Abstract
A 29-year-old woman with known ulcerative colitis developed a right-sided abdominal pain a day after preterm vaginal delivery at 30 weeks. She did not have any nausea, vomiting and had normal bowel movements. The observations were within normal limits and white cell counts were marginally elevated with a normal C reactive protein. A large ovarian vein thrombosis on the left side was an incidental finding on a CT of the abdomen and pelvis undertaken to establish the cause for abdominal pain. The patient was managed by a multidisciplinary team and was treated with anticoagulants for 6 months. This case illustrates that the incidence of pelvic venous thrombosis may be higher in pregnancy and puerperium.
Background
The occurrence of ovarian vein thrombosis (OVT) is uncommon, but can be associated with increased morbidity and mortality if not identified and managed appropriately. We report a case of an incidental finding of left OVT on a CT of the abdomen undertaken for right-sided abdominal pain following preterm vaginal delivery in a woman known to have ulcerative colitis.
Case presentation
A 29-year-old woman, with two previous vaginal deliveries and history of ulcerative colitis, had conceived under mesalazine and methotrexate, but these were stopped in early pregnancy as the symptoms were well controlled. She had reported a flare up of ulcerative colitis at 22 weeks of gestation and was managed with oral steroids and mesalazine. She had a fetal medicine scan at 22 weeks gestation and a further growth scan at 28 weeks, which were normal. She had no personal or family history of thromboembolism. She presented with preterm labour at 30 weeks gestation and delivered within hours of presentation.
The next day the patient reported severe abdominal pain in the right hypochondrium and right iliac fossa. She had no nausea or vomiting, and had normal bowel movements with no rectal bleeding. Her routine observations were satisfactory and abdominal examination was unremarkable.
Investigations
The haemoglobin concentration was 10.1 g/dL, white cell count (WCC) was elevated (19.3×109) and the platelet count was marginally raised at 426×109. The C reactive protein (CRP) was normal (<3). A CT of the abdomen and pelvis was performed to rule out other pathology as the pain did not settle with conservative management. This showed no bowel pathology but demonstrated a left OVT involving most of the vessel length (figure 1). No source of infection was found in the vaginal swab culture or placental culture, however, an Enterococcus infection was detected in the midstream urine culture.
Figure 1.
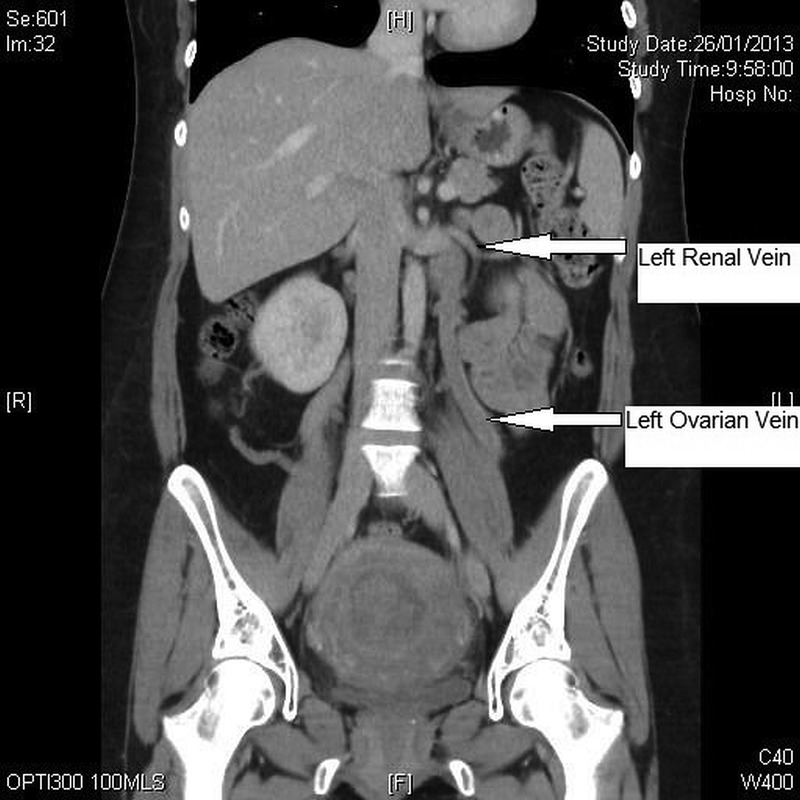
Contrast enhanced CT of abdomen and pelvis demonstrating length of dilated thick walled left ovarian vein (demonstrating thrombosis) merging with left renal vein.
Differential diagnosis
The differential diagnoses were worsening inflammatory bowel disease, acute appendicitis, septic pelvic thrombophlebitis, peritonitis, adnexal torsion, pyelonephritis and tubo-ovarian abscess. Normal bowel habits with no associated nausea and vomiting, and no rectal bleeding was less likely to be of bowel-related pathology. Absence of fever and tachycardia were against acute infective causes. WCC may be raised in pregnancy and in women on corticosteroids, but the CRP was normal.
In our case, though the incidental finding of OVT on the left side was not the likely cause for right-sided abdominal pain, it nevertheless highlights the significance of having pelvic vein thrombosis as a differential diagnosis for abdminopelvic pain in pregnancy.
Treatment
The patient was managed by a multidisciplinary team and was treated with a therapeutic dose of low molecular weight heparin and antithromboembolic stockings. She was also given intravenous antibiotics for a possible abdominal infection at initial presentation and the antibiotics were continued for her urinary tract infection.
Outcome and follow-up
The right-sided abdominal pain settled over the next few days. The patient did not display clinical features of pulmonary embolus or lower limb deep vein thrombosis. Warfarin was given as long-term anticoagulation for 6 months.
Discussion
Thromboembolism is the third most common direct cause for maternal deaths in the UK.1 OVT, first described by Austin in 1956,2 is uncommon, but can potentially be life-threatening during pregnancy. Antenatal OVT appears to be rare,3 and has mainly been recognised and reported in the postnatal period.4 The incidence varies between 1 in 600 to 2000 deliveries.3 5 The risk factors include multiparity, obesity, puerperal endometritis, thrombophilias (acquired and inherited), past and family history of thromboembolism, systemic lupus erythaematosus and smoking.
The pathogenesis of this condition in the postnatal period is not fully understood, but Virchow's triad (blood flow stasis, hypercoagulability and endothelial injury or dysfunction) may well describe the pathogenesis of OVT. The ovarian vein diameter increases in pregnancy with increased blood flow and associated valvular incompetency. Blood flow in these veins in the postnatal period reduces leading to venous collapse and venous blood flow stasis. A state of hypercoagulability in pregnancy persists up to 6 weeks postnatally, and endometritis increases the risk further as the blood flowing from the uterus carries pathogenic bacteria to the ovarian veins causing inflammation and aggravates thrombus formation.6
The right ovarian vein is more prone to thrombosis,7 but it can occur in either or both veins. It is reported to occur predominantly on the right side in about 70–90% of cases and bilaterally in 11–14% of cases.8 9 Multiple incompetent valves, dextrorotation of the gravid uterus causing compression of the vein as it crosses the pelvic brim and relatively longer length appear to increase the risk on the right side.7 10
Multidetector CT has 100% sensitivity in the diagnosis of OVT, but Duplex ultrasonography with a sensitivity of 52% is the preferred first-line of investigation due to availability and safety; also, MRI with 92% sensitivity has no ionising radiation, which is beneficial for younger women.10 Diagnostic delay can be potentially life-threatening with complications such as thrombus extension into the ileofemoral vessels and inferior vena cava, and embolisation into pulmonary vasculature. Approximately one-fourth of untreated patients develop pulmonary embolism and mortality might be about 4%.7 11 12
Long-term anticoagulation remains the mainstay of treatment for OVT. Thrombophilia screening should be undertaken after stopping the anticoagulants. There are no data on the long-term outcome for these patients with regard to subsequent fertility and future pregnancies.
Our patient suffered from severe right-sided abdominal pain without fever in the immediate postnatal period and left OVT was diagnosed incidentally on imaging. This case emphasises that clinicians should have a high level of suspicion for pelvic vein thrombosis as one of the differential diagnoses of acute abdominal pain in pregnancy and postnatal period.
Learning points.
Ovarian vein thrombosis (OVT) is uncommon, with the right ovarian vein being more susceptible.
Although the condition is mostly right sided, OVT can also occur on the left side.
OVT is more common in the postnatal period and the risk is exacerbated by endometritis.
A high level of clinical suspicion for pelvic vein thrombosis is needed.
Long-term anticoagulation reduces associated morbidity and mortality.
Footnotes
Contributors: HMB conceived the idea, collected the data and drafted the manuscript. DJ conceived the idea, collected the data and contributed to the drafting of the manuscript. JS collected the data, and contributed to the idea and drafting of the manuscript. KG conceived the idea and was responsible for overall supervision of the case report.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Centre for Maternal and Child Enquiries (CMACE). Saving Mothers' Lives: reviewing maternal deaths to make motherhood safer: 2006–08. The Eighth Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 2011;118(Suppl 1):1–203. [DOI] [PubMed] [Google Scholar]
- 2.Austin OG. Massive thrombophlebitis of the ovarian veins; a case report. Am J Obstet Gynaecol 1956;72:428–9. [DOI] [PubMed] [Google Scholar]
- 3.Simons GR, Piwnica-Worms DR, Goldhaber SZ. Ovarian vein thrombosis. Am Heart J 1993;126(3 Pt 1):641–7. [DOI] [PubMed] [Google Scholar]
- 4.Kafali H, Onaran YA, Keskin E et al. . Ovarian vein thrombosis and mirror syndrome in association with sacrococcygeal teratoma. Clinics (Sao Paulo) 2010;65:452–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.André M, Delèvaux I, Amoura Z et al. . Ovarian vein thrombosis in the antiphospholipid syndrome. Arthritis Rheum 2004;50:183–6. [DOI] [PubMed] [Google Scholar]
- 6.Takach TJ, Cervera RD, Gregoric ID. Ovarian vein and caval thrombosis. Tex Heart Inst J 2005;32:579–82. [PMC free article] [PubMed] [Google Scholar]
- 7.Kominiarek MA, Hibbard JU. Postpartum ovarian vein thrombosis: an update. Obstet Gynecol Surv 2006;61:337–42. [DOI] [PubMed] [Google Scholar]
- 8.Baran GW, Frisch KM. Duplex Doppler evaluation of puerperal ovarian vein thrombosis. AJR Am J Roentgenol 1987;149:321–2. [DOI] [PubMed] [Google Scholar]
- 9.Prieto-Nieto MI, Perez-Robledo JP, Rodriguez-Montes JA et al. . Acute appendicitis-like symptoms as initial presentation of ovarian vein thrombosis. Ann Vasc Surg 2004;18:481–3. [DOI] [PubMed] [Google Scholar]
- 10.Sharma P, Abdi S. Ovarian vein thrombosis. Clin Radiol 2012;67:893–8. [DOI] [PubMed] [Google Scholar]
- 11.Dunnihoo DR, Gallaspy JW, Wise RB et al. . Postpartum ovarian vein thrombophlebitis: a review. Obstet Gynecol Surv 1991;46:415–27. [DOI] [PubMed] [Google Scholar]
- 12.Benfayed WH, Torreggiani WC, Hamilton S. Detection of pulmonary emboli resulting from ovarian vein thrombosis. AJR Am J Roentgenol 2003;181:1430–1. [DOI] [PubMed] [Google Scholar]


