 2009;72(2):55–64. [Google Scholar]
- 22.Gailey RS. Predictive Outcome Measures Versus Functional Outcome Measures in the Lower Limb Amputee. J Prostet Orthot. 2006;18(6):P51–P60. [Google Scholar]
- 23.Wedge FM, Braswell-Christy J, Brown CJ, Foley KT, Graham C, Shaw S. Factors influencing the use of outcome measures in physical therapy practice. Physiotherapy theory and practice. 2012;28(12):119–33. doi: 10.3109/09593985.2011.578706. [DOI] [PubMed] [Google Scholar]
- 24.Bowman J. Challenges to Measuring Outcomes in Occupational Therapy: a Qualitative Focus Group Study. The British Journal of Occupational Therapy. 2006;69(10):464–72. [Google Scholar]
- 25.Coulter CP, Wynne JH, Davis L, Bertram C, Fatone S. Learn Practical Outcome Measurements for Your Post CVA Patient; 38th Annual Meeting of the American Academy of Orthotists & Prosthetists (AAOP); 2012 March 21-24; Atlanta, Georgia. [Google Scholar]
- 26.Gailey R, Gaunaurd IA, Raya M, editors. American Orthotic and Prosthetic Association O&P World Congress 2013. Orlando, Florida: 2013. Discrimination Between Outcome Measurement Tools to Assess Clinical Effectiveness: Is there one right tool for Prosthetists ? [Google Scholar]
- 27.Wynn J, Fatone S, Bertram C, Kaluf B, editors. American Orthotic and Prosthetic Association O&P World Congress 2013. Orlando, Florida: 2013. Organized Session: Learn Reported Outcomes for Your Adult and Pediatric Patients. [Google Scholar]
- 28.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(22):191–215. doi: 10.1037//0033-295x.84.2.191. 84(2):191-215 PR. [DOI] [PubMed] [Google Scholar]


