Dear Editor
Uveal melanoma (UM) is the most common primary intraocular malignancy and can be categorized into prognostically significant subgroups based on gene expression profile (GEP): class 1 tumors have a low risk and class 2 tumors have a high risk for metastasis [1]. One of the most common treatments for UM is I-125 episcleral plaque radiotherapy. To identify factors associated with response to radiotherapy, we studied a cohort of 281 consecutive UM patients who underwent GEP molecular classification at the time of plaque placement. The study was approved by the Institutional Review Board at the University of Miami. In this letter, we describe a distinct subset of 9 (3%) patients who demonstrated rapid tumor regression associated with transient tumor inflammation and uveitis (Figure 1). The patients included 4 women and 5 men, with a mean age of 54.1 years (median 54 years), mean initial tumor diameter of 13.3 mm (median 13.0 mm), and mean initial tumor thickness of 6.9 mm (median 6.6 mm). Remarkably, all 9 of these patients had a class 1 primary uveal melanoma. Since 162 (58%) patients from the entire cohort had a class 1 tumor, the likelihood of all 9 (100%) patients with acute inflammatory tumor regression having a class 1 tumor by chance is 1 in 1000 (Fisher exact test).
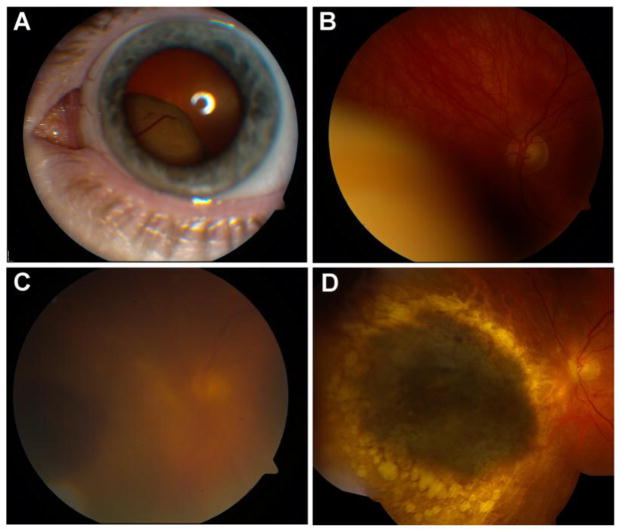
Fig. 1.
A 48-year-old woman had a large uveal melanoma with basal dimensions 12 mm × 11 mm, and height of 10.6 mm. Fine-needle aspiration biopsy of the tumor was performed at the time of Iodine-125 plaque radiotherapy, revealing a class 1 gene expression profile. Sixty-nine months post-treatment, the patient remains metastasis free. Baseline tumor findings seen on external (A) and fundus examination (B). C: One week following I-125 plaque radiotherapy, she developed pain and was found to have a significant uveitic response with vitritis. D: Two years after plaque radiotherapy, the tumor is completely flat with no residual uveitis
Previous reports have linked rapid post-radiation regression of uveal melanomas with a higher risk of metastastic disease [2]. More recent reports have found no association between post-radiation regression rates and GEP prognostic class [3,4]. However, none of these earlier studies identified a subset of patients described here with rapid tumor regression due to post-radiation inflammatory response. Thus, our findings are not contradictory to earlier studies but describe a newly recognized subset.
Class 1 tumors are distinguished from class 2 tumors by their sustained expression of melanocytic differentiation antigens that are down-regulated in the stem cell-like class 2 tumors [5]. It is these differentiation-associated proteins that are most commonly recognized by the immune system in cases of successful immunotherapy in melanoma [6]. Although this study is limited by its retrospective design and small sample of patients with rapid regression, the results suggest that class 1 tumors may be more immunogenic than class 2 tumors following I-125 brachytherapy.
Footnotes
Conflict of Interest Statement
Dr. Harbour is the inventor of intellectual property used in the study and receives royalties from its commercialization. He is a paid consultant for Castle Biosciences, licensee of intellectual property presented in this article. Dr. Chen certifies that he has NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- 1.Harbour JW, Chen R. The DecisionDx-UM Gene Expression Profile Test Provides Risk Stratification and Individualized Patient Care in Uveal Melanoma. PLoS Curr. 2013 doi: 10.1371/currents.eogt.af8ba80fc776c8f1ce8f5dc485d4a618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Augsburger JJ, Gamel JW, Shields JA, Markoe AM, Brady LW. Post-irradiation regression of choroidal melanomas as a risk factor for death from metastatic disease. Ophthalmology. 1987;94:1173–1177. doi: 10.1016/s0161-6420(87)33310-x. [DOI] [PubMed] [Google Scholar]
- 3.Correa ZM, Augsburger JJ. Relationship between rate of posterior uveal melanoma flattening following plaque radiotherapy and gene expression profile class of tumor cells. Invest Opthalmol Vis Sci. 2014;55:556–559. doi: 10.1167/iovs.13-13381. [DOI] [PubMed] [Google Scholar]
- 4.Chappell MC, Char DH, Cole TB, Harbour JW, Mishra K, Weinberg VK, Phillips TL. Uveal melanoma: molecular pattern, clinical features, and radiation response. Am J Ophthalmol. 2012;154:227–232. doi: 10.1016/j.ajo.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Onken MD, Ehlers JP, Worley LA, Makita J, Yokota Y, Harbour JW. Functional gene expression analysis uncovers phenotypic switch in aggressive uveal melanomas. Cancer Res. 2006;66:4602–4609. doi: 10.1158/0008-5472.CAN-05-4196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slingluff CL, Jr, Chianese-Bullock KA, Bullock TN, Grosh WW, Mullins DW, Nichols L, Olson W, Petroni G, Smolkin M, Engelhard VH. Immunity to melanoma antigens: from self-tolerance to immunotherapy. Adv Immunol. 2006;90:243–295. doi: 10.1016/S0065-2776(06)90007-8. [DOI] [PubMed] [Google Scholar]