Abstract
Background:
The use of minimally invasive surgical (MIS) techniques represents the most recent modification of methods used to achieve lumbar interbody fusion. The advantages of minimally invasive spinal instrumentation techniques are less soft tissue injury, reduced blood loss, less postoperative pain and shorter hospital stay while achieving clinical outcomes comparable with equivalent open procedure. The aim was to study the clinicoradiological outcome of minimally invasive transforaminal lumbar interbody fusion.
Materials and Methods:
This prospective study was conducted on 23 patients, 17 females and 6 males, who underwent MIS-transforaminal lumbar interbody fusion (TLIF) followed up for a mean 15 months. The subjects were evaluated for clinical and radiological outcome who were manifested by back pain alone (n = 4) or back pain with leg pain (n = 19) associated with a primary diagnosis of degenerative spondylolisthesis, massive disc herniation, lumbar stenosis, recurrent disc herniation or degenerative disc disease. Paraspinal approach was used in all patients. The clinical outcome was assessed using the revised Oswestry disability index and Macnab criteria.
Results:
The mean age of subjects was 55.45 years. L4-L5 level was operated in 14 subjects, L5-S1 in 7 subjects; L3-L4 and double level was fixed in 1 patient each. L4-L5 degenerative listhesis was the most common indication (n = 12). Average operative time was 3 h. Fourteen patients had excellent results, a good result in 5 subjects, 2 subjects had fair results and 2 had poor results. Three patients had persistent back pain, 4 patients had residual numbness or radiculopathy. All patients had a radiological union except for 1 patient.
Conclusion:
The study demonstrates a good clinicoradiological outcome of minimally invasive TLIF. It is also superior in terms of postoperative back pain, blood loss, hospital stay, recovery time as well as medication use.
Keywords: Degenerative spine, lumbar fusion, minimally invasive transforaminal lumbar interbody fusion, spondylolisthesis
MeSH terms: Spinal arthritis, spondyloarthritis, spondylolisthesis, minimally invasive, spinal fusion
INTRODUCTION
Open transforaminal lumbar interbody fusion (TLIF) has been performed for many years with the aim of improving fusion rates and disc height restoration as compared with the traditional interbody fusion technique.1,2 Wang et al. first reported it as an alternative to posterior lumbar interbody fusion for the management of a variety of spinal disorders.3,4,5 Traditional TLIF is associated with an excessive intraoperative dissection lateral to the facet joints and retraction of the paraspinal musculature, which can lead to denervation and atrophy and an increased risk of “fusion disease.”3
The use of minimally invasive surgical techniques represents the most recent modification of methods used to achieve lumbar interbody fusion, based upon the premise that a smaller, less traumatic incision should afford better recovery and outcomes.4,5,6,7,8 The advantages reported include less soft tissue injury, reduced blood loss, less postoperative pain, shorter hospital stay while achieving clinical outcomes comparable with equivalent open procedure.2,3,4,9,10,11
The minimally invasive TLIF procedure was first described by Holly et al.4,5 It has since become increasing popular method of lumbar interbody fusion. Favorable outcomes of minimally invasive TLIF have been reported with multiple surgical indications.4,9,12
In this study, the authors present the clinicoradiological outcomes of their first 23 consecutive cases performed with a followup of the minimum 1-year to maximum of 5 years.
MATERIALS AND METHODS
The study was conducted after getting clearance from the ethics committee. Informed consent was taken in all cases. The study was conducted from January 2007 to January 2012 on 23 patients with a mean age of 55.45 years (range: 24-78 years) who met the following inclusion and exclusion criteria. The inclusion criteria were (1) degenerative spondylolisthesis (2) lumbar canal stenosis (3) isthmic spondylolisthesis (4) large disc herniations (5) recurrent disc herniation (6) degenerative disc disease. The exclusion criteria were (1) patients with a followup of <2 year (2) more than two level disease (3) grade III or IV spondylolisthesis (4) presence of degenerative scoliosis (5) presence of vertebral fracture (6) presence of infection or tumor.
The most common symptom of the patient was unilateral or bilateral radiculopathy and in three subjects it was back pain. In all patients, the diagnosis was confirmed by antero posterior (AP) and lateral dynamic radiographs and magnetic resonance images (MRI). All cases of single level minimally invasive TLIF were performed by a single surgeon using the tubular retractor system (Medtronics, Memphis, TN, USA). The percutaneous screws used were either the Viper (Depuy, USA) or Sextant (Medtronic, Memphis, TN, USA).
Operative procedure
Under general anesthesia the patients were positioned in the prone position on a radiolucent table on Iliac and chest rolls. Using AP and lateral fluoroscopic images, the pedicles and the midline structures were marked [Figure 1]. Skin incision of approximately 3 cm in length was made up to the fascia. With the help of the dilator tubes, using with the muscles splitting approach, the tubular retractor was docked over the facet joint [Figure 2]. The correct placement of the tubular retractor was checked fluoroscopically. The surgery was performed from the more symptomatic side, the inferior facet was resected and the exiting nerve and traversing root was identified and decompressed. A complete discectomy was done. The endplates were prepared using scrapers and angled curettes. The locally harvested bone graft obtained by local laminectomy was packed into the interbody space anteriorly. The correct size cage was packed with bone graft and inserted under fluoroscopic control [Figure 3].
Figure 1.

Peroperative clinical photograph showing the marking of the midline and the pedicles of two adjacent segments done under image intensifier
Figure 2.
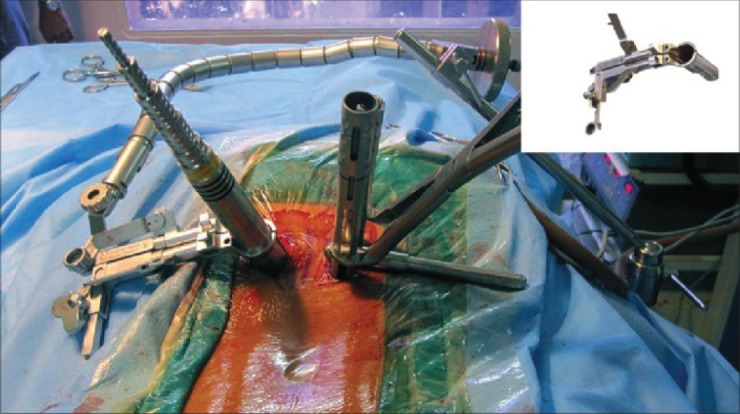
Peroperative clinical photograph showing the docked “quadrant” retractor system along with the dilators (left) the inserted percutaneous screws on the right used for achieving distraction. Inset: the picture of a quadrant retractor
Figure 3.
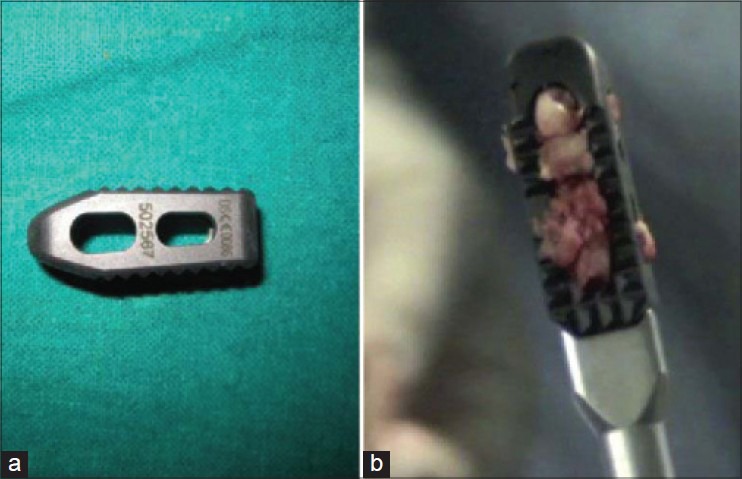
Clinical photograph showing (a) polyetheretherketone cage (b) cage loaded with bone graft on an inserter
The percutaneous pedicle screws were placed on both the sides under fluoroscopic guidance after removal of the tubular retractor. The rods were inserted, and compression was done. The skin was sutured using sub cuticular sutures.
The patients were mobilized on day 2 and depending on the pain tolerance the activity was increased. All patients were evaluated preoperatively and postoperatively on day 18, 1-month, 3 months, 6 months and 1-year [Figure 4].
Figure 4.
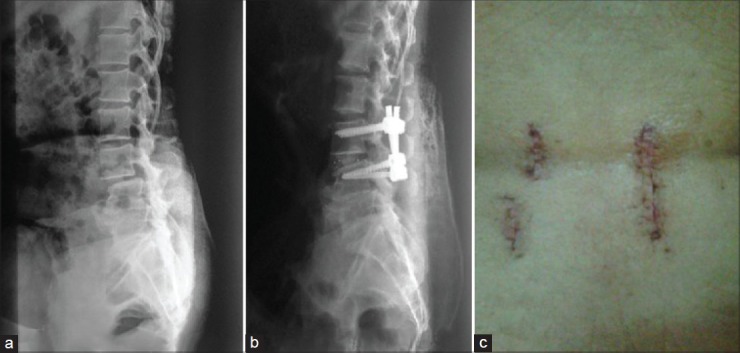
(a) Preoperative X-ray lumbosacral spine (lateral view) showing canal stenosis and grade I listhesis of L3L4 (b) Postoperative X-ray lumbosacral spine showing fixation of L3L4 vertebral body by pedicle screw rod system and fusion by cage (c) Postoperative clinical photograph showing scar
The clinical outcome was assessed using the revised Oswestry disability index and Macnab criteria.13 For radiological evaluation, the AP and lateral dynamic radiographs were done [Figure 5]. Definitive fusion was identified by the formation of trabecular bony bridges between contagious vertebral bodies of the instrumented levels, intact hardware and <3° segmental movement according to fusion criteria.3,13 Figure 6 depicts fluoroscopic images of stepwise procedure.
Figure 5.
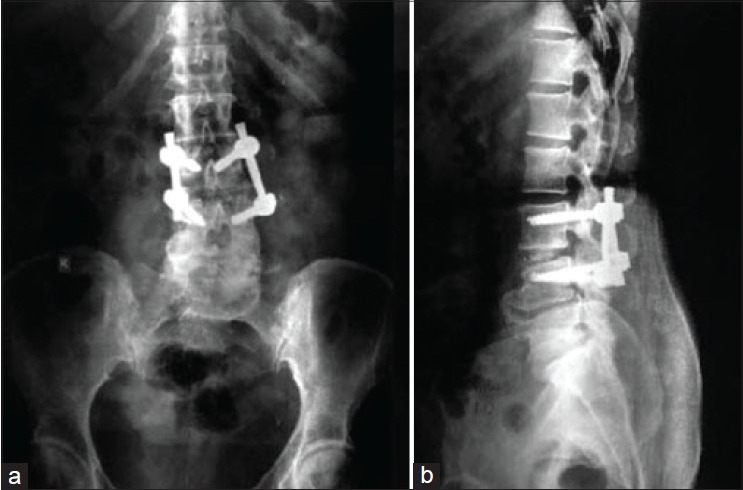
Followup X-rays lumbosacral spine anteroposterior (a) and lateral views (b) showing implant in situ and anterior bridging bone
Figure 6.
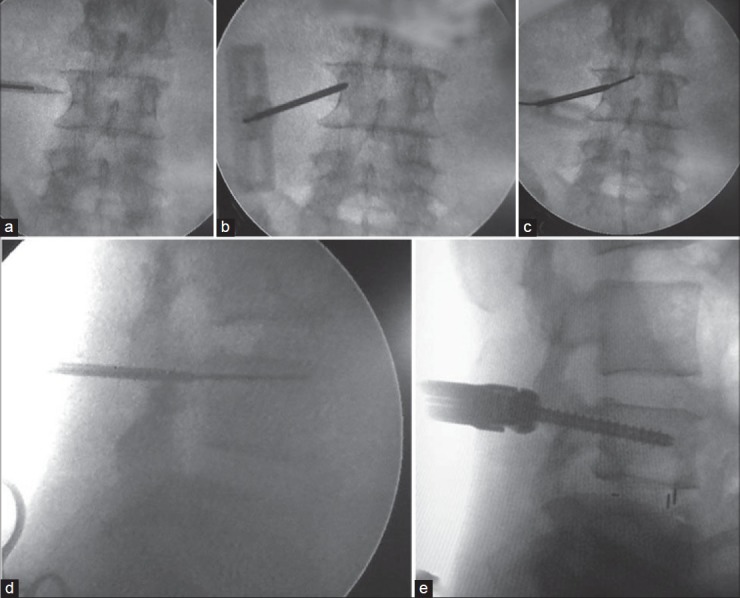
Fluoroscopic images showing (a) marking incision on inspiratory impedance threshold valve. (b) Jamshedi needle in pedicle. (c) guide wire inserted over Jamshedi needle antero-posterior view. (d) Guide wire inserted over Jamshedi needle lateral view. (e) Screw inserted over guide wire
Postoperative computed tomography (CT) scans were done in 5 cases to check for proper screw placement. MRI was not done as it is not a routine practice.
RESULTS
The average followup was 16 months (range 1-5 years). We had no dropouts in our followup. The results were evaluated using the revised Oswestry disability index and the Macnab criteria. There were 6 males and 17 females. L4-L5 level was operated in 14 subjects and L5-S1 in 7 subjects; double level was fixed in 1 patient. L4-L5 degenerative listhesis was the most common indication (n = 12). Symptomatically 9 patients had back pain with bilateral claudication. Back pain with unilateral claudication in 77 patients and 4 had severe back pain [Table 1].
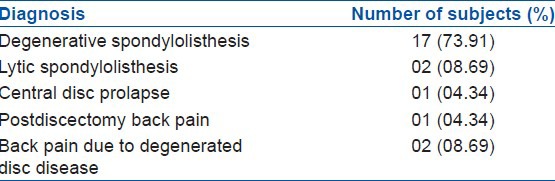
Table 1.
Diagnostic features of patients
Paraspinal approach was taken in all patients with average operative time of 3 h (range 2.5-5.5 h) [Table 2].
Table 2.
Outcome of minimally invasive TLIF (n=23)
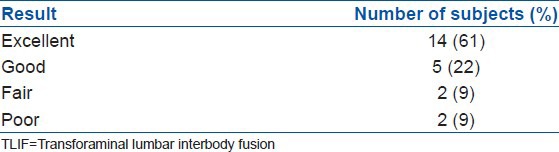
There was a significant decrease in modified Oswestry scores in all patients. Three patients had persistent back pain after the procedure and four patients had residual numbness or radiculopathy.
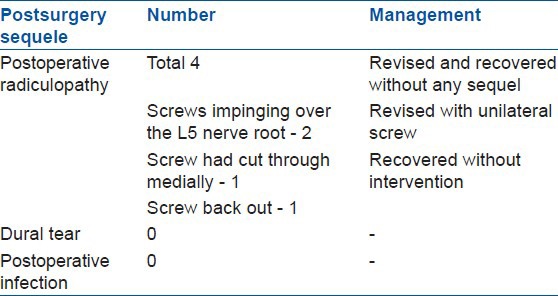
Postoperative CT scan was done in 5 subjects, who had clinical suspicion of screw malposition. These patients had developed postoperative radiculopathy. In two patients screws were found to impinge over the L5 nerve root, in 1 the screw had cut through medially and in the other patient screw back out was noted [Table 3]. Both the cases with nerve impingement were revised, and they recovered without any sequel. One patient who had S1 numbness and radiculopathy postoperative, recovered completely. One case required revision in which unilateral screws were inserted and was associated with a poor result as the subject continued to have low back pain.
Table 3.
Postsurgery sequel and management (n=23)
Allograft was used in 1 case as local bone was inadequate, and the subject had an uneventful recovery. There was rod insertion difficulty in 1 subject. One case required screws to be inserted by open technique and the subject went to get excellent outcome. None of the 23 patients had a Dural tear or postoperative infection.
DISCUSSION
The goal of surgery is to achieve a solid fusion of the lumbar spine. Arthrodesis thus achieved alleviates pain.1,2,3,4,6 Traditionally, open posterior fusion techniques are commonly used. However, decompression, disc preparation, insertion of interbody cage and implantation of spinal instrumentation requires extensive tissue dissection to gain access to the disc space and provide the ideal lateral to medial orientation for optimal screw trajectory. Excessive intraoperative dissection upto. To the facet joints and retraction of the paraspinal musculature can lead to denervation and atrophy, which result in an increased risk of “fusion disease.” Open surgery with significant blood loss and an increased risk of infection are not uncommon. Arikat et al.5 demonstrated long term radiographic atrophy of the operated muscle segment after cases requiring extensive posterior surgical exposure. Recent studies analyzed the amount of muscle damage, via measurements of creatine kinase (CK), which occurs with various types of spine surgery. Open lumbar fusions had a significantly higher amount of CK (muscle damage) in comparison to other minimally invasive procedures.5 Unlike the traditional open TLIF procedure, minimally invasive TLIF uses specially designed retractor system to obtain a working channel within the muscle fibers and permits access to the bony anatomy without stripping muscle. Thus the physiological function of the paraspinal muscles is preserved as it preserves the posterior tension band, and it also helps decrease the postoperative pain, hospital stay.3,6
Minimally invasive TLIF requires an excellent working knowledge of anatomy and is difficult to attempt minimally invasive TLIF for the following reasons.10 The first concerns its learning curve, the second that it takes longer operative time than a conventional open lumbar fusion, third is that it is difficult to treat bilateral symptoms using a unilateral approach and fourth that more radiation time than lumbar fusion during surgery.1,8
The benefits of the minimally invasive TLIF have been highlighted in many studies.12,14 Reduced blood loss is expected in using this technique, which leads to reduced blood trans fusions and risks associated with it.12,16,17 The operative times were slightly higher but statistically insignificant as the time duration decreased with the learning curve.8 Our average operative time in this series was 180 min, which is comparable with Rouben et al. who reported an operative time of 183 min.14 The postoperative clinical outcome as assessed with the Oswestry questionnaire and the Macnab criteria, the results were comparable to other studies.5,9 Union achieved in other studies is comparable to our series, Rouben et al. obtained fusion in 96% of their subjects and Parker et al. had a fusion rate of 89%, that is comparable to our study.14,15 We had nonunion in one case. We used allograft in one case and fusion was achieved in that subject too.
Minimally invasive when compared to open TLIF is associated with a decreased reported incidence of surgical site infections in the literature and may be a valuable tool in reducing hospital costs associated with spine care in our study too.15 We had no incidence of postoperative infection. Infections were not seen in our study although Wang et al. and Rouben et al. reported cases of superficial infection in their study.3,14 Lee et al.1 (n = 1) and Wang et al.3 had a higher incidence of Dural tears (n = 5) as compared to our study which may be due to a gradual learning curve in our hospital, from minimally invasive discectomy to minimally invasive TLIF. Jhala et al.18 in their learning experience of micro endoscopic discectomy concluded that micro endoscopic procedures are safe and effective once the learning curve is overcome. The most important and common complication that required revision was misplacement of screws.3 This is due to heavy reliance on c-arm for placement of screws. Villavicencio et al.8 compared the screw misplacement in open and minimally invasive methods and concluded that this complication is common in both methods, but the incidence is higher in minimally invasive method.
The limitations of study are that even though the data were prospectively collected, the study is retrospective in nature and the patients were not randomly selected. The cohort size is not large enough. Our followup is not long enough to comment of minimally invasive TLIF procedure on the adjacent segment. CT scans were not used to access fusion postoperative.
Despite the limitations of the study, the results demonstrate a good clinical and radiological outcome of minimally invasive TLIF. The procedure is safe and effective once the learning curve is overcome. It is associated with equivalent results with less bleeding and faster rehabilitation when compared to the open procedure.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Lee CK, Park JY, Zhang HY. Minimally invasive transforaminal lumbar interbody fusion using a single interbody cage and a tubular retractor system: Technical tips, and perioperative, radiological and clinical outcome. J Korean Neurosurg Soc. 2010;48:219–4. doi: 10.3340/jkns.2010.48.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tender GC, Ratliff JK. Minimally invasive transforaminal lumbar interbody fusion: Technical note. Open Neurosurg J. 2009;2:8–13. [Google Scholar]
- 3.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Minimally invasive or open transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression of the lumbar spine. Eur Spine J. 2011;20:623–8. doi: 10.1007/s00586-010-1578-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion: Indications, technique, and complications. Neurosurg Focus. 2006;20:E6. doi: 10.3171/foc.2006.20.3.7. [DOI] [PubMed] [Google Scholar]
- 5.Arikat A, Zairi F, Assaker R. Minimally invasive transforaminallumbar interbody fusion: Clinical outcome with a two year followup. Pan Arab J Neurosurg. 2011;15:5–8. [Google Scholar]
- 6.Shunwu F, Xing Z, Fengdong Z, Xiangqian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976) 2010;35:1615–20. doi: 10.1097/BRS.0b013e3181c70fe3. [DOI] [PubMed] [Google Scholar]
- 7.Ng L, Grevitt M. Recent developments in less invasive lumbar spine surgery. J Bone Joint Surg Br. 2010:921–3. [Google Scholar]
- 8.Villavicencio AT, Burneikiene S, Roeca CM, Nelson EL, Mason A. Minimally invasive versus open transforaminal lumbar interbody fusion. Surg Neurol Int. 2010;1:12. doi: 10.4103/2152-7806.63905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park Y, Ha JW, Lee YT, Oh HC, Yoo JH, Kim HB. Surgical outcomes of minimally invasive transforaminal lumbar interbody fusion for the treatment of spondylolisthesis and degenerative segmental instability. Asian Spine J. 2011;5:228–36. doi: 10.4184/asj.2011.5.4.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meyer SA, Wu JC, Mummaneni PV. Mini-open and Minimally invasive transforaminal lumbar interbody fusion: Technique review. Semin Spine Surg. 2011;23:45–50. [Google Scholar]
- 11.Lau D, Lee JG, Han SJ, Lu DC, Chou D. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF) J Clin Neurosci. 2011;18:624–7. doi: 10.1016/j.jocn.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): Technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1–6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 13.Rocchi MB, Sisti D, Benedetti P, Valentini M, Bellagamba S, Federici A. Critical comparison of nine different self-administered questionnaires for the evaluation of disability caused by low back pain. Eura Medicophys. 2005;41:275–81. [PubMed] [Google Scholar]
- 14.Rouben D, Casnellie M, Ferguson M. Longterm durability of minimal invasive posterior transforaminal lumbar interbody fusion: A clinical and radiographic followup. J Spinal Disord Tech. 2011;24:288–96. doi: 10.1097/BSD.0b013e3181f9a60a. [DOI] [PubMed] [Google Scholar]
- 15.Parker SL. Postoperative infection after minimally invasive versus open transforaminal lumbar interbody fusion (TLIF): Literature review and cost analysis. Minim Invasive Neurosurg. 2011;54:33–7. doi: 10.1055/s-0030-1269904. [DOI] [PubMed] [Google Scholar]
- 16.Isaacs RE, Podichetty VK, Santiago P, Sandhu FA, Spears J, Kelly K, et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3:98–105. doi: 10.3171/spi.2005.3.2.0098. [DOI] [PubMed] [Google Scholar]
- 17.Mura PP, Costaglioli M, Piredda M, Caboni S, Casula S. TLIF for symptomatic disc degeneration: A retrospective study of 100 patients. Eur Spine J. 2011;20:S57–60. doi: 10.1007/s00586-011-1761-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jhala A, Mistry M. Endoscopic lumbar discectomy: Experience of first 100 cases. Indian J Orthop. 2010;44:184–90. doi: 10.4103/0019-5413.62051. [DOI] [PMC free article] [PubMed] [Google Scholar]


