TABLE III.
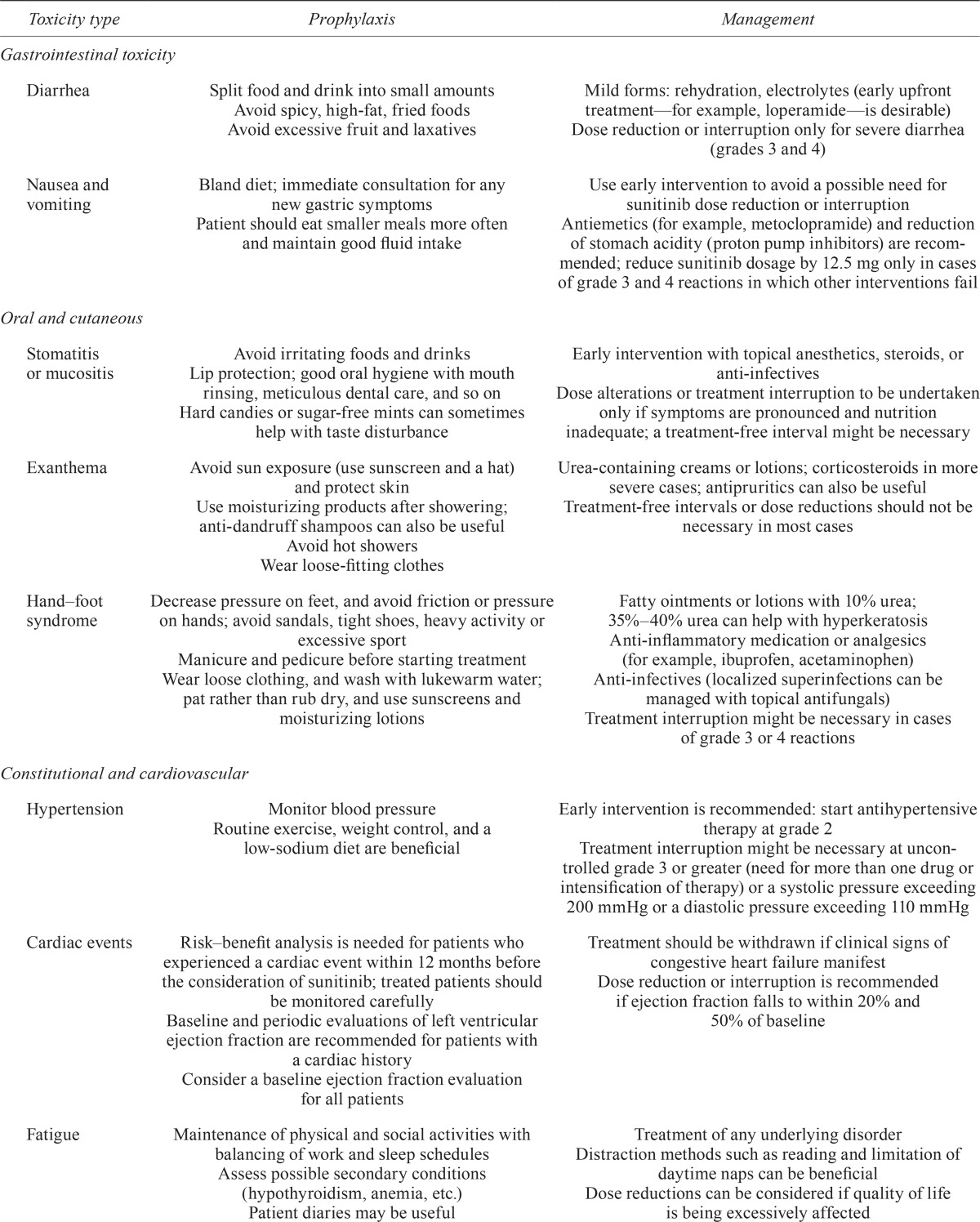
| Toxicity type | Prophylaxis | Management |
|---|---|---|
| Gastrointestinal toxicity | ||
| Diarrhea | Split food and drink into small amounts Avoid spicy, high-fat, fried foods Avoid excessive fruit and laxatives |
Mild forms: rehydration, electrolytes (early upfront treatment—for example, loperamide—is desirable) Dose reduction or interruption only for severe diarrhea (grades 3 and 4) |
| Nausea and vomiting | Bland diet; immediate consultation for any new gastric symptoms | Use early intervention to avoid a possible need for sunitinib dose reduction or interruption |
| Patient should eat smaller meals more often and maintain good fluid intake | Antiemetics (for example, metoclopramide) and reduction of stomach acidity (proton pump inhibitors) are recommended; reduce sunitinib dosage by 12.5 mg only in cases of grade 3 and 4 reactions in which other interventions fail | |
| Oral and cutaneous | ||
| Stomatitis or mucositis | Avoid irritating foods and drinks Lip protection; good oral hygiene with mouth rinsing, meticulous dental care, and so on Hard candies or sugar-free mints can sometimes help with taste disturbance |
Early intervention with topical anesthetics, steroids, or anti-infectives Dose alterations or treatment interruption to be undertaken only if symptoms are pronounced and nutrition inadequate; a treatment-free interval might be necessary |
| Exanthema | Avoid sun exposure (use sunscreen and a hat) and protect skin Use moisturizing products after showering; anti-dandruff shampoos can also be useful Avoid hot showers Wear loose-fitting clothes |
Urea-containing creams or lotions; corticosteroids in more severe cases; antipruritics can also be useful Treatment-free intervals or dose reductions should not be necessary in most cases |
| Hand–foot syndrome | Decrease pressure on feet, and avoid friction or pressure on hands; avoid sandals, tight shoes, heavy activity or excessive sport Manicure and pedicure before starting treatment Wear loose clothing, and wash with lukewarm water; pat rather than rub dry, and use sunscreens and moisturizing lotions |
Fatty ointments or lotions with 10% urea; 35%–40% urea can help with hyperkeratosis Anti-inflammatory medication or analgesics (for example, ibuprofen, acetaminophen) Anti-infectives (localized superinfections can be managed with topical antifungals) Treatment interruption might be necessary in cases of grade 3 or 4 reactions |
| Constitutional and cardiovascular | ||
| Hypertension | Monitor blood pressure Routine exercise, weight control, and a low-sodium diet are beneficial |
Early intervention is recommended: start antihypertensive therapy at grade 2 Treatment interruption might be necessary at uncontrolled grade 3 or greater (need for more than one drug or intensification of therapy) or a systolic pressure exceeding 200 mmHg or a diastolic pressure exceeding 110 mmHg |
| Cardiac events | Risk–benefit analysis is needed for patients who experienced a cardiac event within 12 months before the consideration of sunitinib; treated patients should be monitored carefully Baseline and periodic evaluations of left ventricular ejection fraction are recommended for patients with a cardiac history Consider a baseline ejection fraction evaluation for all patients |
Treatment should be withdrawn if clinical signs of congestive heart failure manifest Dose reduction or interruption is recommended if ejection fraction falls to within 20% and 50% of baseline |
| Fatigue | Maintenance of physical and social activities with balancing of work and sleep schedules Assess possible secondary conditions (hypothyroidism, anemia, etc.) Patient diaries may be useful |
Treatment of any underlying disorder Distraction methods such as reading and limitation of daytime naps can be beneficial Dose reductions can be considered if quality of life is being excessively affected |
| Laboratory tests | ||
| Hypothyroidism | Routine monitoring after baseline measurement is recommended | Continue laboratory monitoring and treat per standard practice (hormone replacement) Treatment interruption is unlikely to be necessary |
| Hematology and liver function | Complete blood workup to be done before treatment (each cycle) | Treatment interruption or dose reduction suggested for grades 3 and 4 abnormalities Treatment withdrawal if results fail to return to normal |
| Hypophosphatemia | Electrolyte control Include serum phosphate in laboratory analyses to be done before each treatment cycle |
Alimentary substitution Treatment interruption or dose reduction should not be necessary |
