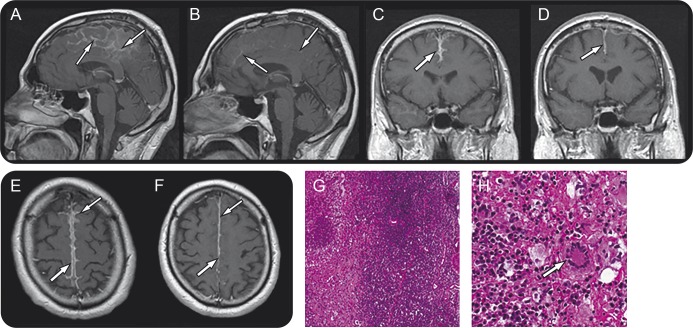
A 44-year-old man with a 20-year history of seropositive erosive rheumatoid arthritis (RA), diagnosed according to the American Rheumatology Association revised criteria,1 was referred for severe headache and partial simple motor seizures. At the time of presentation, his disease was inactive under a stable dose of methylprednisolone (8 mg/day). The neurologic examination was normal: there were no cranial nerve palsies, sensory motor deficits, gait imbalance, impairment of cognitive functions, or neck stiffness. Fundoscopy did not reveal any abnormality. The major finding on neuroimaging was a marked leptomeningeal enhancement (figure, A, C, and E). CSF analysis showed a normal opening pressure, normal cell count, and a slightly increased immunoglobulin G index; viral markers and culture studies were unremarkable. Biopsy specimen displayed necrotizing granulomatous inflammation of leptomeninges without pachymeningeal involvement (figure, G and H). IV methylprednisolone was prescribed (1 g/day for 3 days) followed by methotrexate in order to enhance immunosuppression and avoid an increase of the steroid load; favorable clinical and radiologic responses were observed (figure, B, D, and F).
Figure. Leptomeningeal inflammation.
Postcontrast T1-weighted MRI: abnormal leptomeningeal enhancement over the frontoparietal lobes and interhemispheric fissure before (A, C, E) and after (B, D, F) 3-month methotrexate treatment. Histopathology (G and H): necrotizing granulomas involving the leptomeninges surrounded by mononuclear inflammatory cells and focal giant cell reaction (arrow) without signs of vasculitis. Hematoxylin & eosin stains (×4, ×20).
Chronic meningitis may be due to infections, neoplasms, drugs, sarcoidosis, and autoimmune diseases.2 The involvement of meninges by inflammatory cells in RA may assume the form of leptomeningitis and/or pachymeningitis. Although the real prevalence is unknown, this condition is quite uncommon: only a few histopathologically proven cases have been described and the exact pathogenesis still remains unclear.3 Rheumatoid meningitis may develop in early or late stages as well as in active or inactive phases of the disease, and it may even precede synovial manifestations. The clinical phenotype may be heterogeneous: headache and cranial nerve palsies are usually associated with pachymeningeal invasion, whereas altered consciousness, psychiatric symptoms, sensory or motor deficits, and seizures are often the initial symptoms of leptomeningitis. CSF may reveal increased protein or lymphocytic pleocytosis, or it may be normal. Characteristic, although not specific, MRI findings include diffuse or patchy enhancement of leptomeninges and/or pachymeninges.4 The final diagnosis relies on histopathologic examination, which may display 3 different patterns: rheumatoid nodules, nonspecific meningeal inflammation, or vasculitis.5
Given the rarity of the condition, no formally established guidelines or standardized treatments are available to date. Successful treatment approaches usually include immunosuppressive therapies: corticosteroids, cyclophosphamide, azathioprine, or methotrexate have been variably recommended.6 Clinical improvements were reported with glucocorticoid treatment alone, suggesting that additional cytotoxic immunosuppressive agents may not be required in the induction phase. However, these may be useful as a steroid-sparing strategy to achieve tapering or cessation of steroids and reduce or avoid their long-term side effects. On the other hand, immunosuppressors alone might represent a potential alternative treatment option when glucocorticoids are contraindicated, as in a single case successfully managed with cyclophosphamide.7
Although rheumatoid meningitis is extremely rare, it should be taken into account when patients affected by RA, even in an inactive stage, develop signs or symptoms suggestive of CNS involvement in order to avoid treatment delay and prevent neurologic sequelae.
Acknowledgments
Acknowledgment: The authors thank Dr. Francesco Sessa (Department of Neuroradiology, University Hospital of Ancona, Italy) and Dr. Sara Zagaglia (Neurological Clinic, University Hospital of Ancona, Italy) for editing assistance.
Footnotes
Author contributions: All authors contributed to writing and editing this case study.
Study funding: No targeted funding reported.
Disclosure: S. Lattanzi, C. Cagnetti, P. Di Bella, and M. Scarpelli report no disclosures. M. Silvestrini is an associate editor for Journal of Alzheimer's Disease. L. Provincialli reports no disclosures. Go to Neurology.org/nn for full disclosures. The Article Processing Charge was paid by the Department of Experimental and Clinical Medicine, Marche Polytechnic University.
References
- 1.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–324. [DOI] [PubMed] [Google Scholar]
- 2.Hildebrand J, Aoun M. Chronic meningitis: still a diagnostic challenge. J Neurol 2003;250:653–660. [DOI] [PubMed] [Google Scholar]
- 3.Gotkine M, Vaknin-Dembinsky A. Neurologic manifestations of systemic immunopathological diseases. Curr Treat Options Neurol 2012;14:276–292. [DOI] [PubMed] [Google Scholar]
- 4.Jones SE, Belsley NA, McLoud TC, Mullins ME. Rheumatoid meningitis: radiologic and pathologic correlation. Am J Roentgenol 2006;186:1181–1183. [DOI] [PubMed] [Google Scholar]
- 5.Bathon JM, Moreland LW, Di Bartolomeo AG. Inflammatory central nervous system involvement in rheumatoid arthritis. Semin Arthritis Rheum 1989;18:258–266. [DOI] [PubMed] [Google Scholar]
- 6.Kato T, Hoshi K, Sekijima Y, et al. Rheumatoid meningitis: an autopsy report and review of the literature. Clin Rheumatol 2003;22:475–480. [DOI] [PubMed] [Google Scholar]
- 7.Shimada K, Matsui T, Kawakami M, et al. Diffuse chronic leptomeningitis with seropositive rheumatoid arthritis: report of a case successfully treated as rheumatoid leptomeningitis. Mod Rheumatol 2009;19:556–562. [DOI] [PubMed] [Google Scholar]