Abstract
Objectives
The purpose of this study was to assess the long-term results of endoscopic dilatation of airway stenosis and to evaluate predictive factors for favorable results.
Methods
Fifty-four patients with tracheal and subglottic stenosis who underwent endoscopic dilatation with at least 12 months follow-up were enrolled in this study. We evaluated predictive factors for final treatment outcome such as stenosis length, location, characteristics, procedure type, and the severity of stenosis.
Results
The final outcome of endoscopic dilatation showed a cure rate of 40.7%, improvement rate of 46.3%, and failure rate of 13.0%. Patients with mild stenosis or a shorter stenotic segment and those who underwent a touch-up procedure following tracheal resection with end-to-end anastomosis showed better outcomes. The cure rate of endoscopic dilatation for patients with shorter mild stenosis was 72.2%.
Conclusion
Endoscopic dilatation may be a primary treatment modality for patients with airway stenosis characterized by mild severity and a short stenotic segment.
Keywords: Endoscopic dilatation, Tracheal stenosis, Subglottic stenosis
INTRODUCTION
Currently, the standard treatment of airway stenosis is resection and end-to-end anastomosis. Although end to end anastomosis has shown a higher success rate than endoscopic dilatation, the role of endoscopic dilation for airway stenosis has expanded gradually because of its minimal invasiveness and reversibility [1]. The final success rate for airway stenosis vary between 40% and 80% [2,3].
Shapshay et al. [4] first introduced endoscopic dilatation using a CO2 laser for patients with tracheal stenosis at 1987. The role has expanded during the past two decades [5]. Additionally, endoscopic dilatation using cold instruments with mitomycin-C was introduced recently for the management of tracheal stenosis [6].
Intial endoscopic management of chronic laryngotracheal stenosis has been advocated over the conventional open surgical technique for special situations [7]. However, fewer reports and no long-term follow-up data regarding predictive factors are available.
The purpose of this study was to demonstrate the long-term results of endoscopic dilatation for airway stenosis and to identify predictive factor of favorable outcomes.
MATERIALS AND METHODS
Patients
Fifty-four consecutive patients with tracheal and/or subglottic stenosis following endoscopic dilatation from March 2005 to January 2012 at Soonchunhyang University Bucheon Hospital were included and followed up for at least 12 months postoperatively. All medical records were reviewed retrospectively and the Institutional Review Board approved the study protocol (SCHBC_IRB_10_51).
Most enrolled patients had tracheal and/or subglottic stenosis and a poor general condition or were high-surgical-risk patients. We retrospectively analyzed specific parameters, including preoperative and postoperative stenosis grade, cause of stenosis, vertical length of stenotic segment, and characteristics and locations of stenosis, based on the endoscopic findings and medical records.
Operative techniques
The principles of our endoscopic dilatation were focused on maximal preservation of the tracheal mucosa and minimal trauma during procedure.
First, we evaluated the location and severity of stenosis. The characteristics of stenotic lesion and the vertical length of the stenotic segment were also measured by endoscopy.
To prevent thermal injury, we used cold instruments, such as microscissors or a knife, instead of a CO2 laser, because a laser may induce thermal injury to the surrounding mucosa and a higher rate of restenosis. Before mechanical dilatation, a radial incision was made at 3, 9, and 12 o'clock. Mechanical dilatation was performed using an esophageal bougie or esophageal baloon dilators (Boston Scientific Co, Marlborough, MA, USA). An intralesional steroid injection (triamcinolone 40 mg/mL; Hanall Inc., Seoul, Korea) into the stenotic segments was performed, and mitomycin C (0.4 mg/mL; Kyowa Hakko Kirin Korea Co., Seoul, Korea) was applied for 4 minutes to prevent restenosis (Fig. 1).
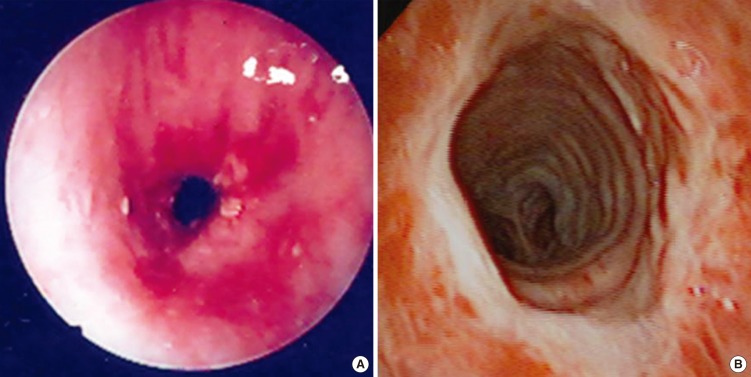
Fig. 1.
Endoscopic views following endoscopic dilatation with subglottic stenosis. (A) Preoperative endoscopic views of subglottic stenosis. (B) Immediate endoscopic views following endoscopic dilatation.
Stenosis grade and assessment of treatment outcome
All patients underwent airway evaluation following dilatation by single surgeon (SWL) with a flexible laryngoscope under topical anesthesia at an outpatient clinic during each follow-up. The severity of stenosis was described based on the Myer-Cotton classification. The grade I, luminal narrowing of <50%; grade II, luminal obstruction of 51%-70%; grade III, luminal obstruction of 71%-90%; and grade IV, luminal obstruction of 100% (virtually no lumen) [8].
The treatment outcome was determined based on the definition of Shapshay et al. [4], considering the grade of stenosis, symptom improvement, and decannulation.
Postoperative subjective symptoms were described based on patient's symptoms following procedure such as no, mild, and moderate/severe limitations on daily life. A cure was defined when a patient's subjective symptoms and objective stenosis grades dramatically improved and decannulation of the tracheotomy tube was achieved. Improvement was defined as improvement in subjective symptoms and objective stenosis grades but with the inability to decannulate the tracheotomy tube. Failure was defined as no improvement in subjective symptoms and objective stenosis grades following endoscopic dilatation.
Statistical analysis
Statistical analyses (SPSS ver. 12.0; SPSS Inc., Chicago, IL, USA) were performed using the paired t-test and chi-square test. P-values of <0.05 were considered to indicate statistical significance.
RESULTS
Demographic data are shown in Table 1. Of the 54 patients, 40 (74.1%) were male and the average age was 51.7±19.8 years (range, 9 to 79 years). Underlying comorbidities included cerebrovascular accidents in 53.7% (29/54), chronic obstructive lung disease in 18.5% (10/54), diabetes mellitus in 7.4% (4/54), and malignancies in 5.6% (3/54). Among all patients, only 14.8% (8/54) had no other chronic debilitating underlying comorbidities. The most common cause of airway stenosis was a tracheotomy (32/54, 59.3%), followed by prolonged intubation (22/54, 40.7%). Other causes included endobronchial tuberculosis in three patients, an inhalation burn in one, and an emergency cricothyroidotomy in one. The average follow-up duration was 26.5±13.7 months (range, 12 to 78 months).
Table 1.
Demographic data of 54 airway stenosis patients
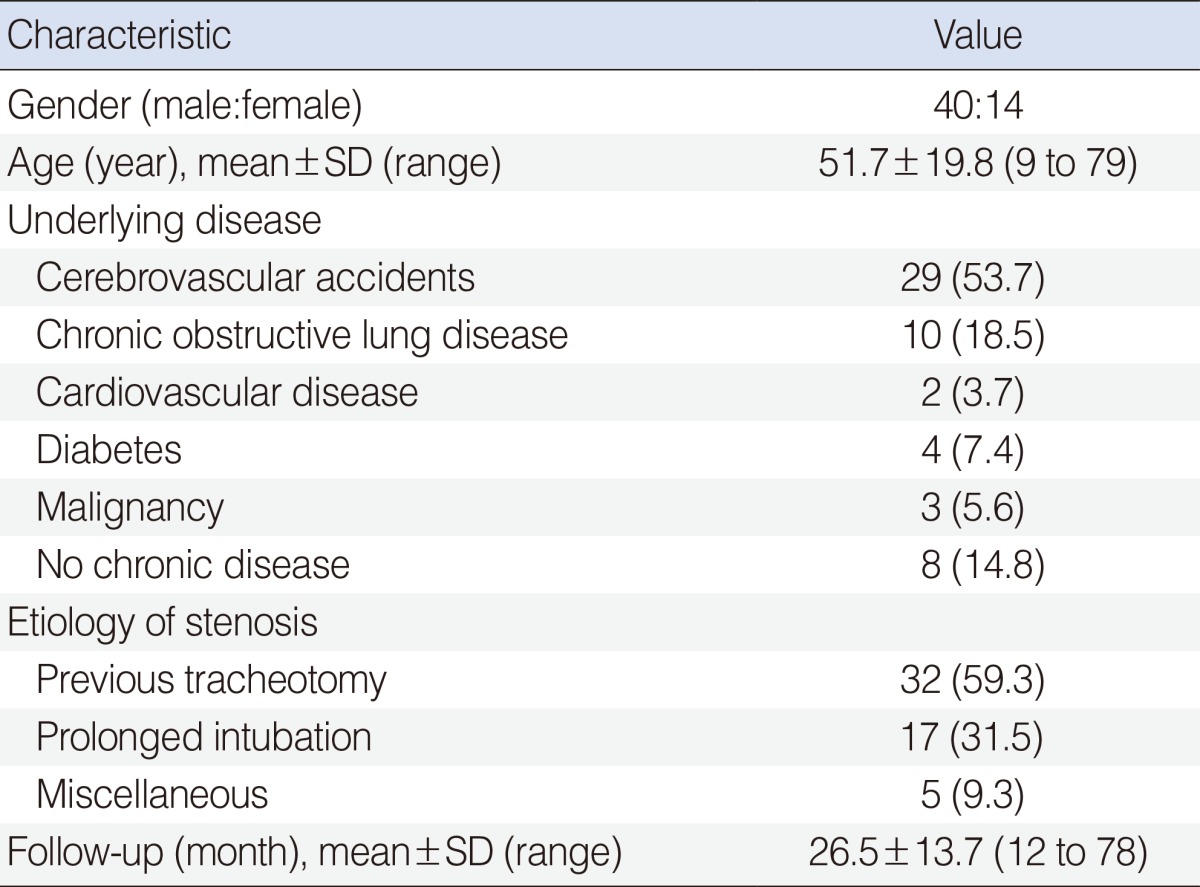
Values are presented as number (%).
The features of the endoscopic dilatation are shown in Table 2. The time interval from symptom occurrence to endoscopic intervention was 2.0±0.7 months. Among the 54 patients, airway stenosis was due to tracheal stenosis in 61.1% (33/54) of patients, subglottic stenosis 22.2% (12/54), and combined stenosis 16.7% (9/54). In total, 15 patients had grade I stenosis; 20, grade II; 14, grade III; and 5, grade IV. The characteristics of the stenotic lesion were fibrotic in 39 (72.2%), granulomatous in 13 (24.1%), and mixed in two patients (3.7%). In total, 48 patients (88.9%) underwent curative endoscopic dilatation and the other patients (7.4%) had a touch-up procedure. The average vertical length of the stenotic segment was 1.9±1.0 cm (range, 0.5 to 4.2 cm), and the average number of interventions was 1.4±0.8 times (range, 1 to 4 times). Regarding repeated interventions, 16 of the 54 patients (29.2%) needed multiple endoscopic dilatation; the rest underwent a single intervention; the mean number of procedures was 1.4±0.8 (range, 1 to 4).
Table 2.
Features of endoscopic dilatation
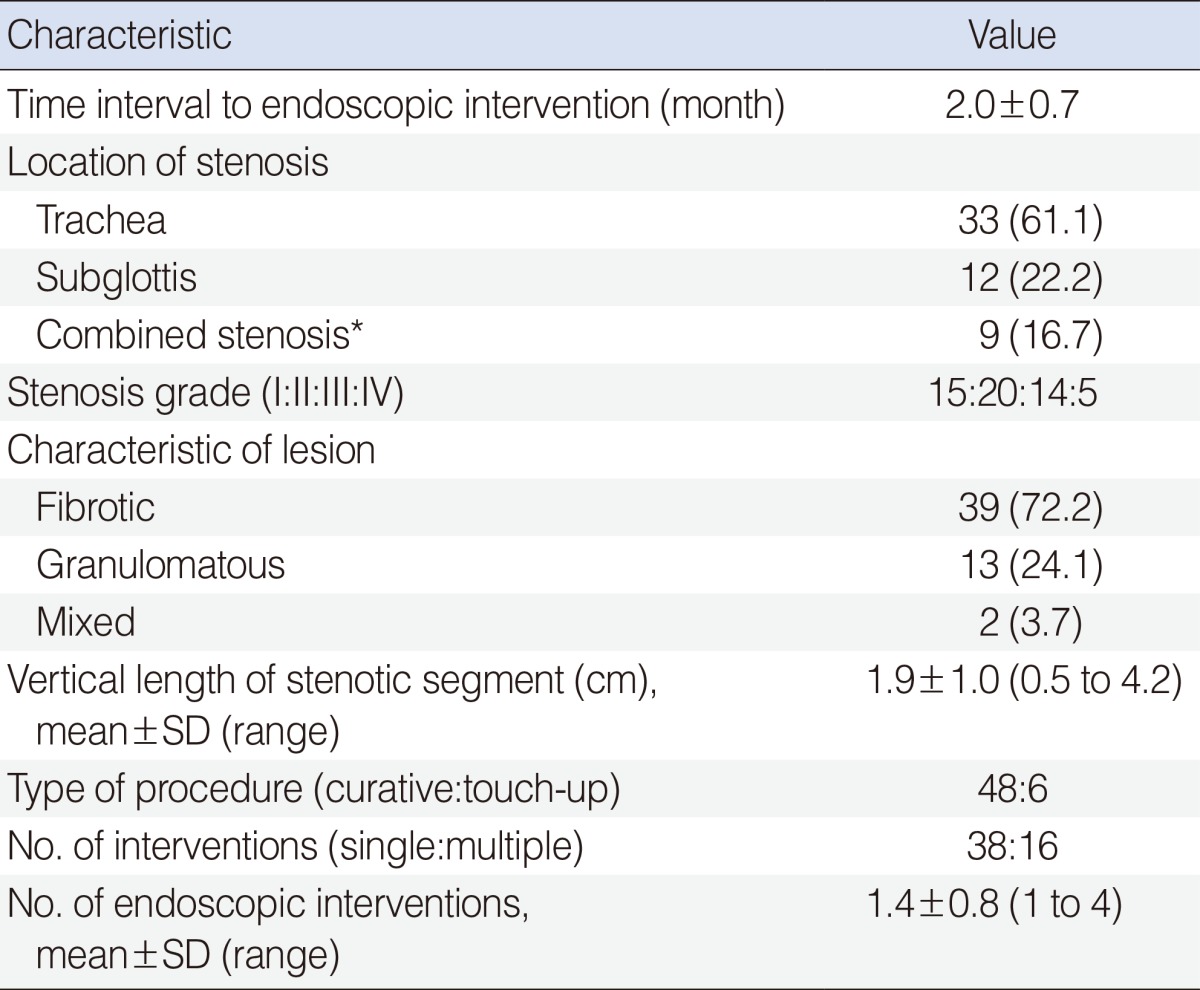
Values are presented as number (%).
*Combined tracheal and subglottic stenosis.
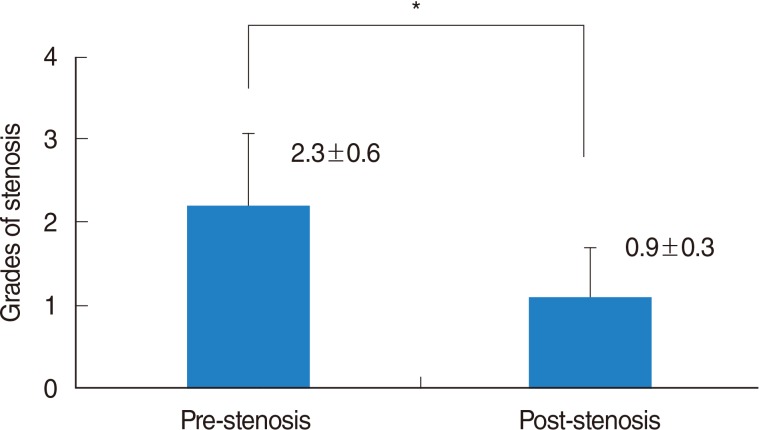
The average grade of stenosis improved significantly, from 2.3±0.6 to 0.9±0.3 following endoscopic dilation (P<0.05) (Fig. 2). Final treatment outcome based on the endoscopic findings and patient symptoms were a cure rate of 40.7% (22/54), an improvement rate of 46.3% (25/54), and a failure rate of 13.0% (7/54) (Table 3). Seven patients showed no improvement, or even aggravation, of airway stenosis despite the procedure. These patients were treated with tracheal resection with end to end anastomosis (TREE) or cricotracheal resection with end to end anastomosis (CTR) (57.2%, 4/7), airway stenting (28.6%, 2/7), and laryngotracheal reconstruction with costal cartilage (14.3%, 1/7).
Fig. 2.
Preoperative and postoperative airway stenosis grades following endoscopic dilatation. Pre-stenosis, grades of preoperative airway stenosis; Post-stenosis, grades of postoperative airway stenosis. *P<0.05.
Table 3.
Final outcomes of endoscopic dilatation (n=54)
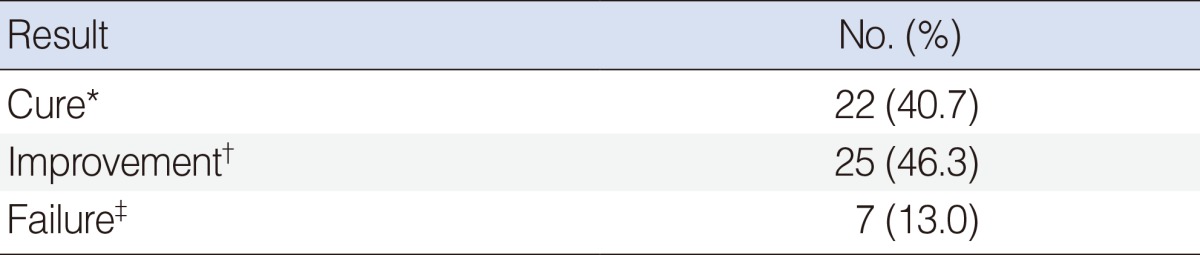
*Patient's subjective symptoms and objective stenosis grade dramatically improved, and decannulation of the tracheostomy tube was finally achieved. †Patient's subjective symptoms and objective stenosis grades improved, but decannulation of the tracheostomy tube was not possible. ‡Patient's subjective symptoms and objective stenosis grades did not improve following endoscopic dilatation.
Complications related to endoscopic dilatation were as follows: no complication, 88.8% (48/54); postoperative airway obstruction due to edema, 5.6% (3/54); postoperative bleeding, 1.9% (1/54); sinus bradycardia, 1.9%; and aspiration pneumonia, 1.9%.
Factors that were independently associated with favorable final outcome on the basis of a multinomial regression model are shown in Table 4: the severity of stenosis, length and location of the stenosis, and type of procedure were the independent predictors of favorable results (P<0.05). However, gender, number of interventions, and characteristics of the stenosis showed no statistically significant association (P>0.05). This means that patients with mild, shorter, and isolated airway stenosis will have better final outcomes than those with more severe, longer, and combined stenosis. Actually, 72.2% of patients with mild, shorter and isolated stenosis can be treated by endoscopic procedures only.
Table 4.
Predictive factors related to favorable final results following endoscopic dilatation
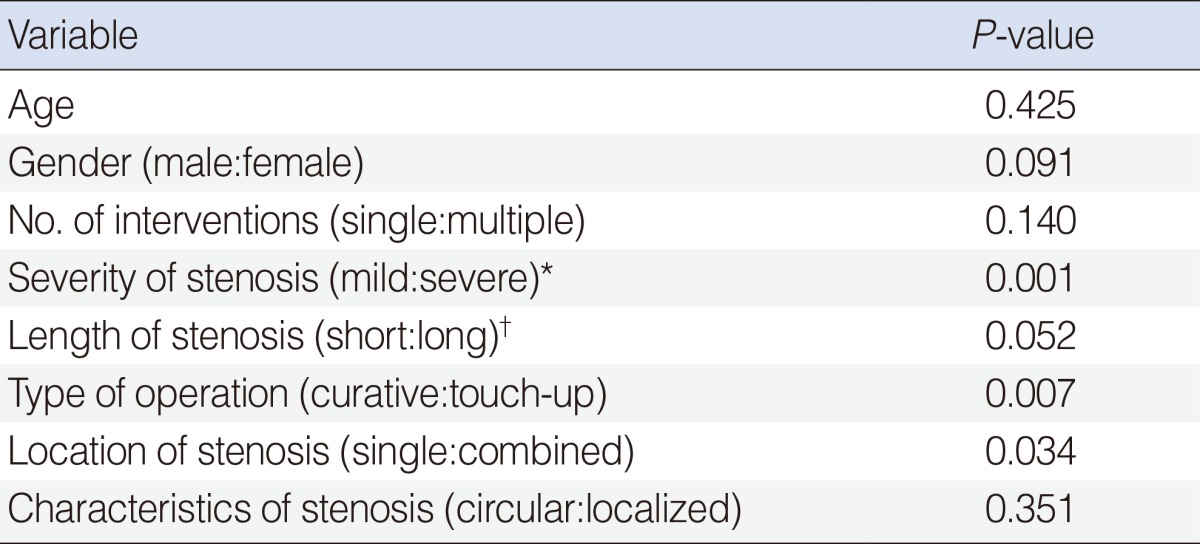
*Mild, grade of I or II; severe, grade of III or IV by Myer-Cotton classification. †Short, length of stenotic segment was ≤1.5 cm; long, >1.5 cm.
DISCUSSION
Surgical treatment of airway stenosis can be divided into two modalities: endoscopic intervention and conventional open airway surgery. However, the selection of proper treatment remains controversial and is usually determined based on the general condition of the patient, location and length of stenosis, and the preference of the surgeon [3].
Although conventional TREE and CTR can correct more severe stenosis with high decannulation rates, the role of endoscopic dilation for airway stenosis has expanded because of its minimal invasiveness and reversibility [3].
Endoscopic dilatation is usually preferred in patients with mild stenosis of grade I or II and a stenotic segment of <1 cm. It is especially preferred in patients with a high surgical risk and poor general condition [1,3]. But, it is not effective for circumferential scarring, longer stenotic segments, or loss of cartilage support [9].
Although this study was retrospective in design but the average follow-up was 26.5±13.7 months, this is sufficient duration to assess the long-term outcomes and prognostic factors of endoscopic dilatation.
Among several factors, stenosis severity, location (isolated or combined), and procedure type (touch-up or curative procedure) were significantly associated with the final treatment outcome.
The cure rate was 40.7% and improvement rate was 46.3% (overall improvement, 87%). This procedure was especially effective for shorter, mild stenotic segments and isolated stenosis (cure rate, 72.2%). This indicates that accurate assessment of tracheal stenosis and proper selection of patients are important factors for predicting the postoperative outcome. Successful endoscopic dilatation may be achieved with proper selection, and a significant number of patients with grades I and II stenosis can be improved to a near-normal airway by endoscopic means without undergoing conventional open procedure.
In this study, most patients had underlying chronic comorbidities such as cerebrovascular accidents, chronic obstructive pulmonary disease, and cancer. For these patients, who are at high surgical risk for conventional open surgery, endoscopic procedure may be a good alternative.
If proper selection of patients were guaranteed, endoscopic dilatation of airway stenosis could be the first or adjunctive treatment modality for those with a poor general condition when open general surgery is not tolerated and in patients with restenosis of the anastomosis site following TREE and CTR.
Notably, touch-up procedures showed significantly higher success rates than primary curative endoscopic procedure in this study. Therefore, when patients showed re-stenosis at the anastomosis site following TREE and CTR, endoscopic dilatation could be a useful adjunct treatment that will aid optimizing the final result [10].
Based on this long-term follow-up results, endoscopic dilatation for tracheal or subglottic stenosis could improve the grades of stenosis and showed the better outcomes in patients with mild stenosis and shorter stenotic segments.
ACKNOWLEDGMENTS
This work was supported by the Soonchunhyang University Research Fund.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Mandour M, Remacle M, Van de Heyning P, Elwany S, Tantawy A, Gaafar A. Chronic subglottic and tracheal stenosis: endoscopic management vs. surgical reconstruction. Eur Arch Otorhinolaryngol. 2003 Aug;260(7):374–380. doi: 10.1007/s00405-002-0578-3. [DOI] [PubMed] [Google Scholar]
- 2.Schweinfurth JM. Endoscopic treatment of severe tracheal stenosis. Ann Otol Rhinol Laryngol. 2006 Jan;115(1):30–34. doi: 10.1177/000348940611500105. [DOI] [PubMed] [Google Scholar]
- 3.Yamamoto K, Kojima F, Tomiyama K, Nakamura T, Hayashino Y. Meta-analysis of therapeutic procedures for acquired subglottic stenosis in adults. Ann Thorac Surg. 2011 Jun;91(6):1747–1753. doi: 10.1016/j.athoracsur.2011.02.071. [DOI] [PubMed] [Google Scholar]
- 4.Shapshay SM, Beamis JF, Jr, Hybels RL, Bohigian RK. Endoscopic treatment of subglottic and tracheal stenosis by radial laser incision and dilation. Ann Otol Rhinol Laryngol. 1987 Nov-Dec;96(6):661–664. doi: 10.1177/000348948709600609. [DOI] [PubMed] [Google Scholar]
- 5.Monnier P, George M, Monod ML, Lang F. The role of the CO2 laser in the management of laryngotracheal stenosis: a survey of 100 cases. Eur Arch Otorhinolaryngol. 2005 Aug;262(8):602–608. doi: 10.1007/s00405-005-0948-8. [DOI] [PubMed] [Google Scholar]
- 6.Simpson CB, James JC. The efficacy of mitomycin-C in the treatment of laryngotracheal stenosis. Laryngoscope. 2006 Oct;116(10):1923–1925. doi: 10.1097/01.mlg.0000235934.27964.88. [DOI] [PubMed] [Google Scholar]
- 7.Nouraei SA, Singh A, Patel A, Ferguson C, Howard DJ, Sandhu GS. Early endoscopic treatment of acute inflammatory airway lesions improves the outcome of postintubation airway stenosis. Laryngoscope. 2006 Aug;116(8):1417–1421. doi: 10.1097/01.mlg.0000225377.33945.14. [DOI] [PubMed] [Google Scholar]
- 8.Cotton RT. Pediatric laryngotracheal stenosis. J Pediatr Surg. 1984 Dec;19(6):699–704. doi: 10.1016/s0022-3468(84)80355-3. [DOI] [PubMed] [Google Scholar]
- 9.Bailey M, Hoeve H, Monnier P. Paediatric laryngotracheal stenosis: a consensus paper from three European centres. Eur Arch Otorhinolaryngol. 2003 Mar;260(3):118–123. doi: 10.1007/s00405-002-0526-2. [DOI] [PubMed] [Google Scholar]
- 10.Bent JP, Shah MB, Nord R, Parikh SR. Balloon dilation for recurrent stenosis after pediatric laryngotracheoplasty. Ann Otol Rhinol Laryngol. 2010 Sep;119(9):619–627. doi: 10.1177/000348941011900909. [DOI] [PubMed] [Google Scholar]