Abstract
Background:
The surgical extraction of impacted third molars is a common oral surgical procedure, and it is often associated with complications such as sensory nerve damage, dry socket, pain, swelling, trismus, infection and hemorrhage.
Aim:
The aim of this study was to determine the surgical indications and risk factors for complications of third molar surgery at a Nigerian teaching hospital.
Materials and Methods:
Medical records of patients referred to the Oral Surgery Clinic of our institution for surgical extraction of their impacted mandibular third molars from January 2008 to December 2010 were retrospectively examined. Information on patients’ demography, types of impaction, operative parameters and complications were obtained and analyzed using Statistical Package for Social Sciences (SPSS Version 13), Chicago, IL, USA. A P < 0.0.5 was considered significant.
Results:
A total of 330 impacted teeth were extracted from 250 patients. Male comprises (104/250 [41.6%]) and female (146/250 [58.4%]). The mesioangular (176/330 [53.4%]) and distoangular (73/330 [22.1%]) impactions were the commonest types. Recurrent pericoronitis (154/330 [46.7%]) was the most common indication for extraction. The complications were delayed healing (19/330 [5.8%]), alveolar, osteitis (9/330 [2.7%]) and injury to alveolar nerve (2/330 [0.6%]). Cigarette smoking (P < 0.001), Oral contraceptives use (P = 0.01), age of the patient (P = 0.03) and the surgeon's experience (P = 0.04) were found to be significantly associated with the development of alveolar osteitis; nerves injuries were significantly associated with the raising of a lingual flap (P < 0.001) and the technique of surgery (P ≤ 0.001).
Conclusion:
The age of the patient, cigarette smoking and oral contraceptive use at the time of surgery are some of the factors affecting outcome in third molar surgery.
Keywords: Indications and complications, Surgery, Third molar
Introduction
The surgical extraction of impacted third molars is a common oral surgical procedure.[1] Common complications following third molar surgery include sensory nerve damage, dry socket, pain, swelling, trismus, infection and hemorrhage.[1,2] Other complications include oro-antral fistula, buccal fat herniations, and iatrogenic damage to the adjacent second molar and iatrogenic mandibular fracture. Pain, trismus and swelling are almost universal after this procedure, and the incidence of both inferior alveolar and lingual nerve damage is high and may be permanent.[3] Jerjes et al.[3] found incidence of 0.7% and 1.0% for inferior alveolar and lingual nerves respectively after 2 years post operation. In another study, conducted by Blondeau and Daniel, 3 (0.5%) cases of permanent nerve damage were observed out of the 6 (1.1%) cases of nerve injuries seen in 327 patients who had surgical extraction of their impacted third molar teeth.[4] The authors observed that patients over 24 years of age had a higher incidence of nerve injury.[4]
Generally, age has been reported to affect the postoperative morbidity following third molar surgery. It is believed that with increasing age, bone become harder and brittle; ostectomy is more difficult and prolonged resulting in more pain, trismus and swelling.[3,5] Other factors that may affect post-operative complications in impacted third molar surgery are gender, type and depth of impaction, level of difficulty, experience of the surgeon, patient medical condition, as well as smoking and use of oral contraceptive pills.[6,7,8] The latter, especially in relation to the development of alveolar osteitis has generated lots of controversy. While some authors believed that the use of oral contraceptive pills increases the risk of post extraction alveolar osteitis,[3,6,9] other authors have a contrary opinion.[4,10]
The aim of this study was to determine the surgical indications and complications of third molar surgery at a Nigerian teaching hospital, where no previous study on this subject has been carried out. The study also aimed at establishing the risk factors associated with complications after the impacted third molar surgery.
Materials and Methods
The medical records of patients referred to the Oral Surgery Clinic of our institution for surgical extraction of their impacted mandibular third molars from January 2008 to December 2010 were retrospectively collected. The study protocol was exempted by our institutional ethics review committee. Information on patients’ demography, side of impaction, types of impaction, level of experience of operating surgeons and complications such as nerve injury, alveolar osteitis and delayed healing were obtained. Nerve injury was assessed by an abnormal lingual or the labial sensation.[11] The diagnosis for alveolar osteitis or dry socket was made on the basis of persistent throbbing pain and exposure of bare alveolar bone, presenting 48-72 h post-surgery, as described by Cheung et al.[12] The criteria described by Phillips et al.[13] for delayed healing after third molar surgery was modified and adopted for evaluation of delayed healing in the present study. A post-surgery visit in which at least one of the following treatments occurred: an antibiotic or analgesic was prescribed; the surgical site was reopened or debrided; or another unspecified treatment was rendered, was categorized as delayed healing. The collected data were analyzed using Statistical Package for Social Sciences Version 13 (Chicago, IL, USA). Comparative statistics were done using Chi-square and Fisher's exact tests as appropriate. A P < 0.05 was considered significant.
Results
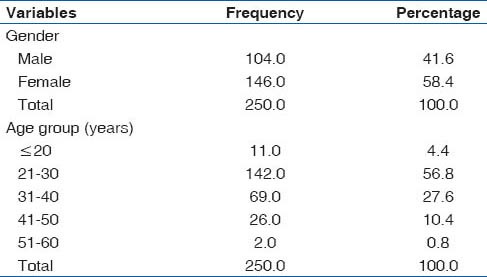
A total of 330 impacted lower third molars were extracted from 250 patients within the study period. Male comprises, 104/250 (41.6%) and female, 146/250 (58.4%) with ages ranging from 18 to 54 years [Mean 29.7 (7.60)] Over half of the patients were in the 21-30 years age category (142/250 [56.8%]); this was followed by the 31-40 years age bracket (69/250 [27.6%]), [Table 1]. Dental Officers (107/330 [32.4%]) and Senior Registrars (104/330 [31.5%]) performed more of the third molar surgeries, followed by Registrars (84/330 [25.5%]). The least number of surgeries were carried out by Consultants (35/330 [10.6%]).
Table 1.
Demographic characteristics of patients
More impacted teeth were found on the left side (189/330 [57.3%]) than the right side (141/330 [42.7%]). The mesioangular and distoangular impactions were the commonest type of impactions accounting for 176/330 (53.4%) and 73/330 (22.1%) respectively. Vertical and horizontal impactions were almost equal proportions [Table 2]. Recurrent pericoronitis (154/330 [46.7%]) was the most common indication for surgical extraction. Others indications are listed in Table 2. Prophylactic extractions accounted for about 14/330 (4.2%) of the cases.
Table 2.
Impaction types and indications for surgery
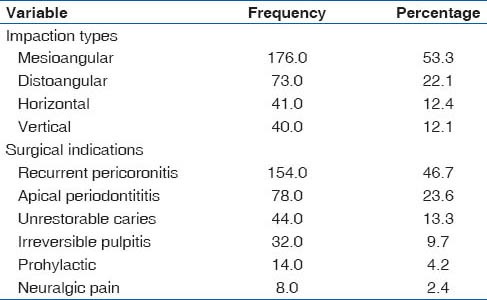
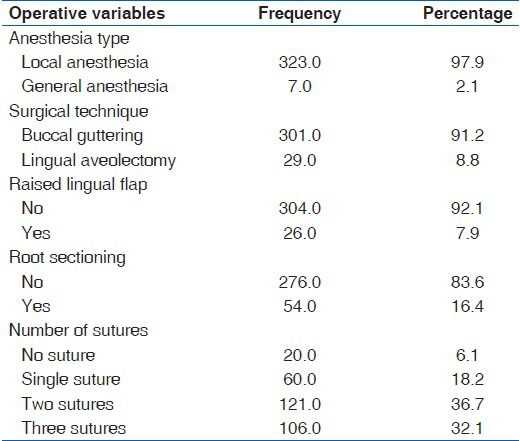
Table 3 shows operative characteristics of the extracted teeth. Almost all the cases (327/330 [97.9%]) were done under local anesthesia, and the buccal “guttering” technique was the favored operative method and was used in 301/330 (91.2%) of the extractions. Lingual flap was raised in 26/330 (7.9%) of cases while root sectioning was performed in only 54/330 (16.4%) of the surgical extractions. Multiple suturing was the preferred method of closure, with placement of two sutures slightly favored >3. Suture-less technique was observed in only 20/330 (6.1%) of cases [Table 3].
Table 3.
Operative characteristics of 330 impacted mandibular third molars
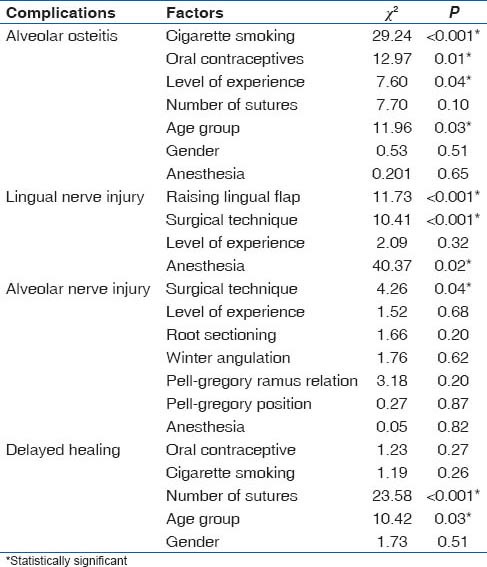
The most common complication was delayed healing (19 [5.8%]), followed by alveolar, osteitis (9 [2.7%]), injury to alveolar nerve (2 [0.6%]), and injury to the lingual nerve (1 [0.3%]) in that order. While the development of delayed healing was significantly associated with the number of sutures (χ2 = 23.58, P < 0.001), cigarette smoking (χ2 = 9.24, P < 0.001), oral contraceptives use (χ2 = 12.97, P = 0.01), age of the patient (χ2 = 11.96, P = 0.03) and the surgeon's experience (χ2 = 7.60, P = 0.04) were found to be significantly associated with the development of alveolar osteitis [Table 4]. Older patients are likely to develop more alveolar osteitis than younger ones. Similarly, injuries to the lingual and inferior alveolar nerves were significantly associated with the raising of a lingual flap and the technique of surgery respectively. While gender, number of sutures and type of anesthesia were not significant in the development of alveolar osteitis, injury to the lingual nerve was significantly associated with the anesthesia type (χ2 = 40.37; P = 0.02) [Table 4]. The risk of injury to the lingual nerve was seen to be higher in patients who had surgical extraction under general anesthesia (GA). However, anesthesia type had no significant effect on the incidence of inferior alveolar nerve injury (P = 0.82) [Table 4].
Table 4.
Factors influencing complications of surgical extractions
Discussion
Majority of impacted mandibular third molars are diagnosed and extracted during the second and third decades of life.[2,11] This was well-demonstrated by the result of the present study with over 60% of the extractions carried out in patients aged 30 years and below. The reason may be because majority of studies on third molar surgery including the present one were carried out either in a university community or in an urban setting where a good number of the population fall within this age group.
There were slightly more females than males and the ratio of 1:1.3 obtained in the present study is consistent with published reports on gender incidence of impacted mandibular third molars.[6,8,11] The reasons usually stated for the slight female predominance is that females tend to present earlier at the clinic probably due to their lower level of tolerance and lower pain threshold compared to their male counterpart.[14]
The mesioangular impaction was the most common impaction observed in this study, lending credence to the results of other authors.[11,15,16] Few authors however found vertical impaction most common.[6,17] Although our data did not include information on mucosa coverage, we found recurrent pericoronitis to be the most common indication for third molar surgery. One report has shown that mesioangular and vertical impactions, especially those with partial mucosa coverage, tends to present with recurrent episodes of pericoronitis.[17] Thus, the high prevalence of recurrent periconitis observed in the present study may be connected with the recorded high proportion of mesioangular impactions. Our result is in agreement with published reports on indications for surgical extraction of impacted third molars.[7,11,18] However, Mwaniki and Guthua[19] found pain due to caries as the main indication for surgical intervention in the 827 patients treated.
Prophylactic extraction was expectedly low in this study, and this differs sharply from most studies in the western world where extraction for prophylactic reasons still account for a considerable proportions of third molar surgeries.[20] One possible reason for the differences is that over 68% of surgical extractions of the impacted third molar are done under GA by surgeons in the western world[18,21] compared to the 2.1% for GA in the present study. To avoid repeated exposure to GA, prophylactic extractions of all the impacted third molars, where one of multiple impacted teeth is indicated for surgery under GA is a common practice. The factors guiding the choice of anesthesia are the patient's preference, the number of teeth to be extracted, the depth of impaction and the patient's level of anxiety.[11] In a resource-limited economy like ours cost and lack of facilities for day case surgery may be other factors to be considered in the choice of anesthesia for third molar surgery.
Delayed clinical healing after third molar surgery is not uncommon and Ruvo et al.[22] have shown that this significantly increased the prevalence of delayed recovery for lifestyle, oral function, late symptoms and pain. In the present study, the most common complication was delayed healing, and this was found to be significantly associated with the number of sutures and age. Delayed healing was observed in patients who had single or multiple sutures techniques. This was consistent with published reports on suture techniques and complications in third molar surgery.[23,24,25]
The overall rate of dry socket has been reported to vary from 0% to 35% among studies.[1,11,26] Thus, the prevalence of 2.7% obtained in the present study is in line with earlier reports on the frequency of dry socket. The development of alveolar osteitis was found to be significantly associated with the use of oral contraceptives, cigarette smoking, patient's age and level of experience of the operating surgeon. These observed factors are consistent with previous reports.[6,23,27] With increasing age, bone becomes harder and brittle; ostectomy is more difficult and prolonged resulting in more pain and this may result in the higher incidence of alveolar osteitis than in younger individuals.[6,11] Benediktsdóttir et al.[6] in their analysis of 335 patients with age ranging from 18.1 to 44.8 years, who had surgical extraction, found that patients over 26.5 years had 2-2.5 times higher risk for operation time (above 10 min) compared to younger patients (OR = 2.50; P = 0.01). The surgeon's experience has been reported to affect the rate of postoperative complications. Sisk et al.[27] compared the outcome of impacted third molar surgery performed by an oral surgery faculty group to the resident group in the same institution. They found that complications were numerous after removal of teeth classified as partially or completely impacted within bone and that less experienced surgeons had significantly higher incidences of complications.
The rate of sensory nerve damage after third molar surgery has been shown to range from 0.5% to 20%.[1,11,19] In this study, the prevalence of nerve injuries was low with injury to alveolar and lingual nerves accounting for 0.6% and 0.3% respectively. The findings may not be unconnected to the observed surgical techniques which were predominantly the buccal ‘guttering’ technique and without the raising of a lingual flap in majority of the cases. The results of our study agreed with published reports on nerve injury in third molar surgery.[28,29] Avoidance of lingual nerve retraction will minimize the incidence of injury to the lingual nerve during impacted third molar surgery.[29,30]
Other factors that have been linked to increased risks of nerve injury in third molar surgery include radiological signs of proximity to the inferior alveolar canals, fully impacted teeth, age of the patient and visibility of inferior alveolar nerve during surgery.[4,6] Reports by Benediktsdóttir et al.[6] and Blondeau and Daniel[4] have shown that with increasing age, the incidence of nerve injuries rises. Apart from age, other information such as socioeconomic factors and medical history of patients, which may affect the outcome of third molar surgery, were not available from the medical records of our subjects and this may be one of the limitations of this study
In conclusion, delayed healing, alveolar osteitis and nerve injuries are complications associated with third molar surgery. Patients’ medical condition, the age of the patient, cigarette smoking, as well as use of oral contraceptives at the time of surgery, are some of the factors affecting outcome of third molar surgery. Patients should be counseled on the potential complications of third molar surgery based on the presence of any identifiable risk factors. For the preventable ones, careful attention to surgical details will go a long way in minimizing the incidence of such complications in impacted third molar surgery.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Mercier P, Precious D. Risks and benefits of removal of impacted third molars. A critical review of the literature. Int J Oral Maxillofac Surg. 1992;21:17–27. doi: 10.1016/s0901-5027(05)80447-3. [DOI] [PubMed] [Google Scholar]
- 2.Ogini FO, Ugboko VI, Assam E, Ogunbodede EO. Postoperative complaints following impacted mandibular third molar surgery in Ile-Ife, Nigeria. South Afr Dent J. 2002;57:264–8. [PubMed] [Google Scholar]
- 3.Jerjes W, Swinson B, Moles DR, El-Maaytah M, Banu B, Upile T, et al. Permanent sensory nerve impairment following third molar surgery: A prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e1–7. doi: 10.1016/j.tripleo.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: Postoperative complications and their risk factors. J Can Dent Assoc. 2007;73:325. [PubMed] [Google Scholar]
- 5.Shepherd JP, Brickley M. Surgical removal of third molars. Prophylactic surgery should be abandoned. Br Med J. 1994;309:620–1. doi: 10.1136/bmj.309.6955.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benediktsdóttir IS, Wenzel A, Petersen JK, Hintze H. Mandibular third molar removal: Risk indicators for extended operation time, postoperative pain, and complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:438–46. doi: 10.1016/j.tripleo.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 7.Yuasa H, Sugiura M. Clinical postoperative findings after removal of impacted mandibular third molars: Prediction of postoperative facial swelling and pain based on preoperative variables. Br J Oral Maxillofac Surg. 2004;42:209–14. doi: 10.1016/j.bjoms.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Jerjes W, El-Maaytah M, Swinson B, Banu B, Upile T, D’sa S, et al. Experience versus complication rate in third molar surgery. Head Face Med. 2006;2:14. doi: 10.1186/1746-160X-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garcia AG, Grana PM, Sampedro FG, Diago MP, Rey JM. Does oral contraceptive use affect the incidence of complications after extraction of a mandibular third molar? Br Dent J. 2003;194:453–5. doi: 10.1038/sj.bdj.4810032. [DOI] [PubMed] [Google Scholar]
- 10.Larsen PE. Alveolar osteitis after surgical removal of impacted mandibular third molars. Identification of the patient at risk. Oral Surg Oral Med Oral Pathol. 1992;73:393–7. doi: 10.1016/0030-4220(92)90312-e. [DOI] [PubMed] [Google Scholar]
- 11.Obiechina AE, Oji C, Fasola AO. Impacted mandibular third molars: Depth of impaction and surgical methods of extraction among Nigerians. Odontostomatol Trop. 2001;24:33–6. [PubMed] [Google Scholar]
- 12.Cheung LK, Chow LK, Tsang MH, Tung LK. An evaluation of complications following dental extractions using either sterile or clean gloves. Int J Oral Maxillofac Surg. 2001;30:550–4. doi: 10.1054/ijom.2000.0128. [DOI] [PubMed] [Google Scholar]
- 13.Phillips C, White RP, Jr, Shugars DA, Zhou X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg. 2003;61:1436–48. doi: 10.1016/j.joms.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Colorado-Bonnin M, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Quality of life following lower third molar removal. Int J Oral Maxillofac Surg. 2006;35:343–7. doi: 10.1016/j.ijom.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Bamgbose BO, Akinwande JA, Adeyemo WL, Ladeinde AL, Arotiba GT, Ogunlewe MO. Effects of co-administered dexamethasone and diclofenac potassium on pain, swelling and trismus following third molar surgery. Head Face Med. 2005;1:11. doi: 10.1186/1746-160X-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sekhar CH, Narayanan V, Baig MF. Role of antimicrobials in third molar surgery: Prospective, double blind, randomized, placebo-controlled clinical study. Br J Oral Maxillofac Surg. 2001;39:134–7. doi: 10.1054/bjom.2000.0557. [DOI] [PubMed] [Google Scholar]
- 17.Stanley HR, Alattar M, Collett WK, Stringfellow HR, Jr, Spiegel EH. Pathological sequelae of “neglected” impacted third molars. J Oral Pathol. 1988;17:113–7. doi: 10.1111/j.1600-0714.1988.tb01896.x. [DOI] [PubMed] [Google Scholar]
- 18.Almendros-Marqués N, Berini-Aytés L, Gay-Escoda C. Influence of lower third molar position on the incidence of preoperative complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:725–32. doi: 10.1016/j.tripleo.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 19.Mwaniki D, Guthua SW. Incidence of impacted mandibular third molars among dental patients in Nairobi, Kenya. Trop Dent J. 1996;19:17–9. [Google Scholar]
- 20.Lopes V, Mumenya R, Feinmann C, Harris M. Third molar surgery: An audit of the indications for surgery, post-operative complaints and patient satisfaction. Br J Oral Maxillofac Surg. 1995;33:33–5. doi: 10.1016/0266-4356(95)90083-7. [DOI] [PubMed] [Google Scholar]
- 21.Worrall SF. Antibiotic prescribing in third molar surgery. Br J Oral Maxillofac Surg. 1998;36:74–5. doi: 10.1016/s0266-4356(98)90765-3. [DOI] [PubMed] [Google Scholar]
- 22.Ruvo AT, Shugars DA, White RP, Philips C. The impact of delay clinical healing after third molar surgery on health-related quality of life outcomes. J Oral Maxillofac Surg. 2005;63:929–35. doi: 10.1016/j.joms.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 23.Waite PD, Cherala S. Surgical outcomes for suture-less surgery in 366 impacted third molar patients. J Oral Maxillofac Surg. 2006;64:669–73. doi: 10.1016/j.joms.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 24.Osunde OD, Saheeb BD, Adebola RA. Comparative study of effect of single and multiple suture techniques on inflammatory complications after third molar surgery. J Oral Maxillofac Surg. 2011;69:971–6. doi: 10.1016/j.joms.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 25.Osunde OD, Adebola RA, Saheeb BD. A comparative study of the effect of suture-less and multiple suture techniques on inflammatory complications following third molar surgery. Int J Oral Maxillofac Surg. 2012;41:1275–9. doi: 10.1016/j.ijom.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Chiapasco M, Crescentini M, Romanoni G. Germectomy or delayed removal of mandibular impacted third molars: The relationship between age and incidence of complications. J Oral Maxillofac Surg. 1995;53:418–22. doi: 10.1016/0278-2391(95)90715-7. [DOI] [PubMed] [Google Scholar]
- 27.Sisk AL, Hammer WB, Shelton DW, Joy ED., Jr Complications following removal of impacted third molars: The role of the experience of the surgeon. J Oral Maxillofac Surg. 1986;44:855–9. doi: 10.1016/0278-2391(86)90221-1. [DOI] [PubMed] [Google Scholar]
- 28.Garcia AG, Sampedro FG, Rey JG, Vialla PG, Martins MS. Pell-Gregory classification is unreliable as a predictor of difficulty in extracting impacted lower third molars. Br J Oral Maxillofac Surg. 2003;83:585–7. doi: 10.1054/bjom.2000.0535. [DOI] [PubMed] [Google Scholar]
- 29.Pichler JW, Beirne OR. Lingual flap retraction and prevention of lingual nerve damage associated with third molar surgery: A systematic review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:395–401. doi: 10.1067/moe.2001.114154. [DOI] [PubMed] [Google Scholar]
- 30.Coulthard P. Increased tendency to temporary nerve damage with lingual retractor use. Evid Based Dent. 2002;3:107–8. [Google Scholar]


