Abstract
Objective
To examine differences in access to health care and receipt of clinical preventive services by type of disability among working-age adults with disabilities.
Data Source
Secondary analysis of Medical Expenditure Panel Survey (MEPS) data from 2002 to 2008.
Study Design
We conducted cross-sectional logistic regression analyses comparing people with different types of disabilities on health insurance status and type; presence of a usual source of health care; delayed or forgone care; and receipt of dental checkups and cancer screening.
Data Collection
We pooled annualized MEPS data files across years. Our analytic sample consisted of adults (18–64 years) with physical, sensory, or cognitive disabilities and nonmissing data for all variables of interest.
Principal Findings
Individuals with hearing impairment had better health care access and receipt than people with other disability types. People with multiple types of limitations were especially likely to have health care access problems and unmet health care needs.
Conclusions
There are differences in health care access and receipt of preventive care depending on what type of disability people have. More in-depth research is needed to identify specific causes of these disparities and assess interventions to address health care barriers for particular disability groups.
Keywords: People with disabilities, health care disparities, insurance coverage, adult, population surveillance
Timely receipt of appropriate health care plays a key role in facilitating wellness, preventing injury and illness, promoting optimal recovery when injuries and illness do occur, and managing chronic health conditions (Agency for Healthcare Research and Quality [AHRQ] 2012). However, not all groups in the United States have equal access to quality health care (AHRQ 2012). A number of studies have found health care disparities between people with and without disabilities. Compared to those without disabilities, people with disabilities report more unmet health care needs (National Organization on Disability and Harris Interactive Inc 2004; Gulley and Altman 2008; Iezzoni, Frakt, and Pizer 2011) and are less satisfied with the care they do receive (Jha et al. 2002; Iezzoni et al. 2003; Parish and Huh 2006; Gulley and Altman 2008). There are disability-related disparities in receipt of preventive services such as cancer screening, eye exams, and dental checkups (Chan et al. 1999, 2008; Havercamp, Scandlin, and Roth 2004; Ramirez et al. 2005; Chevarley et al. 2006; Parish and Huh 2006; Yankaskas et al. 2010; Andresen et al. 2013). People with disabilities are also more likely to delay health care due to cost (Chevarley et al. 2006; Lee, Hasnain-Wynia, and Lau 2012). These disparities in health care can contribute to disparities in health status, mortality, and health-related quality of life (McGinnis, Williams-Russo, and Knickman 2002; Drum et al. 2005; U.S. Department of Health and Human Services 2005).
Much of the research on disability-related disparities has analyzed data for people with disabilities compared to those without, as the examples above illustrate. Some of these studies have disaggregated their disability samples in various ways (e.g., by disability type or severity), and the resulting comparisons of each subgroup to the nondisabled reference group imply certain differences between subgroups of people with disabilities. For example, Havercamp, Scandlin, and Roth (2004) found that women with developmental cognitive disabilities were less likely than women without disabilities to have ever had a mammogram, while women with other types of disabilities did not significantly differ from the nondisabled reference group. Iezzoni, Frakt, and Pizer (2011) compared people with upper body mobility, lower body mobility, cognitive, vision, and hearing disabilities to a reference group with no disabilities. They found that odds ratios for delayed or forgone care were highest for people with cognitive limitations. These findings suggest that people with cognitive disabilities may experience greater disparities than those with other types of disabilities. However, very few studies have directly compared health care access and utilization within the disability population.
The population of people with disabilities is quite heterogeneous (Iezzoni 2011), which raises the question of where the disparities really lie. Do people with certain types of disabilities experience greater disparities than people with other disability types? Ability to access and receive health care may vary depending on the particular type of disability a person has. For example, people with physical disabilities often encounter inaccessible doctors' offices, exam tables, and diagnostic equipment (Scheer et al. 2003; Iezzoni, Kilbridge, and Park 2010; Todd and Stuifbergen 2012). Individuals who are deaf or hard of hearing may have difficulty communicating with health care providers, particularly when appropriate interpreter services are not provided (Iezzoni et al. 2004). People who are blind or have low vision have reported problems with receiving health care information in inaccessible formats (O'Day, Killeen, and Iezzoni 2004). The variations in barriers experienced by people with different types of disabilities may have important implications for receipt of needed health care. Yet there is a scarcity of data directly comparing health care access issues between people with different types of disabilities.
The purpose of this study was to further understand disability disparity by examining health care access and receipt of clinical preventive services among adults with disabilities and comparing differences by type of disability. Disparity can be defined in a variety of ways, ranging from any difference between groups (e.g., U.S. Department of Health and Human Services 2000) to differences remaining after accounting for as many other factors as possible (e.g., Vaccarino et al. 2005; Kirby, Taliaferro, and Zuvekas 2006; Lee, Hasnai-Wynia, and Lau 2012). One widely used conceptual model was presented in the Institute of Medicine (IOM) report, Unequal Treatment, which defined racial health care disparities as differences in treatment not justified by underlying health conditions or patient preferences (Smedley, Stith, and Nelson 2003). Thus, adjustments for health and patient preferences should be made to the extent possible in analyses of health care disparities. However, the IOM definition does not suggest controlling for socioeconomic status (SES), because doing so would treat important socioeconomic differences between groups as nonexistent and therefore underestimate true disparities in access to care (Smedley, Stith, and Nelson 2003; Gulley, Rasch, and Chan 2010).
When studying disparities impacting people with disabilities, established approaches applied to other health disparity populations are useful so that findings can be interpreted within the context of existing frameworks. Therefore, we applied the IOM model in our examination of disparities related to disability type. People with disabilities who have more health problems (i.e., high levels of need for health care) may interact with the health care system on a more regular basis than individuals with disabilities who have less complex health care needs. The IOM model takes these differences into account. On the other hand, because the IOM model does not adjust for SES, we expected to see higher levels of health care access and utilization in disability type groups with higher average income. Specifically, based on our preliminary descriptive analyses and prior research on SES differences between disability groups (Erickson, Lee, and von Schrader 2012), we anticipated that (1) people with hearing impairments would have the fewest access problems and unmet needs; and (2) people with cognitive disabilities or more than one type of disability would have the worst access and most unmet health care needs. Furthermore, because the barriers experienced by people with vision impairment are related in large part to communication of information (O'Day, Killeen, and Iezzoni 2004), we hypothesized that this group would be fairly similar to people with hearing impairment. People with physical disabilities are likely to encounter problems with physically inaccessible health care buildings and offices, inaccessible exam equipment, and inadequate training or equipment for safely transferring patients to exam tables (Iezzoni, Kilbridge, and Park 2010). Therefore, we expected that people with physical disabilities would have relatively high levels of unmet health care needs.
Methods
Decisions regarding definitions, research design, and analysis methods were guided by the Expert Panel on Disability and Health Disparities, a national advisory group convened for this project. The six-member panel included highly experienced disability and health researchers with extensive background in epidemiology, medicine, health services research, and the lived experience of disability.
Data Source
We pooled 2002–2008 full-year consolidated files from the Medical Expenditure Panel Survey (MEPS) Household Component to create our analytic dataset. Recommendations for preventive services were consistent for these years, as described below. The MEPS is conducted by the AHRQ and collects comprehensive information on demographic characteristics, health care utilization, quality of care, health care expenditures, sources of payment, and health insurance coverage. The MEPS employs multistage stratified sampling to provide a nationally representative sample of the U.S. community-dwelling population. The MEPS over-samples subgroups of persons who are Hispanic, African American, Asian, and of low-income status to increase the precision of estimates for these groups. The household component has an overlapping panel design, in which a new panel of sample households is selected each year from the National Health Interview Survey sample for the previous year (Ezzati-Rice, Rohde, and Greenblatt 2008; Cohen, Cohen, and Banthin 2009). For each panel, data are collected through five in-person interviews, providing data over a 2-year period. AHRQ creates full-year consolidated files that include data from two consecutive panels, weighted to provide annualized U.S. population estimates. For this study, we conducted cross-sectional analyses of pooled annual data files.
Sample
Our analytic sample within the pooled dataset consisted of working-age adults with disabilities. Because health care access issues differ for adults age 65 and older, almost all of whom have Medicare, we focused specifically on adults aged 18–64 years. We defined presence of disability based on an affirmative response to one or more items reflecting difficulty with basic actions (Altman and Bernstein 2008). These included any limitation in physical functions such as walking, lifting, standing, bending, reaching, or grasping; cognitive limitations such as confusion or memory loss or difficulty making decisions; and any degree of difficulty with vision or hearing (see Appendix SA2). Of the overall sample, 133,368 were working-age adults and 26,090 were working-age adults with disabilities (weighted disability prevalence among working-age adults = 17.9 percent). We excluded 320 people who were insured all year but part of the time was with private insurance and part was with public insurance. In exploratory analyses, this group did not follow patterns similar to any of the other insurance status/types groups but was too small to analyze separately. Therefore, the Expert Panel decision was to exclude these individuals. Similarly, we excluded a small group (n = 428) of individuals who were underweight (body mass index [BMI] < 18.5). From the remaining sample, we included in our analyses 24,141 individuals with no missing data on our variables of interest (see Figure1). When weighted to reflect the larger population, our sample represented a total of 32,869,479 adults with disabilities, including 4,934,859 with hearing limitations, 5,088,305 with vision limitations, 11,424,262 with physical limitations, 2,221,171 with cognitive limitations, and 9,200,882 with multiple types of limitations. Within our analytic sample, we identified three subsamples for analyses regarding cancer screening. There were 13,375 women age 18 years or older (analyzed for receipt of Pap test), 9,951 women 40 years of age or older (analyzed for receipt of mammogram), and 11,506 men and women 50 years of age or older (analyzed for receipt of colorectal cancer screening).
Figure 1.
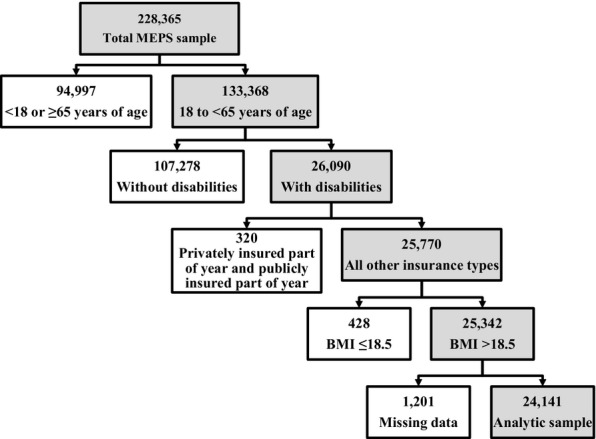
Analytic Sample Selection Process — Medical Expenditure Panel Survey Household Component, 2002–2008
Measures
Dependent Variables
We used three variables to assess access to health care. The first variable combined presence and type of health insurance. The categories were (1) privately insured all year; (2) publicly insured all year; (3) uninsured part of the year and either privately or publicly insured the remainder; and (4) uninsured all year. “Privately insured all year” served as the reference category against which all other categories were compared in multinomial logistic regression. The second variable was whether or not the individual reported having a usual source of medical care (yes/no). A follow-up question asked those who answered yes what their source of care was. If the emergency department was the usual source of care, we recoded respondents as having no usual source of medical care. Third, we created a composite variable to indicate whether individuals had not received or were delayed in receiving medical or dental care or prescription medications in the last 12 months (yes/no). Exploratory analyses examined delayed and forgone care separately for each of the three types of health care service; because patterns were similar across these variables, we combined them into the composite variable.
We analyzed four variables focused on receipt of preventive care. These variables included the following: dental checkup (≥1 per year vs. less often or never), Pap smear for women (within past 3 years or not), mammogram for women age 40 years and older (within past 2 years or not), and colorectal cancer screening for men and women age 50 years and older (ever received blood stool test, sigmoidoscopy, or colonoscopy). We coded cancer screening variables according to U.S. Preventive Services Task Force recommendations that were in effect at the time data were collected (i.e., prior to the 2009 change in breast cancer screening recommendations [U.S. Preventative Services Task Force 2009]).
Primary Independent Variable
We created a single variable indicating type of disability with the following categories: (1) hearing impairment only; (2) vision impairment only; (3) limitation in physical function only; (4) cognitive limitation only; and (5) more than one type of limitation. These categories are congruent with broad functional categories used in the International Classification of Functioning, Disability and Health (World Health Organization 2001). See Appendix SA2 for details of how each disability type was defined. As noted above, we hypothesized that the hearing impairment group would have the fewest problems; therefore, we selected this group as our reference category for all analyses.
Covariates
The demographic and health-related covariates that we controlled for were as follows: race/ethnicity (non-Hispanic white, non-Hispanic Black, Hispanic, non-Hispanic American Indian/Alaskan Native, non-Hispanic Asian/Native Hawaiian/Pacific Islander, or non-Hispanic multiple races), gender, age, perceived physical and mental health (excellent, very good, good, fair, or poor), body mass index (BMI: 18.5–<25, 25–<30, 30–<40, or 40 and higher), diabetes (yes or no), arthritis (yes or no), stroke (yes or no), cardiovascular disease (yes or no), and lung disease (yes or no). We also included a covariate nominated by our Expert Panel to provide additional information about disability: complex activity limitation (yes or no). Complex activity limitation is defined as limitations in ability to participate in social role and self-care activities (Altman and Bernstein 2008), and it was based on responses to MEPS items about needing assistance with activities of daily living or instrumental activities of daily living, and limitations in work, housework, social, or recreational activities (see Appendix SA2).
Statistical Analysis
To implement the IOM definition of health care disparities, we controlled for needs variables (health status and medical conditions) as well as demographic variables closely associated with health and health care use: age, race/ethnicity, and gender (Lê Cook, McGuire, and Zaslavsky 2012). Our models also controlled for presence or absence of complex activity limitation. We performed binomial and multinomial logistic regression using Stata version 12.0 to account for the complex survey design of MEPS (StataCorp 2011). Taylor series linearization was employed for variance estimation. We used a significance level of <0.05 and 95 percent confidence intervals (CI) for all analyses.
Results
The majority of individuals in the sample of working-age people with disabilities were non-Hispanic white and over the age of 40 years (see Table1). Over half of the sample had private health insurance (Table2). Nearly half had received less than one dental checkup per year. Among those 50 years or older, a large percentage had never received colorectal cancer screening.
Table 1.
Demographic and Health Characteristics of Medical Expenditure Panel Survey Household Component 2002–2008 Adults Aged 18–64 Years with Disabilities
| Characteristic | N (Weighted%) |
|---|---|
| Race/ethnicity* | |
| White | 14,521 (72.7) |
| Black | 14,183 (12.1) |
| Hispanic | 4,045 (9.6) |
| American Indian/Alaskan Native | 196 (0.8) |
| Asian/Native Hawaiian/Pacific Islander | 650 (2.6) |
| Multiple races | 546 (2.2) |
| Women | 13,660 (52.4) |
| Age (years) | |
| 18–29 | 2,724 (11.9) |
| 30–39 | 3,380 (13.5) |
| 40–49 | 6,380 (26.3) |
| 50–59 | 8,133 (33.5) |
| 60–64 | 3,524 (14.8) |
| Perceived physical health status | |
| Excellent | 2,463 (12.2) |
| Very good | 4,859 (23.0) |
| Good | 7,356 (31.1) |
| Fair | 6,012 (21.9) |
| Poor | 3,451 (11.8) |
| Perceived mental health status | |
| Excellent | 5,666 (26.0) |
| Very good | 5,611 (25.4) |
| Good | 7,738 (30.6) |
| Fair | 3,853 (13.6) |
| Poor | 1,273 (4.4) |
| Adult body mass index | |
| 18.5–<25 | 6,470 (28.3) |
| 25–<30 | 7,567 (32.2) |
| 30–<40 | 7,781 (31.0) |
| ≥40 | 2,323 (8.5) |
| Diabetes | 3,621 (13.0) |
| Arthritis | 9,740 (39.2) |
| Stroke | 1,213 (4.3) |
| Cardiovascular disease | 3,846 (15.5) |
| Lung disease | 4,311 (17.1) |
| Total | 24,141 (100) |
Except for Hispanic, all categories are ethnically non-Hispanic.
Table 2.
Distribution of Disability Type, Insurance Type or Status, and Health Care Access and Receipt Outcomes among Adults Aged 18–64 Years with Disabilities in the Medical Expenditure Panel Survey Household Component 2002–2008
|
Disability Type |
||||||
|---|---|---|---|---|---|---|
|
N (Weighted%) |
||||||
| Outcome | All Disability N (Weighted%) | Hearing | Vision | Physical | Cognitive | >One |
| Insurance | ||||||
| Privately insured all year | 11,076 (54.5) | 2,080 (73.3) | 1,910 (61.2) | 4,203 (58.0) | 508 (36.5) | 2,375 (40.7) |
| Publicly insured all year | 5,937 (18.2) | 207 (5.3) | 291 (5.6) | 1,790 (15.8) | 667 (30.8) | 2,982 (32.2) |
| Uninsured part of the year* | 2,869 (11.5) | 291 (9.1) | 496 (13.5) | 1,002 (11.3) | 257 (15.8) | 823 (11.0) |
| Uninsured all year | 4,259 (15.7) | 438 (12.3) | 893 (19.7) | 1,393 (14.9) | 330 (16.9) | 1,205 (16.1) |
| Access and utilization | ||||||
| No usual source of care | 4,533 (18.4) | 598 (19.1) | 1,032 (26.7) | 1,357 (15.8) | 441 (24.1) | 1,105 (15.3) |
| Delayed or forgone care† | 6,803 (27.7) | 477 (15.3) | 907 (25.4) | 2,097 (24.8) | 390 (23.0) | 2,932 (40.5) |
| Dental checkup‡ | 12,296 (46.4) | 1,211 (37.1) | 1,741 (44.2) | 4,041 (43.8) | 928 (47.5) | 4,375 (55.7) |
| No mammogram§ | 2,965 (27.8) | 180 (23.9) | 470 (29.9) | 958 (23.2) | 178 (34.9) | 1,179 (32.2) |
| No pap test¶ | 2,575 (18.8) | 183 (17.9) | 342 (15.5) | 857 (16.6) | 199 (21.8) | 994 (23.1) |
| No colorectal screening** | 5,034 (40.7) | 625 (38.0) | 655 (51.2) | 1,771 (38.6) | 295 (54.7) | 1,688 (39.1) |
| Total | 24,141 (100) | 3,016 (15.0) | 3,590 (15.5) | 8,388 (34.8) | 1,762 (6.8) | 7,385 (28.0) |
Uninsured part of the year and privately or publicly insured the rest of the year.
Delayed or forgone medical or dental care or prescription.
Less than one dental checkup per year.
More than 2 years since last mammogram, or never; only women 40 years and older were included (n = 9,997).
More than 3 years since last pap test, or never; only women were included (n = 13,504).
Never had colonoscopy, sigmoidoscopy, or blood stool test; only men and women 50 years and older were included (n = 11,534).
Results of the multinomial model of health insurance are shown in Table3. While adjusting for covariates, those with cognitive disabilities or more than one type of disability were significantly more likely than the reference group (those with hearing impairment only) to be publicly insured all year, uninsured part of the year, or uninsured all year. Those with vision impairment were more likely to be uninsured part of the year or uninsured all year, and those with physical disabilities were more likely to be uninsured all year.
Table 3.
Health Insurance by Disability Type among Adults Aged 18–64 Years with Disabilities in the Medical Expenditure Panel Survey Household Component 2002–2008*
|
Results† |
||||
|---|---|---|---|---|
| Outcome | Disability Type | AOR‡ | 95% CI | p |
| Publicly insured all year | Hearing | Reference | ||
| Vision | 0.90 | 0.71, 1.14 | .38 | |
| Physical | 0.89 | 0.70, 1.12 | .32 | |
| Cognitive | 2.45 | 1.85, 3.24 | <.01 | |
| >One | 1.51 | 1.21, 1.90 | <.01 | |
| Uninsured part of the year§ | Hearing | Reference | ||
| Vision | 1.37 | 1.13, 1.65 | <.01 | |
| Physical | 1.16 | 0.96, 1.39 | .12 | |
| Cognitive | 1.80 | 1.40, 2.30 | <.01 | |
| >One | 1.42 | 1.15, 1.77 | <.01 | |
| Uninsured all year | Hearing | Reference | ||
| Vision | 1.58 | 1.30, 1.91 | <.01 | |
| Physical | 1.33 | 1.12, 1.59 | <.01 | |
| Cognitive | 1.64 | 1.27, 2.11 | <.01 | |
| >One | 1.85 | 1.55, 2.21 | <.01 | |
The category “privately insured all year” served as the base group in multinomial logistic regression.
IOM models were adjusted for perceived physical and mental health status, body mass index, diabetes, arthritis, stroke, cardiovascular disease, lung disease, gender, age, race/ethnicity, and complex activity limitation.
Adjusted odds ratio (AOR) 95% confidence interval (CI) and p-value for variable by multinomial logistic regression model.
Uninsured part of the year and privately or publicly insured the rest of the year.
There were several statistically significant associations for the remaining health care access variables and for receipt of clinical preventive services (Table4). Those with vision impairment were more likely than the reference group to report no usual source of care, delayed or forgone care, less than one dental checkup per year, and never having had colorectal screening. Individuals with physical disabilities had greater odds of reporting delayed or forgone care as well as no colorectal screening. No usual source of care, delayed or forgone care, less than one dental checkup per year, and more than 2 years since last mammogram were all more likely among people with multiple limitations. People with cognitive limitations had higher odds of never having had colorectal screening.
Table 4.
Health Care Access and Utilization Outcomes among Adults Aged 18–64 Years with Disabilities in the Medical Expenditure Panel Survey Household Component 2002–2008
|
Results* |
||||
|---|---|---|---|---|
| Outcome | Disability Type | AOR† | 95% CI | p |
| No usual source of care | Hearing | Reference | ||
| Vision | 1.37 | 1.17, 1.61 | <.01 | |
| Physical | 1.16 | 1.00, 1.35 | .05 | |
| Cognitive | 1.19 | 0.97, 1.46 | .10 | |
| >One | 1.34 | 1.14, 1.57 | <.01 | |
| Delayed or forgone medical or dental care or prescription | Hearing | Reference | ||
| Vision | 1.69 | 1.43, 1.99 | <.01 | |
| Physical | 1.35 | 1.17, 1.56 | <.01 | |
| Cognitive | 1.13 | 0.93, 1.37 | .23 | |
| >One | 2.39 | 2.04, 2.79 | <.01 | |
| Less than one dental checkup per year | Hearing | Reference | ||
| Vision | 1.38 | 1.21, 1.58 | <.01 | |
| Physical | 1.11 | 0.98, 1.25 | .09 | |
| Cognitive | 1.10 | 0.94, 1.29 | .24 | |
| >One | 1.44 | 1.27, 1.64 | <.01 | |
| More than 2 years since last mammogram, or never‡ | Hearing | Reference | ||
| Vision | 1.24 | 0.95, 1.62 | .11 | |
| Physical | 0.97 | 0.75, 1.24 | .79 | |
| Cognitive | 1.36 | 0.97, 1.91 | .08 | |
| >One | 1.30 | 1.02, 1.67 | .03 | |
| More than 3 years since last pap test, or never§ | Hearing | Reference | ||
| Vision | 0.91 | 0.70, 1.19 | .50 | |
| Physical | 0.79 | 0.62, 1.01 | .06 | |
| Cognitive | 1.17 | 0.82, 1.67 | .38 | |
| >One | 1.02 | 0.80, 1.31 | .86 | |
| Never had colonoscopy, sigmoidoscopy, or blood stool test¶ | Hearing | Reference | ||
| Vision | 1.55 | 1.27, 1.89 | <.01 | |
| Physical | 1.19 | 1.01, 1.40 | .04 | |
| Cognitive | 1.66 | 1.26, 2.17 | <.01 | |
| >One | 1.16 | 0.98, 1.38 | .09 | |
Models were adjusted for perceived physical and mental health status, body mass index, diabetes, arthritis, stroke, cardiovascular disease, lung disease, gender, age, race/ethnicity, and complex activity limitation.
Adjusted odds ratio (AOR) 95% confidence interval (CI) and p-value for variable by logistic regression model.
Only women 40 years and older were included (n = 9,997).
Only women were included (n = 13,504).
Only men and women 50 years and older were included (n = 11,534).
Discussion
Our hypotheses regarding health care disparities by type of disability were partially supported. As we hypothesized, people in cognitive, physical, and multiple disability type groups were more likely to have problems with health care access and receipt of preventive services and other needed care. People with multiple types of limitations appeared especially vulnerable with regard to both health care access and receipt of health care. People with cognitive disabilities had significantly poorer access to health insurance than the hearing impairment reference group and were the group least likely to have received colorectal cancer screening. People with physical disabilities also had reduced odds of colorectal cancer screening, as well as increased odds of delaying or forgoing needed care. However, contrary with our expectations, people with vision impairment were not similar to those with hearing impairment. In fact, people with vision impairment had elevated odds of experiencing more types of unmet need than any other group except those with multiple types of disabilities. The high number of health care disparities experienced by people with vision impairment suggests that the communication and other barriers faced by people with vision impairment (O'Day, Killeen, and Iezzoni 2004) may interfere with their ability to establish a usual source of care and obtain needed care on a timely basis.
Based on prior findings about barriers to care for people with physical disabilities (e.g., Iezzoni, Kilbridge, and Park 2010; Story, Kailes, and MacDonald 2010), we suspect the unmet needs we observed for this group were also related to environmental barriers. The impacts of such barriers might have been even more apparent had we not controlled for complexity (i.e., severity) of disability (Iezzoni, Frakt, and Pizer 2011). Similarly, for people with more than one type of disability, disparities in having a usual source of care and receiving needed care may be related to greater environmental barriers experienced by people with multiple disabilities. Yankaskas et al. (2010) surveyed women with vision, hearing, physical, or multiple disabilities on reasons for not returning for regular mammograms. They found that women with multiple limitations were much more likely to report problems with transportation, parking, and accessibility of health care facilities, as well as lack of a physician recommendation for screening. Unfortunately, we were not able to explore these barriers directly in our analyses. Although MEPS contains data on reasons for forgoing or delaying some types of care, the list of reasons does not address accessibility and attitudinal barriers faced by many people with disabilities. Further work to identify and reduce health care barriers encountered by people with specific types or combinations of disabilities is a key component of eliminating disability-related health disparities.
Our findings highlight noteworthy differences between people with different types of disabilities. The magnitude of most of our significant effects was modest. Yet, even relatively small effects are indicative of impacts for substantial numbers of people when considered at the population level. For example, we found an odds ratio of 1.37 for people with vision impairment not having a usual source of care. The weighted percentages of people with hearing impairment only and with visual impairment only who did not have a usual source of care were 19.1 and 26.7 percent, respectively (see Table2). If there were no disparity in usual source of care between these groups, the percentages should be equal or close to equal. Given our total weighted count of 5,088,305 people with vision impairment, the observed 7.6 percentage point difference from the reference group in having no usual source of care corresponds to a weighted count of 386,711 additional people with visual impairment who do not have a usual source of care. In other words, nearly 400,000 more people with vision impairment are without a usual source of care than would be expected if the odds ratio had been 1.0. The subgroup differences we identified suggest that type of disability is important to consider when developing and implementing interventions to reduce health care disparities. Interventions can be targeted to the most critical needs of specific disability groups rather than taking a one-size-fits-all approach. However, there were some inconsistent patterns in our results. For example, while people with cognitive disabilities had relatively high odds of being uninsured, they did not differ significantly from the reference group in having a usual source of care or having unmet health care needs, with the exception of colorectal cancer screening. Additional research is needed to better understand these patterns, and the full range of factors that may contribute to or protect against unmet needs.
All of our findings must be placed in the context of current and impending changes in the U.S. health care system, which may help address some of the disparities we observed. Public Law 111-148, the Patient Protection and Affordable Care Act (ACA), forbids denial of insurance coverage to individuals with pre-existing conditions and prohibits rescinding coverage after a person acquires a new condition. People with disabilities will therefore have greater access to affordable health insurance than has previously been the case. Furthermore, Medicaid coverage will be expanded to cover more people, at least in some states. Many people with disabilities are already eligible for public insurance based on their disability, but substantial numbers remain uninsured. Increased coverage, particularly in states participating in Medicaid expansion, should reduce the extent to which lack of health insurance is a barrier to getting health care. These transitions create an exciting opportunity for future research to study the impacts of expanded coverage and evaluate how health care access and receipt may change from the results reported here. Due to anticipated differences by state, much of the research in this area may need to be conducted at a state, rather than national, level. When national studies are conducted, they will need to take into account state health care policy variations to the extent possible. Thus, data sources that facilitate state-level analyses will be especially useful for future research.
Other important changes under the ACA include mandated coverage of preventive care and elimination of caps on benefits, both of which will improve ability to afford needed care. Of particular relevance to people with disabilities, Section 5307 of the ACA calls for educating health care professionals on working with individuals with disabilities. It is important that any such training efforts address issues related to lack of respect and communication problems particularly noted by people with vision impairments (O'Day, Killeen, and Iezzoni 2004), as well as working with people with cognitive impairments who may have low health literacy (Iezzoni, Frakt, and Pizer 2011). Training is also needed on logistical issues (e.g., clinic accessibility; transferring and positioning) associated with providing exams to people with physical disabilities. Requirements in Section 4203 of the ACA pertaining to accessible exam equipment may further reduce physical access barriers. Ongoing research is needed to assess possible reductions in disparities as these components of the ACA are implemented. Based on our findings, it will be important to analyze disparities separately for people with different types of disabilities in addition to considering overall trends for people with disabilities.
Limitations
The MEPS is a rich source of population-based data on health care use. The household survey does have limitations in that data on receipt of clinical preventive services are based on respondent report rather than medical records. As such, the data are subject to possible errors in respondent memory, particularly with regard to how recently a screening or vaccination was received (Rauscher et al. 2008; Cronin et al. 2009). In addition, the cross-sectional nature of our analyses does not allow determinations of cause and effect. Our analyses do not elucidate whether a given type of disability preceded problems with access to or receipt of health care. Some disabilities could have arisen after a long history of substandard health care, but the MEPS does not provide data on such long-term patterns. Our analyses utilized data from 2002 to 2008. Although data from 2009 to 2010 are also now available, we did not include them because U.S. Preventive Services Task Force recommendations regarding mammography receipt changed in 2009 (U.S. Preventative Services Task Force 2009) and there are not yet sufficient data to analyze compliance with the updated recommendations by disability type. For consistency, we also limited our analyses of other health care access variables to the 2002–2008 period. As additional years of data become available, future studies should revisit our analyses. There may also be potential for considering secular trends across time, particularly after key provisions of the ACA take effect.
Conclusions
Prior research has established disparities between people with and without disabilities with regard to access to health care and receipt of clinical preventive services. However, the population of people with disabilities is quite heterogeneous. People with different types of disabilities may encounter differing barriers to health care. Our findings indicate that working-age adults with vision impairment or with multiple types of limitations are at especially high risk of having reduced access to health care and unmet needs for clinical preventive services and other health care. People with cognitive or physical disabilities also experienced significant disparities in access to health insurance and/or receipt of health care. Further and more in-depth research is needed to identify the specific causes of these disparities and develop interventions to address the barriers faced by these particularly vulnerable groups.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported in part by grant H133A080031 from the National Institute on Disability and Rehabilitation Research, U.S. Department of Education. However, the contents do not necessarily represent the policy of the Department of Education, and you should not assume endorsement by the Federal Government. Additional support was provided by cooperative agreement U59DD00942 from the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention; grant 90DD0684 from the Administration on Intellectual and Developmental Disabilities; and the Institute on Development and Disability at Oregon Health and Science University. The authors thank Henry T. Ireys, Ph.D., for his input during the development of the research design; Barbara M. Altman, Ph.D., Elizabeth K. Rasch, P.T., Ph.D., and Stephen P. Gulley, Ph.D., M.S.W., for consultation on identifying people with disabilities in MEPS data; and Amy Sharer for assistance with reference formatting.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Author Matrix.
Operational Definitions of Disability Types — Medical Expenditure Panel Survey Household Component 2002–2008.
Appendix SA3: Operational Definition of Complex Activity Limitation — Medical Expenditure Panel Survey Household Component 2002–2008.
References
- Agency for Healthcare Research and Quality [AHRQ] National Healthcare Disparities Report 2011. Rockville, MD: AHRQ; 2012. [Google Scholar]
- Altman B. Bernstein A. Disability and Health in the United States, 2001–2005. Hyattsville, MD: National Center for Health Statistics; 2008. [Google Scholar]
- Andresen EM, Peterson-Besse JJ, Krahn GL, Walsh ES, Horner-Johnson W. Iezzoni LI. Pap, Mammography, and Clinical Breast Examination Screening among Women with Disabilities: A Systematic Review. Women's Health Issues. 2013;23(4):e205–14. doi: 10.1016/j.whi.2013.04.002. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan L, Doctor JN, MacLehose RF, Lawson H, Rosenblatt RA, Baldwin L. Jha A. Do Medicare Patients with Disabilities Receive Preventive Services? A Population-Based Study. Archives of Physical Medicine and Rehabilitation. 1999;80:642–6. doi: 10.1016/s0003-9993(99)90166-1. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Chan L, Ciol MA, Shumway-Cook A, Yorkston KM, Dudgeon BJ, Asch SM. Hoffman JM. A Longitudinal Evaluation of Persons with Disabilities: Does a Longitudinal Definition Help Define Who Receives Necessary Care? Archives of Physical Medicine and Rehabilitation. 2008;89:1023–30. doi: 10.1016/j.apmr.2007.10.045. and. “ ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevarley FM, Thierry JM, Gill CJ, Ryerson AB. Nosek MA. Health, Preventive Health Care, and Health Care Access among Women with Disabilities in the 1994-1995 National Health Interview Survey, Supplement on Disability. Women's Health Issues. 2006;16(6):297–312. doi: 10.1016/j.whi.2006.10.002. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Cohen JW, Cohen SB. Banthin JS. The Medical Expenditure Panel Survey: A National Information Resource to Support Healthcare Cost Research and Inform Policy and Practice. Medical Care. 2009;47(7 Suppl 1):S44–50. doi: 10.1097/MLR.0b013e3181a23e3a. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Cronin KA, Miglioretti DL, Krapcho M, Yu B, Geller BM, Carney PA, Onega T, Feuer EJ, Breen N. Ballard-Barbash R. Bias Associated with Self-Report of Prior Screening Mammography. Cancer Epidemiology Biomarkers & Prevention. 2009;18(6):1699–705. doi: 10.1158/1055-9965.EPI-09-0020. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drum CE, Krahn G, Culley C. Hammond L. Recognizing and Responding to the Health Disparities of People with Disabilities. Californian Journal of Health Promotion. 2005;3(3):29–42. and. “. ”. [Google Scholar]
- Erickson W, Lee C. von Schrader S. 2011 Disability Status Report: United States. Ithaca, NY: Cornell University Employment and Disability Institute (EDI); 2012. [Google Scholar]
- Ezzati-Rice TM, Rohde F. Greenblatt J. Sample Design of the Medical Expenditure Panel Survey Household Component, 1998-2007. Rockville, MD: AHRQ; 2008. [Google Scholar]
- Gulley SP. Altman BM. Disability in Two Health Care Systems: Access, Quality, Satisfaction, and Physician Contacts among Working-Age Canadians and Americans with Disabilities. Disability and Health Journal. 2008;1(4):196–208. doi: 10.1016/j.dhjo.2008.07.006. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Gulley SP, Rasch EK. Chan L. When Difference Becomes Disparity: Health Status and Health Service Utilization on the Basis of Race and Ethnicity among U.S. Adults with Disabilities. Denver, CO: Paper presented at the 138th Annual Meeting of the American Public Health Association; 2010. [Google Scholar]
- Havercamp SM, Scandlin D. Roth M. Health Disparities among Adults with Developmental Disabilities, Adults with Other Disabilities, and Adults Not Reporting Disability in North Carolina. Public Health Reports. 2004;119(4):418–26. doi: 10.1016/j.phr.2004.05.006. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni LI. Eliminating Health and Health Care Disparities among the Growing Population of People with Disabilities. Health Affairs. 2011;30(10):1947–54. doi: 10.1377/hlthaff.2011.0613. “. ”. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Frakt AB. Pizer SD. Uninsured Persons with Disability Confront Substantial Barriers to Health Care Services. Disability and Health Journal. 2011;4(4):238–44. doi: 10.1016/j.dhjo.2011.06.001. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Kilbridge K. Park ER. Physical Access Barriers to Care for Diagnosis and Treatment of Breast Cancer among Women with Mobility Impairments. Oncology Nursing Forum. 2010;37(6):711–7. doi: 10.1188/10.ONF.711-717. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni LI, Davis RB, Soukup J. O'Day B. Quality Dimensions That Most Concern People with Physical and Sensory Disabilities. Archives of Internal Medicine. 2003;163(17):2085–92. doi: 10.1001/archinte.163.17.2085. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, O'Day BL, Killeen M. Harker H. Communicating about Health Care: Observations from Persons Who Are Deaf or Hard of Hearing. Annals of Internal Medicine. 2004;140(5):356–62. doi: 10.7326/0003-4819-140-5-200403020-00011. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Jha A, Patrick DL, MacLehose RF, Doctor JN. Chan L. Dissatisfaction with Medical Services among Medicare Beneficiaries with Disabilities. Health Services Research. 2002;83:1335–41. doi: 10.1053/apmr.2002.33986. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Kirby JB, Taliaferro G. Zuvekas SH. Explaining Racial and Ethnic Disparities in Health Care. Medical Care. 2006;44(suppl 5):I64–72. doi: 10.1097/01.mlr.0000208195.83749.c3. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Lê Cook B, McGuire TG. Zaslavsky AM. Measuring Racial/Ethnic Disparities in Health Care: Methods and Practical Issues. Health Services Research. (3, Part II) 2012;47:1232–54. doi: 10.1111/j.1475-6773.2012.01387.x. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JC, Hasnain-Wynia R. Lau DT. Delay in Seeing a Doctor Due to Cost: Disparity between Older Adults with and without Disabilities in the United States. Health Services Research. 2012;47(2):698–720. doi: 10.1111/j.1475-6773.2011.01346.x. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinnis JM, Williams-Russo P. Knickman JR. The Case for More Active Policy Attention to Health Promotion. Health Affairs. 2002;21(2):78–93. doi: 10.1377/hlthaff.21.2.78. and. “. ”. [DOI] [PubMed] [Google Scholar]
- National Organization on Disability and Harris Interactive Inc. Detailed Results from the 2004 NOD/Harris Survey of Americans with Disabilities. New York: National Organization on Disability and Harris Interactive Inc; 2004. [Google Scholar]
- O'Day BL, Killeen M. Iezzoni LI. Improving Health Care Experiences of Persons Who Are Blind or Have Low Vision: Suggestions from Focus Groups. American Journal of Medical Quality. 2004;19(5):193–200. doi: 10.1177/106286060401900503. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Parish SL. Huh J. Health Care for Women with Disabilities: Population-Based Evidence of Disparities. Health and Social Work. 2006;31(1):7–15. doi: 10.1093/hsw/31.1.7. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Ramirez A, Farmer GC, Grant D. Papachristou T. Disability and Preventive Cancer Screening: Results from the 2001 California Health Interview Survey. American Journal of Public Health. 2005;95(11):2057–64. doi: 10.2105/AJPH.2005.066118. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauscher GH, Johnson TP, Cho YK. Walk JA. Accuracy of Self-Reported Cancer-Screening Histories: A Meta-Analysis. Cancer Epidemiology Biomarkers & Prevention. 2008;17(4):748–57. doi: 10.1158/1055-9965.EPI-07-2629. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Scheer J, Kroll T, Neri MT. Beatty P. Access Barriers for Persons with Disabilities: The Consumer's Perspective. Journal of Disability Policy Studies. 2003;13(4):221–30. and. “. ”. [Google Scholar]
- Smedley BD, Stith AY. Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- StataCorp. Stata. College Station, TX: StataCorp; 2011. [Google Scholar]
- Story MF, Kailes JI. MacDonald C. The ADA in Action at Health Care Facilities. Disability and Health Journal. 2010;3(4):245–52. doi: 10.1016/j.dhjo.2010.07.005. and. “. ”. [DOI] [PubMed] [Google Scholar]
- Todd A. Stuifbergen A. Breast Cancer Screening Barriers and Disability. Rehabilitation Nursing. 2012;37(2):74–9. doi: 10.1002/RNJ.00013. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- U.S. Department of Health and Human Services. The Surgeon General's Call to Action to Improve the Health and Wellness of Persons with Disabilities. U.S. Department of Health and Human Services, Office of the Surgeon General; 2005. [PubMed] [Google Scholar]
- U.S. Preventative Services Task Force. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2009;151(10):716–26. doi: 10.7326/0003-4819-151-10-200911170-00008. “. ”. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, Manhapra A, Mallik S. Krumholz HM. Sex and Racial Differences in the Management of Acute Myocardial Infarction, 1994 through 2002. New England Journal of Medicine. 2005;353(7):671–82. doi: 10.1056/NEJMsa032214. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- Yankaskas BC, Dickens P, Bowling JM, Jarman MP, Luken K, Salisbury K, Halladay J. Lorenz CE. Barriers to Adherence to Screening Mammography among Women with Disabilities. American Journal of Public Health. 2010;100(5):947–53. doi: 10.2105/AJPH.2008.150318. and. “. ”. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Matrix.
Operational Definitions of Disability Types — Medical Expenditure Panel Survey Household Component 2002–2008.
Appendix SA3: Operational Definition of Complex Activity Limitation — Medical Expenditure Panel Survey Household Component 2002–2008.


