Abstract
Demographic characteristics have been found to influence pain management decisions, but limited focus has been placed on participants’ reactions to feedback about their use of sex, race, or age to make these decisions. The present study aimed to examine the effects of providing feedback about demographic cue use to participants making pain decisions. Participants (n=107) viewed 32 virtual human (VH) patients with standardized levels of pain, and provided ratings for VHs’ pain intensity and their treatment decisions. Real-time LENS model idiographic analyses determined participants’ decision policies based on cues used. Participants were subsequently informed about cue use and completed feedback questions. Frequency analyses were conducted on responses to these questions. Between 7.4%–89.4% of participants indicated awareness of their demographic or pain expression cue use. Of those individuals, 26.9%–55.5% believed this awareness would change their future clinical decisions, and 66.6%–75.9% endorsed that their attitudes affect their imagined clinical practice. Between 66.6%–79.1% of participants who used cues reported willingness to complete an online tutorial about pain across demographic groups. This study was novel because it provided participants feedback about their cue use. Most participants who used cues indicated willingness to complete in an online intervention, suggesting this technology’s utility for modifying biases.
Keywords: Virtual Human Technology, Sex, Race, Age, Feedback, Cues
Introduction
Although pain is among the most common reasons why individuals seek medical attention,7 pain assessment and treatment can be difficult. Self-reports of pain remain the gold standard for pain assessment; however, clinicians and laypeople often rely on their own judgments to make pain management decisions.12 As a result, research has showed that healthcare providers have stereotypes or biases based on a patient’s demographic characteristics that influence their pain management decisions.2,3,5,11,15,17 However, there is limited research that experimentally examines the use of demographic characteristics to make pain management decisions, and even fewer studies that inform people of their use of demographic characteristics. In order to minimize disparities in pain management, it is important for individuals to be aware of their explicit and implicit biases/cue use and their influence on clinical decision-making.1,8
Discrepancies in the pain management decisions related to sex, race, and age have been demonstrated through the use of virtual human (VH) technology.8,16,18 The advantage of using VH technology and VH patients to evaluate pain management decisions is that it is a standardized, experimentally-controlled approach that assesses whether an individual uses demographic cues in their pain decision-making. Another advantage of VH technology is that the participants can be provided immediate feedback on their pain management decisions. The previous studies have also found that participants rated the VH faces are depicting realistic facial expressions and have high visual fidelity.9 However, the novelty of this study was that the participants were able to immediately learn whether they are using demographic characteristics to make their pain management decisions.
Targeting participants’ use of cues in pain decision-making could result in better quality of care for patients. It is also important to know how individuals making clinical decisions would respond to such feedback about their cues. There is a dearth of information about whether individuals are aware of their own use of cues in pain decision-making, and how awareness of their cue use would affect their clinical practice. The purpose of this study was to examine to what extent individuals making pain assessment and treatment decisions were aware of their demographic cue use, and how becoming aware to it would influence their likelihood to participate in an intervention to modify their cue use. Overall, this project was used to establish the initial examination of the possibility of using VH technology and environment for their potential to alter cue use in decisions about pain.
Materials and Methods
Participants
Participants consisted of 107 undergraduate students (mean age = 23.9 years, SD = 7.6 years; 59 female) from the University of Florida. Race breakdown across participants showed that the study included individuals from the following backgrounds: Caucasian (62%), Asian (19%), African-American (9%), or “other race” (10%). Ethnically, the sample was predominantly Non-Hispanic (86%). Participants were recruited via study announcements posted throughout the University of Florida’s campus. Inclusion criteria for the study was: 1) age of 18 years or older at the time of the study, and 2) currently enrolled student at the University of Florida. Compensation for participating in the 1.5-hour online study was through a $15 gift card.
Procedure
This study was approved by the University of Florida’s Institutional Review Board in Gainesville, FL. Prior to enrollment, all participants completed an informed consent form for completing study procedures. Interested participants received a password to a secure, password-protected website, and were asked to complete a demographic questionnaire. Each participant then viewed 32 empirically validated VH profiles, each consisting of a 20-second looped video of a VH face, a clinical vignette of a patient with low back pain, and vital signs.14 Each VH face displayed a different combination of demographic characteristics such as sex (male or female), race (Caucasian or African American), age (young or old) and pain expression (high or low). Each combination of the VH faces was displayed twice, although the exact same VH faces were not used, in order to average the results to get a composite pain assessment and treatment score for each combination of VH faces. Figures 1 and 2 show still frame images of VH faces displaying high and low pain. Subsequently, participants answered pain assessment and treatment questionnaires.
Figure 1.
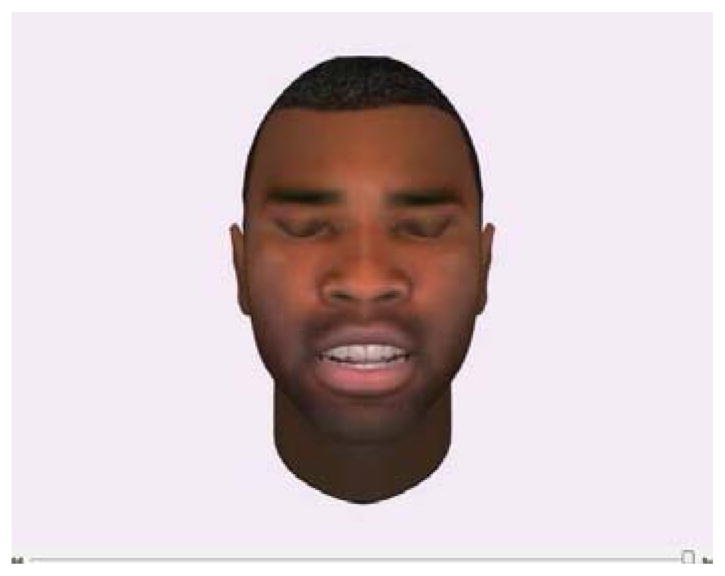
Example of a young, African American virtual human male displaying a “high” pain expression.
Figure 2.

Example of an old, Caucasian virtual human female displaying a “low” pain expression.
A LENS model was employed to determine how individuals use environmental cues to make judgments about how to make pain management decisions.4,6 Empirical applications of this model typically consists of using cue-containing profiles that are presented to a study participant, and ask them to make decisions. The LENS model not only captures the cue-use of the participants’ as a group (nomothetic analyses), but also the individual participant’s use of cues decisions (idiographic analyses).
Based on the participants’ responses to questions regarding VHs’ pain intensity and their likelihood to administer opioid analgesics, idiographic analyses were used conducted, which involved calculating automatic regressions to capture whether sex, race, age or pain expression influenced participants’ pain management decisions. Participants who used demographic cues to make pain assessment and treatment recommendations were informed of their cue use. For example, a participant who used race in making pain assessment and treatment decisions was presented with the following revelation:
“You rate that Caucasians have lower pain intensity than African Americans. You are less likely to administer opioids analgesics to Caucasians than African Americans.”
Following the revelation of cue use, participants were asked questions related to awareness of their response patterns and the influence of this feedback on attitudes towards receiving educational interventions to alter their clinical decision-making. Individuals that did not use demographic cues in their pain management decisions were instructed to answer questions from the perspective of someone who used demographic cues. However, because only 3/107 participants had non-significant cue use, analyses were not conducted on these participants.
Questionnaires
Pain Assessment and Treatment Questionnaires
Participants were asked to imagine that they are healthcare professionals, and they were asked to rate the pain intensity of and willingness to administer opioid analgesics to the VH patients using an electronic 100-point visual analog scale (VAS). Participants indicated their responses to pain intensity by moving the slider with endpoints ranging from “No pain sensation” to the “Most pain sensation imaginable.” Participants were asked to make recommendations regarding their willingness to administer opioid analgesics to the VH patient by moving the VAS slider with endpoints ranging from “Not at all likely” to “Complete certainty.”
Feedback Questionnaires
Participants who used demographic cues (i.e., sex, race, age) to make pain assessment and treatment recommendations were asked to individually answer questions for each type of cue used. Participants were asked to answer “Yes” or “No” for the following questions: (1) Were you aware that you used sex, race, age or pain to make your pain assessment and treatment decisions? (2) Does knowledge of your results change your attitude? (3) Do you think your attitudes affect your clinical practice? (4) Would you be willing to participate in an online tutorial that provides information about pain in patients who belong to different demographic groups (e.g., sex, race, or age)?
In addition, participants answered the following VAS questions: (1) “How likely are you to change your assessment and treatment attitudes after finding out the results from this study?”, with endpoints ranging from “Not at all willing to change” to “Completely willing to change,” (2) “How much do you think your attitudes affect your clinical practice?”, with endpoints ranging from “Does not affect” to “Completely affect,” and (3) “How likely are you to modify your assessment and treatment practices after taking an online tutorial on pain management?”, with endpoints ranging from “Not at all likely” to “Very likely.”
GREP
The Gender Role Expectations of Pain (GREP) questionnaire has 9 VASs ranging from 0 (not at all sensitive, no endurance, or not at all willing) to 100 (most sensitive imaginable, most endurance imaginable, or most willing imaginable). The GREP examines a participant’s view of the typical man and women with respect to pain sensitivity, pain endurance, and willingness to report pain. The GREP also assists in determining a person’s attribution of his or her own pain sensitivity, pain endurance, and willingness to report pain relative to the typical man and woman.
Statistical Analyses
All data analyses were performed using SPSS for Windows (Version 20). Descriptive analyses were conducted to summarize the demographic characteristics of the sample. Idiographic analyses were conducted by calculating linear regressions, which automatically calculated as each participant answered the pain assessment and treatment decisions in order to obtain the beta weights to determine frequency of sex, race, age, or pain expression cue use when making pain management decisions. If participants had a significant beta weight for a particular demographic cue (e.g., sex), they were determined to be using the cue to make their pain management decisions, and they were then asked to complete a feedback questionnaire for that cue.8 Frequency analyses were conducted in order to examine the number of cues that each participant employed when rating pain intensity and likelihood of administering opioids analgesics, as well as to determine how many participants were aware of their use of cues in their decisions. Frequency analyses were also conducted on feedback questions related to participants’ beliefs, such as whether these results change their attitudes, if attitudes affect their clinical practice, and their willingness to participate in an online tutorial for each of the cues. Z-tests of proportions were then calculated to determine whether significant differences were present in the proportions of “yes” responses to feedback questions based on age, race, or sex cue use. Z-tests of proportions were also used to examine differences in participant demographics based on type of cue used. Finally, independent-samples t-tests were used to measure the difference in the GREP scores based on sex, race, and age cue use.
Results
Participant Characteristics
To determine whether cue use was associated with the participants’ own demographic characteristics, Z-tests of proportions were conducted. Z-tests showed that cue use was not significantly different based on the participant’s race or sex. However, a significantly higher proportion of non-Hispanic participants used race as a cue (z = −2.43, p < .05) compared to Hispanic participants (see Table 1). For each cue type, independent-samples t-tests showed that there were no significant GREP response pattern differences based on whether the participants’ cue use.
Table 1.
Frequencies of participants’ demographic characteristics based on type of VH cue used in pain decision-making. A significantly greater proportion of non-Hispanic, compared to Hispanic participants used race as a cue.
| Sex | Race | Ethnicity | Age | ||||
|---|---|---|---|---|---|---|---|
| Cue Type | Male N=48 | Female N=59 | Caucasian N=66 | Minority N=41 | Hispanic N=15 | Non-Hispanic N=92 | Average = 23.9 years |
| Sex (n = 24) | 11 | 13 | 16 | 8 | 2 | 22 | 22.33 |
| Race (n = 27) | 10 | 17 | 16 | 11 | 0 | 27* | 24.7 |
| Age (n = 50) | 20 | 30 | 32 | 18 | 7 | 43 | 23.92 |
| Pain (n = 104) | 47 | 57 | 65 | 39 | 14 | 90 | 23.96 |
| No cue (n = 3) | 1 | 2 | 1 | 2 | 1 | 2 | 22.67 |
p < .05 based on Z-test of proportions
Demographic or Pain Cues Used By Participants
After viewing 32 VH patient faces, participants were asked to rate the VHs’ pain intensity and their willingness to administer opioids to the VH patients. Based on the pain management questions, a significant number of the participants used demographic and pain expression cues to make their pain management decisions: 23.4% (24/107) used sex, 25.2% (27/107) used race, 46.7% (50/107) used age, and 96.3% (103/107) used pain expression. There were only three people who did not have a statistically reliable decision strategy using the available cues. Not only was there a significant difference between the number of participants who used demographic and pain expression cues to make their pain management decisions, there was also as significant difference between how participants used sex, age, and pain cues. Participants were significantly more likely to use female, old, and high pain expression cues to make their pain management decisions. See Table 2 for frequency and z-scores tests of proportions for demographic and pain expression cue use.
Table 2.
As demonstrated by frequency analyses, cue use tended to be in the direction of VHs that were female, African-American, older adults, and/or had a high pain facial expression. Z-score tests of proportions showed that significantly more individuals used female, old, and high pain, compared to male, young, and low pain cues, respectively.
| Sex N=24 | Race N=27 | Age N=50 | Pain Expression N=104 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Z-score | Caucasian | African American | Z-score | Old | Young | Z-score | Low Pain | High Pain | Z-score |
| 7 | 17 | 2.87*** | 12 | 15 | 0.82 | 46 | 4 | 8.4*** | 14 | 90 | 10.54*** |
Significance level for Z-score tests of proportions:
p<.05,
p<.01,
p<.001
Note: There were 3 participants who did not use any cues during this study (total N=107). Participants’ cue use was determined to be significant at the p<.10.
Of the participants who used demographic cues to make pain management decisions, participants were most likely to use two cues at once (49/107; 45.8%). Participants most commonly used both age and pain expression together to make their pain management decisions (30/107; 28%). Twenty-nine percent (32/107) or participants used one demographic or pain cue (32/107; 29.9%). Pain expression was the most commonly used feature for participants with only one type of cue use (32/107; 29.9%).
Participant Awareness of Cue Use in Pain Management Decision-Making
Overall, pain expression was the most commonly used cue (104/107; 96.3%), with most (89%) of these individuals indicating awareness for factoring this cue into their pain management decisions. Information about sex, race, and age cue usage is described below.
Sex
Of the participants who used sex as a cue, 50% (12/24) were aware that they used sex to make their pain assessment and treatment decisions. More than half of these participants indicated that awareness of their results would change their pain assessment and treatment attitudes (54.2%, 13/24). Seventy-five percent of these participants endorsed that their attitudes would affect their imagined clinical practice. Further, 79.2% (19/24) indicated that they would be willing to participate in an online tutorial about pain in patients of different demographic groups.
Race
Less than 1% of the participants (2/27) indicated that they were aware that they used race as a cue to make pain assessment and treatment decisions. However, 55.6% of the participants (15/27) stated that learning their results changed their attitudes, and 66.7% (18/27) thought that their attitudes affected their imagined clinical practice. Of the participants who used race as a cue, 66.7% (18/27) stated that they were willing to participate in an online tutorial about pain in patients of different demographic groups.
Age
Age was the most common demographic cue used by participants (46.7%; 50/107), and 62% (31/50) were aware that they used age to make pain assessment and treatment decisions. Almost one third of participants (32%; 16/50) noted that learning their results changed their attitudes, and 68% (34/50) endorsed that their attitudes affected their imagined clinical practice. Of the participants who used age as a cue, 78% (39/50) reported that they were willing to participate in an online tutorial about pain in patients of different demographic groups.
Z-Tests of Proportions Based on Demographic Cue Use
Based on the VHs’ sex, race, and age, Z-tests of proportions were conducted to examine differences in proportions of individuals who 1) were aware of their cue use, 2) changed their attitudes after learning their results, and 3) would be willing to participate in an online tutorial about pain. Significantly larger proportions of individuals indicated awareness of using sex (z = −3.402, p < .001) and age (z = −4.62, p < .001) as cues compared to race. However, there was no significant difference between individuals who indicated awareness of using age as a cue compared to sex (z = −.98, p = .33).
A significantly higher proportion of individuals who used race as a cue compared to those who used age indicated a change in attitudes after learning their results (z = 2.011, p < .05). However, there was no significant difference in the proportion of those who indicated a change in attitudes after learning their results between individuals who used sex as a cue compared to those who used race (z = −0.10, p = 0.92) or age (z = 1.82, p = .07). Additionally, there were no significant differences in the proportion of individuals who indicated willingness to participate in an online tutorial about pain comparing individuals who used race as a cue compared to age (z = 1.08, p = .28) or sex (z = .099, p = .32), and comparing those who used age as a cue compared to sex (z = .11, p = .91).
Discussion
The influence of a patient’s sex, race, and age on clinical decision-making for pain has been reported across laypersons, healthcare trainees, and healthcare professionals.1,8,9,18,19 Limited focus, however, has been placed on whether individuals are aware of their use of cues, or how these individuals would respond to feedback about their potential use of cues in making judgments about another person’s pain. The current study used an experimental approach, VH technology, and LENS model analyses, to measure participants’ use of demographic cues in pain assessment and treatment. Feedback was provided about each participant’s cue use, and as a result, we were able to measure participants’ awareness of cue use when making clinical decisions. Further, we examined how this feedback affected their likelihood of changing their imagined clinical practices.
Regarding demographic cue use, we found that participants most frequently used pain expression as a cue for VH pain intensity and willingness to administer opioids. This finding is consistent with previous VH idiographic studies showing that pain expression is the most commonly used cue in pain management decisions.8,18,19 However, also consistent with previous VH idiographic studies, sex, race, and age cue use were also significant, with age being the most commonly used of these demographic characteristics.8 Although it was most common for participants to use two cues, including pain expression, our data suggest that a significant percentage of participants relied on additional patient characteristics in evaluating the VHs’ pain intensity and in making treatment decisions.
One novel aspect of the current study was that we provided feedback to participants about their cue use, and evaluated their awareness of using demographic features and pain expression in making pain management decisions. As expected, we found that participants were most commonly aware of using pain expression as a factor in decision-making. Certain participants also indicated awareness of using cues related to the VHs’ demographic characteristics; specifically, significantly higher percentages of individuals were aware that they used age or sex as cues compared to race. To the best of our knowledge, this is the first study to examine participants’ awareness of age, sex, and race cues in pain management. This information provides valuable insight for the creation of future interventions to target cue use, but also acts as an intervention in itself, as many individuals were not aware of how they used cues when making their decisions.
Another innovative aspect of this study was the assessment of whether individuals changed their attitudes after learning about their results, and whether they would be willing to engage in an online intervention to target cue use. We found that the highest proportion of individuals who indicated a change in attitudes after learning their results were those who used race as a cue. This finding is in line with our results showing that racial cues in pain decision-making were least acceptable. Interestingly, this proportion was only significantly greater from those who used age as a cue, suggesting that individuals with age-related cue use may have had what they perceived as an acceptable rationale for using this cue. Although our findings suggest differences in acceptability based on type of cue use, we found that for all cues, more than half of the individuals indicated willingness to participate in an online intervention targeting attitudes about demographic differences in pain decision-making. This finding demonstrates the acceptability of such interventions to target cue use, even for individuals who were aware of their use of cues.
Examination of available participant characteristics of race/ethnicity and sex, indicated that Hispanic participants were less likely to use race as a cue, compared to white participants. There were no differences between men and women participants. These results have implications for training, consistent with theories of prejudice, and exposure/experience with minority or “outgroup” populations.13
The results from this study have implications for the use of online interventions to target cue use in pain management decision-making. First, our results showed that disparities in pain assessment and treatment of VHs were present in our sample. Although age was the most commonly used cue, race was likely the least acceptable, given that the smallest proportion of people indicated awareness of this cue use. Online interventions to target cue use could focus on debunking reasons for individuals’ beliefs for age-related differences, as well as increasing knowledge about race-related differences in the experience of pain. Second, our results demonstrated that online interventions to target pain decision cues were acceptable to a majority of our participants. However, future research is needed to examine how to modify the likelihood of individuals to engage in an online intervention if they do not initially indicate that they would do so. Thus, a better understanding of why some individuals might not be willing to participate in an intervention would be beneficial for ultimately alleviating disparities in pain management. Third, we found that participants’ self-reported attitudes changed as a result of feedback provided from VH technology, suggesting that being made aware of their use of cues could act as a small intervention in itself. Nonetheless, without additional information or behavioral follow-up, it is unclear if this represents real attitude change or a socially desirable response. With the addition of education about pain management across demographic groups, perhaps participants would be even more inclined to change their clinical practice. A future study is needed to determine whether changes in attitudes as a result of an intervention would result in actual clinical practice modifications.
This study was limited in that we used undergraduate students as raters rather than healthcare providers. However, using undergraduate students was an important first step to establishing the feasibility of using VH technology to automatically collect and provide feedback to participants about their use of cues. Our previous work8,16,18 has shown that these cues operate in both licensed healthcare professionals and student populations, suggesting these attitudes are consistent, and somewhat independent of group membership (healthcare professional vs. layperson). Additionally, decisions about pain are made regularly by laypersons for family members and friends. And finally, undergraduate students enrolled in this study could potentially make pain management decisions in the future as healthcare providers. This intervention was valuable for providing them with insight to how certain cues influence their decision-making. A future study would be beneficial to examine the attitudes of currently practicing healthcare professionals and provide feedback about their cue use.
Overall, our results suggest that in addition to pain expression, a significant number of individuals use demographic cues in making pain management decisions. The individuals who used race as a cue were the least aware of their use of cues, but the most likely to change these attitudes after finding out about their cue use. Alternatively, individuals who used age as a demographic cue were the most aware of their use of cues, but least likely to change their attitudes. This study demonstrated that providing feedback about cue use could influence individuals to change their clinical attitudes. Importantly, our results suggest that feedback about cue use could be a critical first step in encouraging individuals to engage in interventions to target implicit biases. Participant ethnicity differences in race cue use also implicate perspective-taking interventions as a plausible method of altering cue use over and above knowledge of cue use.
Perspective.
This is the first study to make individuals aware of whether a VH’s sex, race, or age influences their decision-making. Findings suggest a majority of the individuals who were made aware of their demographic cue us would be willing to participate in an online intervention.
Acknowledgments
Supported by: A grant from the National Institute of Dental & Craniofacial Research (R01DE013208) to Dr. Michael E. Robinson
Footnotes
Disclosure
This research was funded by the National Institute of Dental and Craniofacial Research through a grant (R01DE013208) to Michael E. Robinson. There is no conflict of interest among authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could a3ect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Alqudah AF, Hirsh AT, Stutts LA, Scipio CD, Robinson ME. Sex and race differences in rating others’ pain, pain-related negative mood, pain coping, and recommending medical help. J Cyber Ther Rehabil. 2010;3(1):63–70. [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson KO, Mendoza TR, Valero V, Richman SP, Russell C, Hurley J, Gning I, Lynch GR, Kalish D, Cleeland CS. Minority cancer patients and their providers: pain management attitudes and practice. Cancer. 2000;88:1929–1938. [PubMed] [Google Scholar]
- 3.Aubrun F, Salvi N, Coriat P, Riou B. Sex-and age-related differences in morphine requirements for postoperative pain relief. Anesthesiology. 2005;103(1):156–160. doi: 10.1097/00000542-200507000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Beal D, Gillis JS, Stewart T. The LENS model: computational procedures and applications. Percept Motor Skill. 1978;46:3–28. [Google Scholar]
- 5.Calderone KL. The influence of gender on the frequency of pain and sedative medication administered to postoperative patients. Sex Roles. 1990;23(11–12):713–725. [Google Scholar]
- 6.Cooksey RW. Judgment analysis: Theory, methods, and applications. San Diego, CA: Academic Press; 1996. [Google Scholar]
- 7.Hing E, Cherry DK, Woodwell DA. National ambulatory medical care survey: 2004 summary. Adv Data. 2006;374:1–33. [PubMed] [Google Scholar]
- 8.Hirsh AT, Alqudah AF, Stutts LA, Robinson ME. Virtual human technology: capturing sex, race, and age influences in individual pain decision policies. Pain. 2008;140(1):231–238. doi: 10.1016/j.pain.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hirsh AT, George SZ, Robinson ME. Pain assessment and treatment disparities: a virtual human technology investigation. Pain. 2009;143:106–113. doi: 10.1016/j.pain.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hirsh AT, Callander SB, Robinson ME. Patient demographic characteristics and facial expressions influence nurses’ assessment of mood in the context of pain: a virtual human and lens model investigation. Int J Nurs Stud. 2011;48(11):1330–1338. doi: 10.1016/j.ijnurstu.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horgas AL, Elliott AF. Pain assessment and management in persons with dementia. Nurs Clin North Am. 2004;39:593–606. doi: 10.1016/j.cnur.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 12.Martel MO, Thibault P, Sullivan MJ. Judgments about pain intensity and pain genuineness: the role of pain behavior and judgmental heuristics. J Pain. 2011;12(4):468–475. doi: 10.1016/j.jpain.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 13.Pettigrew TF, Tropp LR. How does intergroup contact reduce prejudice? meta-analytic tests of three mediators. Eur J Soc Psychol. 2008;38(6):922–934. [Google Scholar]
- 14.Prkachin KM. The consistency of facial expressions of pain: a comparison across modalities. Pain. 1992;51:297–306. doi: 10.1016/0304-3959(92)90213-U. [DOI] [PubMed] [Google Scholar]
- 15.Robinson ME, Wise EA. Prior pain experience: influence on the observation of experimental pain in men and women. J Pain. 2004;5(5):264–269. doi: 10.1016/j.jpain.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Stutts LA, Hirsh AT, George SZ, Robinson ME. Investigating patient characteristics on pain assessment using virtual human technology. Eur J Pain. 2010;14:1040–1045. doi: 10.1016/j.ejpain.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vallerand AH, Polomano RC. The relationship of gender to pain. Pain Manag Nurs. 2000;1(3):8–15. doi: 10.1053/jpmn.2000.9759. [DOI] [PubMed] [Google Scholar]
- 18.Wandner LD, Stutts LA, Alqudah AF, Craggs JG, Scipio CD, Hirsh AT, Robinson ME. Virtual human technology: patient demographics and healthcare training factors in pain observation and treatment recommendations. J Pain Res. 2010;3:241–247. doi: 10.2147/JPR.S14708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wandner LD, Hirsh AT, Torres CA, Lok BC, Scipio CD, Heft MW, Robinson ME. Using virtual human technology to capture dentists’ decision policies about pain. J Dent Res. 2013;92(4):301–305. doi: 10.1177/0022034513480802. [DOI] [PMC free article] [PubMed] [Google Scholar]


