Abstract
Background
Technology in orthopaedic surgery has become more widespread in the past 20 years, with emerging evidence of its benefits in arthroplasty. Although patients are aware of benefits of conventional joint replacement, little is known on patients' knowledge of the prevalence, benefits or drawbacks of surgery involving navigation or robotic systems.
Methods
In an outpatient arthroplasty clinic, 100 consecutive patients were approached and given questionnaires to assess their knowledge of navigation and robotics in orthopaedic surgery. Participation in the survey was voluntary.
Results
Ninety-eight patients volunteered to participate in the survey, mean age 56.2 years (range, 19 to 88 years; 52 female, 46 male). Forty percent of patients thought more than 30% of National Health Service (NHS) orthopaedic operations involved navigation or robotics; 80% believed this was the same level or less than the private sector. One-third believed most of an operation could be performed independently by a robotic/navigation system. Amongst perceived benefits of navigation/robotic surgery was more accurate surgery (47%), quicker surgery (50%), and making the surgeon's job easier (52%). Sixty-nine percent believed navigation/robotics was more expensive and 20% believed it held no benefit against conventional surgery, with only 9% believing it led to longer surgery. Almost 50% would not mind at least some of their operation being performed with use of robotics/navigation.
Conclusions
Although few patients were familiar with this new technology, there appeared to be a strong consensus it was quicker and more accurate than conventional surgery. Many patients appear to believe navigation and robotics in orthopaedic surgery is largely the preserve of the private sector. This study demonstrates public knowledge of such new technologies is limited and a need to inform patients of the relative merits and drawbacks of such surgery prior to their more widespread implementation.
Keywords: Robotics, Navigation, Arthroplasty, Patients, Survey
Robotic and navigation (RN) systems have been used in surgery since the 1980s and first became used in orthopaedic surgery in the early 1990s for use in planning of total hip replacements and optimal positioning of final implants. The number of total joint arthroplasty (TJA) procedures performed in the United Kingdom has steadily been increasing with over 150,000 recorded in the National Joint Registry in 2011; however, the number utilising RN systems, the vast majority of which comprise navigation, are 2% of total knee replacements and less than 1% of total hip replacements.1)
The evidence for the benefits of RN systems is growing with short-term improvements in clinical and radiological outcomes reported.2) It is known that patients are well informed about the benefits and have realistic expectations following conventional TJA.3) However, very little is known on patients' knowledge regarding RN systems in orthopaedic surgery. Patients are becoming more resourceful in seeking information from the internet and other media; it has been established that having expectations of surgery met is the strongest predictor of the postoperative assessment of outcomes and satisfaction, even more so than optimal pain relief and the patient's hospital experience.4) It is therefore of utmost importance to have well-informed patients with realistic expectations in order to improve patient satisfaction with their orthopaedic procedures.
The aim of this study was to explore patients' preexisting knowledge and opinions on the prevalence, benefits and drawbacks of RN systems in orthopaedic surgery.
METHODS
A cross-sectional observational study was conducted amongst patients in a lower-limb orthopaedic clinic in October 2011. Patients attending this clinic were either awaiting or being followed-up from arthroplasty or soft tissue surgery of the hip or knee. Surgery involving robotic and navigation systems was not used by the consultant in charge of the clinic. Eligible study participants were at least 16 years of age, the lower age limit of this particular clinic, and able to read and write in English in order to understand the survey. There was no upper age limit. Patients were excluded if they did not have capacity to consent for participation in the survey. The questionnaire was given to all patients in the clinic; it was not restricted to those awaiting or following arthroplasty specifically, as we did not want any influence from patients who may have already been given information on the subject.
A survey was designed that consisted of closedended multiple choice questions (Appendix 1). The questionnaire consisted of demographic information, the patients' knowledge of the prevalence of navigation and robotics, the capabilities, benefits and limitations and opinions of surgery. The questionnaire was pretested with an independent group of five orthopaedic surgeons and five non-medical members of the public in order to assess the clarity and comprehensiveness of the items contained in the questionnaire; all were able to understand the questionnaire and answer all questions fully.
One of the authors (SSJ) approached 100 patients, who were either existing patients of the lead author or new patients referred for assessment. Patients were asked to complete the survey whilst waiting for the consultation. SSJ was available to answer questions and check the questionnaires for completeness and clarify any uncertain, illegible or confusing responses.
Statistical Analysis
Responses were entered into a Microsoft Excel 2010 (Microsoft, Redmond, WA, USA) spreadsheet and tabulated. Further statistical analysis was conducted within Microsoft Excel. A chi-square test was used to assess for differences within the cross section, stratified by age. A statistical significance level of 5% was set for analysis.
RESULTS
Ninety-eight patients successfully completed the questionnaire. Mean age of the responders was 56.2 years, range 19 to 88 years. Thirty-three patients were aged under 50 years and 65 patients were aged over 50 years. Fifty-two patients were female, 46 were male. Only 12% of patients had either received, or knew a family member that had received, orthopaedic surgery involving RN. All patients had knowledge of someone having orthopaedic surgery using conventional techniques. Patients had gained information on arthroplasty from a combination of sources including patient-specific leaflets in the clinic, the internet and information given to them by their surgeon or primary physician.
At least one-third of patients believed that most or all of an operation could be independently performed by a RN system (Fig. 1). Three quarters of patients believed that at least 10% of orthopaedic operations in the National Health Service (NHS) currently used RN systems (Fig. 2). Over 80% believed that this was the same level or less when compared to orthopaedic RN surgery in private practice (Fig. 3). Approximately half of all patients perceived RN surgery to be more accurate, easier for the surgeon and quicker in comparison to conventional surgery (Fig. 4). Approximately 70% of patients recognised that RN surgery was more expensive than conventional surgery and approximately 20% did not believe that it held more benefit than conventional surgery (Fig. 5). Finally, almost 50% of patients wouldn't mind at least some of their surgery performed with the use of RN systems with less than 20% preferring to have none at all involving a RN system (Fig. 6).
Fig. 1.
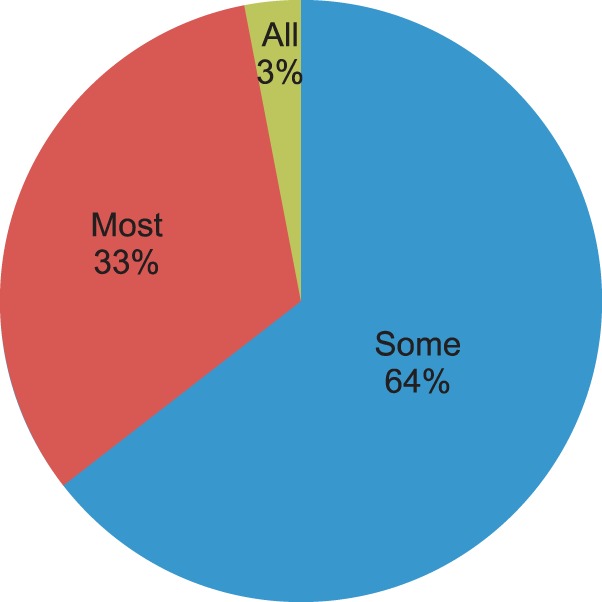
Pie chart of Question 1 responses: How much of an operation do you think can be independently performed by a robot or with navigation? Sixty-four percent believe some of an operation can be performed independently; 33% replied 'most' and 3% stated 'all.'
Fig. 2.
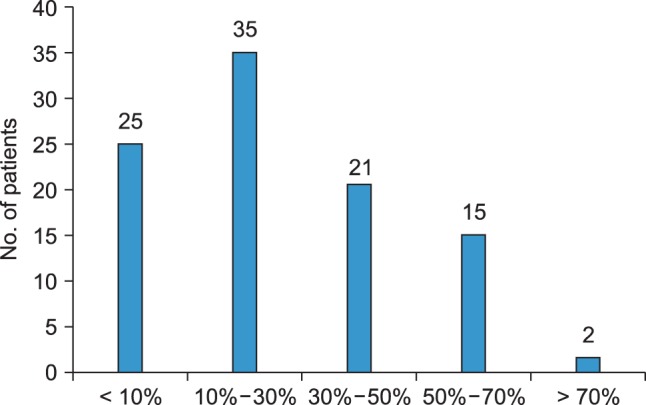
Bar chart of Question 2 responses: Can you estimate what percentage of orthopaedic operations in the National Health Service (NHS) currently use robotics or navigation? Twenty-five percent estimated less than 10% whilst 75% estimated at least 10%. Seventeen percent believed that more than half of NHS operations used robotics or navigation.
Fig. 3.
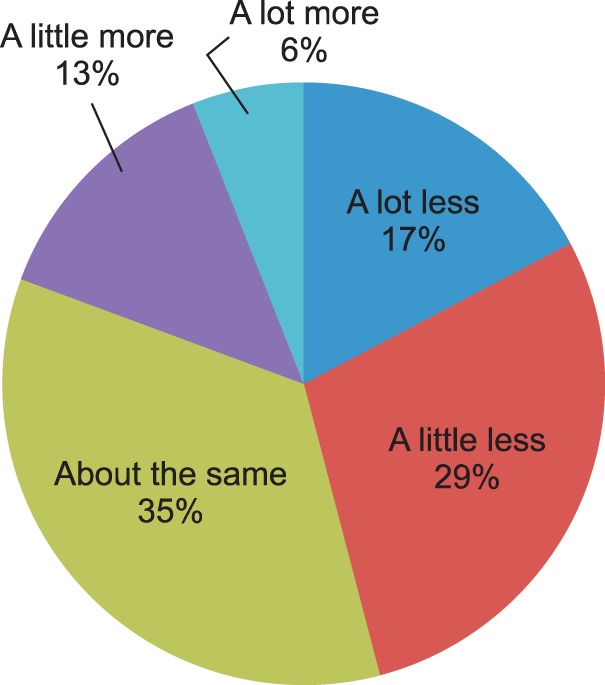
Pie chart of Question 3 responses: How do you think use of robotics and navigation in National Health Service (NHS) compares to use in the private sector? Nineteen percent believed that more was done in the NHS, 35% believed it was the same as in the private sector and 46% believed that more operations involving robotics and navigation were done in the private sector.
Fig. 4.
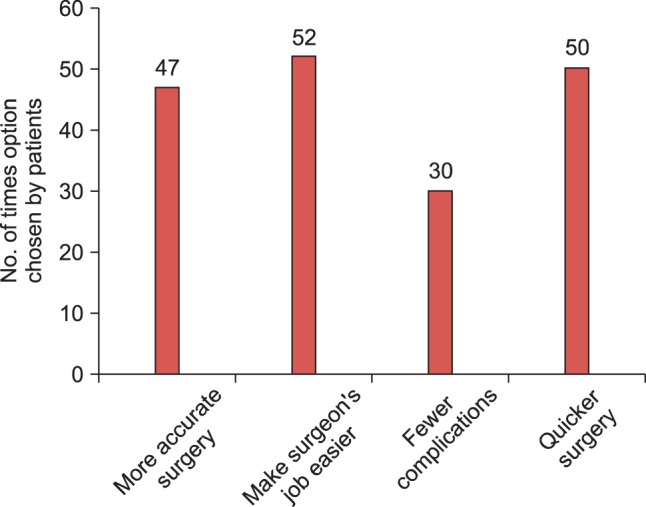
Bar chart of Question 4 responses: What sort of benefits do you think robots and navigation may have for surgery (compared to conventional surgery)? At least 50% of responders believed that surgery involving robotics and navigation was quicker and easier for the surgeon compared to conventional surgery. Forty-seven percent believed it was more accurate and 30% believed it has fewer complications compared to conventional surgery.
Fig. 5.
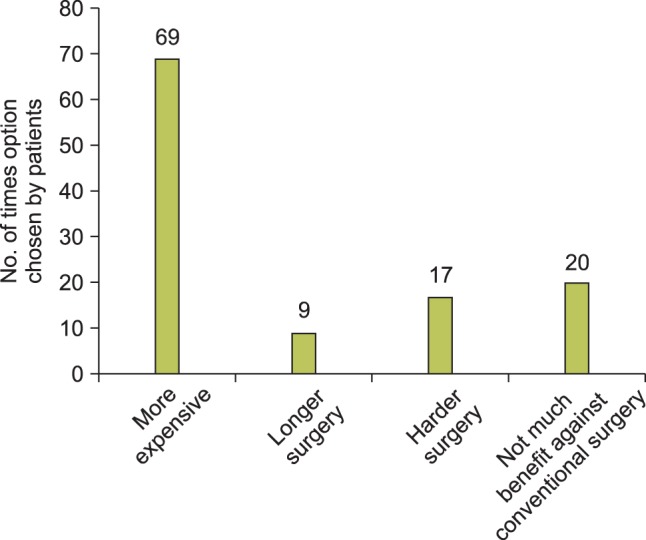
Bar chart of Question 5 responses: What sort of drawbacks do you think robotics and navigation may have for surgery (compared to conventional surgery)? Sixty-nine percent believed it was more expensive compared to conventional surgery. Nine percent thought it took longer and 20% believed there was not much benefit over conventional methods.
Fig. 6.
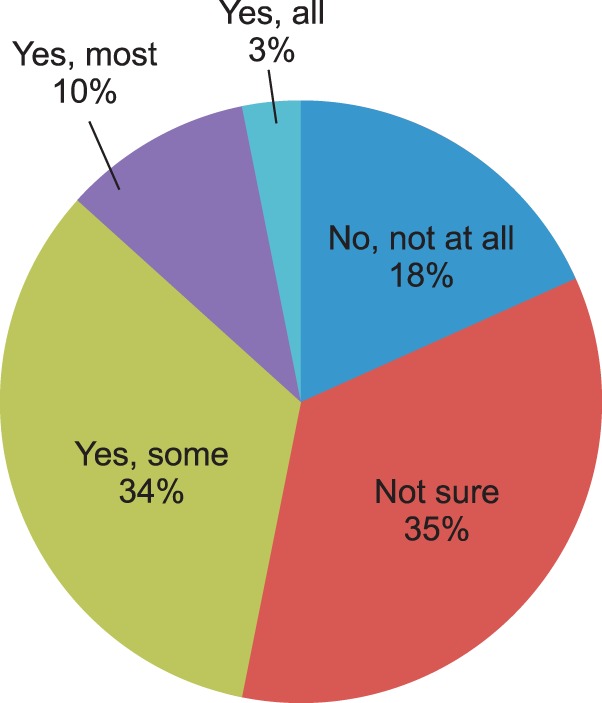
Pie chart of Question 6 responses: Do you think you would like to have your operation done using robotics or navigation? Eighteen percent would not like their surgery to involve robotics or navigation. Thirty-five percent were not sure and 47% would not mind at least some of their operation to involve robotics and navigation.
When separating the results based on age, there were a greater proportion of patients aged over 50 years that had not heard of someone having RN surgery compared with those under 50 years (70% vs. 42%, respectively). The proportion of patients correctly estimating that fewer than 10% of operations in the United Kingdom involve RN surgery were 27% and 25% for those aged under 50 years and over 50 years, respectively. Eighty-two percent of those aged under 50 years thought that RN surgery was performed at the same level or more frequently in the private sector compared to 80% of those aged over 50 years. Thirty-nine percent of those aged under 50 years thought most or all of an operation could be done with RN surgery alone compared to 33% of those aged over 50 years. Fifty-seven percent of patients aged under 50 years thought RN surgery was more accurate compared to 43% of those aged over 50 years whilst 42% of those aged under 50 years thought RN surgery made the surgeon's job easier compared to 58% aged over 50 years. Eighty-seven percent of patients aged under 50 years thought RN surgery was more expensive compared to 62% of patients aged over 50 years. Finally, 57% of patients aged under 50 years would like at least some of their surgery done by RN systems compared to 40% aged over 50 years. Applying statistical analysis to the results using chi-squared testing, there were no statistically significant differences for the responses given to questions based on the age of the patient (p > 0.05 for all questions).
DISCUSSION
This study has demonstrated that patients appear to believe that RN surgery is widely practised in the NHS, but is also largely the preserve of private practice. It has demonstrated that patients believe that RN surgery, when compared to conventional surgery, is faster and easier for the surgeon to perform. It is acknowledged that RN surgery is a more expensive practice to run. In addition, these responses do not significantly differ between different ages and sexes.
This study has confirmed a difference between what patients perceive to be the status and capabilities of RN in surgery in the United Kingdom and the actual situation. There were some differences in the pattern of responses to the questions based on the patients' age, in particular the proportion that would like to have their operation performed with RN systems and knowledge of the benefits and drawbacks of RN surgery. However, this did not have statistical significance. This may be surprising as it can be perceived that younger patients have more access to information on RN surgery. However, this may highlight the increased capabilities of older patients to search for information or that the pool of information on RN surgery is not well-known to the public.
Evidence in support of RN surgery over conventional surgery has been described in the literature. Cobb et al.5) demonstrated that postoperative outcome scores and the accuracy of bone cuts were significantly superior in robotassisted unicondylar knee replacement when compared to unicondylar knee replacement performed without robotic assistance in a prospective randomised study. Jolles et al.6) demonstrated that navigation-assisted techniques were able to accurately measure pelvic orientation during surgery and therefore significantly improve the accuracy of positioning of the acetabular cup in comparison to surgery without navigational assistance; this has also been supported by a more recent meta-analysis.7) Aspects in which RN surgery performs less favourably to conventional techniques include longer operating times and increased blood loss.2) In all of these studies, follow-up is relatively short-term and there is little data to see if such differences and clinical improvements are maintained in the long-term. It has been demonstrated that only a small percentage of TJA procedures involve RN techniques in the United Kingdom. It is likely that financial obstacles, in addition to a lack of prospective long-term clinical outcome data, are preventing the more widespread uptake of RN surgery in current practice.
It can be argued that the limitations in knowledge of RN surgery demonstrated by patients may be applied to other emerging technologies, such as customised arthroplasty implant systems and currently no studies exist to explore patient knowledge in these areas. It has been demonstrated that direct-to-consumer marketing of orthopaedic implants has a significant influence over patient knowledge and decision-making with respect to TJA surgery.8) It is possible that, in the future, such marketing may further shape patient knowledge and expectations of an array of emerging technologies, all of which will present greater challenges to the clinician trying to allow their patients to make informed decisions and improve their satisfaction.
The limitations of this study include a relatively small sample size largely comprising of a predominantly urban population. The questionnaire was handed out in a single clinic, although the patients were representative of our normal population group and would not likely differ significantly from our general population. We did not include any patients that could not understand the questionnaire from not speaking English, but this only excluded a negligible portion of our clinics and would not have influenced the trend in responses. In our study, robotics and navigation systems have been treated as a common item; from a surgical and economic perspective, they are vastly different. However, we chose not to differentiate in order to reduce potential confusion from our subject and thus compliance with the questionnaire. It is possible that a more rural-based population may have a different preexisting knowledge of RN surgery in orthopaedics. Furthermore, it is not clear as to the pre-existing knowledge level of this particular group of patients; those who had more knowledge on the subject may have given different responses in comparison to those who had little knowledge on the subject. Future versions of this study may include occupation status and education level to provide further stratification of results. As the centre did not routinely perform RN surgery, different results may have been seen in centres and under consultants for whom RN surgery is routinely practised. Finally, the questionnaires were not comprehensively piloted and therefore further studies may be required to validate their reproducibility.
In conclusion, patients' knowledge of the prevalence, benefits and limitations of RN surgery in orthopaedics shows a significant difference to the current practice. This study highlights the clear need to educate patients on the merits and drawbacks of RN and indeed other emerging technologies in order to realign expectations and improve levels of satisfaction.
ACKNOWLEDGEMENTS
With thanks to Nick Marson, medical student, for help in distribution of questionnaire and compilation of results.
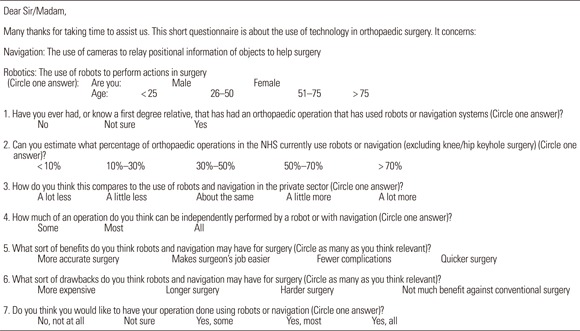
Appendix
Appendix 1
Questionnaire Handed to Patients
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.National Joint Registry [Internet] Hemel Hempstead: National Joint Registry; c2008-2014. [cited 2014 Aug 30]. Available from: http://www.njrcentre.org.uk. [Google Scholar]
- 2.Lang JE, Mannava S, Floyd AJ, et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br. 2011;93(10):1296–1299. doi: 10.1302/0301-620X.93B10.27418. [DOI] [PubMed] [Google Scholar]
- 3.Lavernia CJ, Contreras JS, Parvizi J, Sharkey PF, Barrack R, Rossi MD. Do patient expectations about arthroplasty at initial presentation for hip or knee pain differ by sex and ethnicity? Clin Orthop Relat Res. 2012;470(10):2843–2853. doi: 10.1007/s11999-012-2431-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamilton DF, Lane JV, Gaston P, et al. What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. BMJ Open. 2013;3(4):e002525. doi: 10.1136/bmjopen-2012-002525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cobb J, Henckel J, Gomes P, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br. 2006;88(2):188–197. doi: 10.1302/0301-620X.88B2.17220. [DOI] [PubMed] [Google Scholar]
- 6.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;(426):174–179. doi: 10.1097/01.blo.0000141903.08075.83. [DOI] [PubMed] [Google Scholar]
- 7.Gandhi R, Marchie A, Farrokhyar F, Mahomed N. Computer navigation in total hip replacement: a meta-analysis. Int Orthop. 2009;33(3):593–597. doi: 10.1007/s00264-008-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bozic KJ, Smith AR, Hariri S, et al. The 2007 ABJS Marshall Urist Award: the impact of direct-to-consumer advertising in orthopaedics. Clin Orthop Relat Res. 2007;458:202–219. doi: 10.1097/BLO.0b013e31804fdd02. [DOI] [PubMed] [Google Scholar]


