Figure 5. Central Illustration. Sympathetic and Parasympathetic Stimuli, the QT-Interval, and CVD Events.
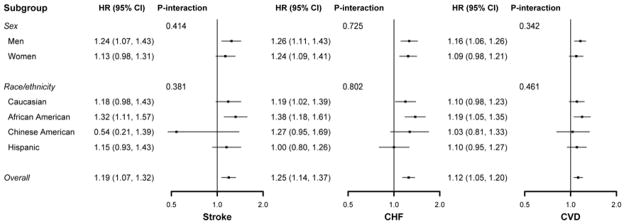
There is a complex interaction between the central nervous system (CNS) sympathetic and parasympathetic stimuli and cardiac conduction intervals. By increasing the heart rate (HR), sympathetic stimulation (green arrows) can secondarily decrease the QT-interval. In contrast, by decreasing the heart rate, parasympathetic stimulation can increase the QT interval (orange arrows). Autonomic stimuli also exert direct effects upon the QT interval. Increased catecholamine levels typically result in QT interval prolongation in healthy individuals (light green arrow). Additionally, high sympathetic tone is associated with the development of atherosclerosis with potential secondary effects upon cardiac repolarization and the QT interval (grey arrows). Left ventricular mass is also positively associated with high sympathetic tone and the QT interval (grey arrows). In this study, we observed positive associations between baseline-corrected QT intervals and risks of incident stroke, HF, and CVD events in a cohort of middle-aged participants free of cardiovascular disease at baseline. Prolongation of the QT interval as a surrogate of elevated sympathetic tone and autonomic imbalance may explain its association with cardiovascular events. However, the QT interval may be associated with other factors, which may mediate its association with cardiovascular events. Please note that the arrows in this illustration are provided to note associations and do not imply causality.
CVD = cardiovascular disease; HR = heart rate; LV = left ventricle.
