Gareth Evans et al. in a recent article in the journal [http://www.ncbi.nlm.nih.gov/pubmed/24687378] concluded that survival from breast cancer in very high risk women is better in screened versus unscreened women with or without a demonstrated genetic cause, and that BRCA2 mutation carriers may benefit from MRI screening in addition to mammography (Mx). However, this may not be the case for BRCA1 mutation carriers. Their dataset included no more than 27 and 24 BRCA1 breast cancer cases detected through Mx or MRI, respectively. We recently reported survival in BRCA1 mutation carriers diagnosed with breast cancer through annual Mx and MRI [http://www.ncbi.nlm.nih.gov/pubmed/23615785]. The main finding was that despite detecting tumours at an early stage, survival was inferior to what might have been expected according to Kurian et al. [http://www.ncbi.nlm.nih.gov/pubmed/22231042]. Referring to our results, Evans et al. state in their discussion that ‘.. formal evidence for a survival advantage (for MRI versus mammography alone) has not so far been published’.
In order to make our data for patients followed at the outpatient clinic at Oslo University Hospital available to all, we here present updated survival analysis in the MRI series previously reported (MRI series), and compare that series to survival in BRCA1 breast cancer cases detected through annual screening with mammography without MRI (Mx series).
Our selection, methods and ethics were described in our recent publication mentioned above. The Mx series were the prospectively detected breast cancer cases before MRI was added to the protocol for BRCA1 mutation carriers in 2001, and those subjected to annual Mx alone based on family history before their BRCA1 mutations were detected subsequently. In contrast to our previous report, only patients not having had any cancer before or at first planned examination were included in the present analysis.
We diagnosed 6 carcinoma in situ in the Mx series and 3 in the MRI series.
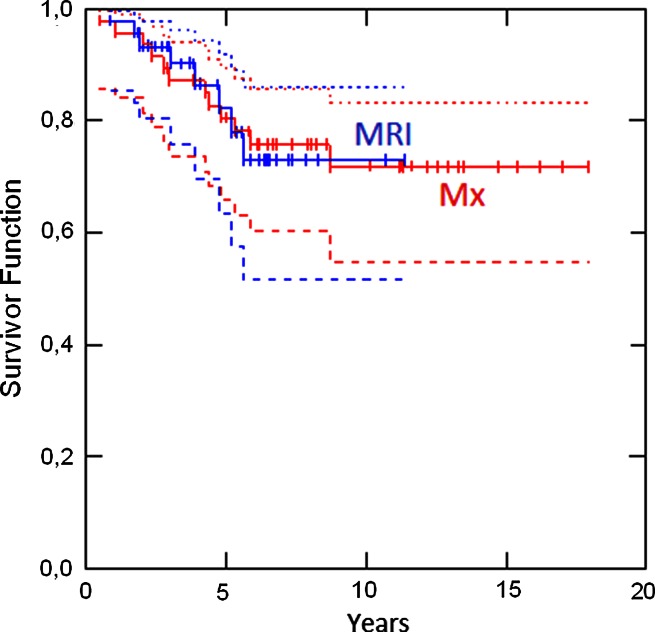
Kaplan–Meier survival analyses were performed in the 47 invasive cancer cases detected in the Mx series among whom 12 had died, and in the 45 invasive cancer cases in the MRI series among whom 8 had died. None of the deceased had any other cancers. 5- and 10-years survival was 0.81 (95 % CI 0.63–0.88) and 0.72 (95 % CI 0.60–0.86), respectively, in the Mx series, compared to 0.82 (95 % CI 0.63–0.92) and 0.73 (95 % CI 0.52–0.86) in the MRI series (Fig. 1).
Fig. 1.
Survival in the MRI and Mx series with 95 % CIs
Age (grouped as <50 years/> = 50 years), tumour size (<=10 mm/11–20 mm/> 20 mm), nodal spread (yes/no), ER, PR and grade were compared with survival through Cox proportional hazard models in the combined series. None gave significant results for univariate analyses (p ≥ 0.18 for any), nor for multivariate analyses (p ≥ 0.24).
The findings in this larger series than the one reported by Gareth Evans et al. support their notion that there may be no additional survival benefit from early diagnosis through MRI compared to Mx for BRCA1 mutation carriers: As previously reported, tumours did appear to be downstaged in the MRI series compared to the Mx series—but the expected improved survival was not observed, and there was no association with survival and stage at diagnosis, which would have been expected if the earlier stage at diagnosis in the MRI series were to be associated with better prognosis. Prevalence of carcinoma in situ was low in both series. Time-trends in treatment are potential confounders to survival studies recruiting patients over many years: The MRI cases were treated in more recent years than the Mx cases and would have been expected to have improved survival because of that, nonetheless this was not found. We had expected a right-shift in the survival curve for the MRI series reflecting the earlier diagnosis even in the absence of a ‘true’ improved survival; however, this was not found. Our population has specific founder BRCA1 mutations, and the female carriers may be subjected to different environment factors compared to carriers in other populations.
We had no control group without screening, and our results are not in conflict with the conclusion by Gareth Evans et al. that early diagnosis and treatment may be associated with improved survival. Our results address the putative benefit of adding MRI to annual Mx, for which none was apparent.
We look forward to reports from other groups on the observed survival related to early diagnosis with MRI in BRCA1 mutation carriers, because despite our series being the largest reported so far, we are still short of patients included to be sure that results are not caused by chance variation based on limited numbers.