Abstract
Introduction
Acute kidney injury (AKI) occurs frequently after liver transplantation and is associated with significant morbidity and mortality. Recent evidence has linked the predominant usage of ‘chloride-liberal’ intravenous fluids, such as 0.9% saline to the development of renal dysfunction in general critically ill patients. We compared the effects of perioperative fluid types on AKI in liver transplant recipients.
Methods
An observational analysis of liver transplant recipients over a 33-month period, between January 2010 and September 2013, was performed. Intensive care unit database and patient records were analyzed for determinants of early postoperative AKI. Univariate and multivariate regression analysis was carried out using a two-tailed P value less than 0.05 to establish significance. The institutional Research Ethics Committee approved the study methodology (RAC no. 2131 073).
Results
One hundred and fifty-eight liver transplants were performed, AKI developed in 57 (36.1%) patients: 39 (68.4%) fully recovered, 13 (22.8%) developed chronic renal failure and 10 (17.5%) required long-term hemodialysis. On univariate regression analysis, AKI was significantly associated with greater than 3,200 ml of chloride-liberal fluids infused within the first postoperative day (HR 5.9, 95% CI 2.64, 13.2, P <0.001), greater than 1,500 ml colloids received in the operating room (hazard ratio (HR) 1.97, 95% CI 1.01, 3.8, P = 0.046), vasopressor requirement for 48 hours posttransplant (HR 3.34, 95% CI 1.55, 7.21, P = 0.002), hyperchloremia at day 2 (HR 1.09, 95% CI 1.01, 1.18, P = 0.015) and preoperative model for end-stage liver disease (MELD) score (HR 1.08, 95% CI 1.03, 1.13, P <0.001).
After stepwise multivariate regression, infusion of greater than 3,200 ml of chloride-liberal fluids (HR 6.25, 95% CI 2.69, 14.5, P <0.000) and preoperative MELD score (HR 1.08, 95% CI 1.02, 1.15, P = 0.004) remained significant predictors for AKI.
Conclusions
In a sample of liver transplant recipients, infusion of higher volumes of chloride-liberal fluids and preoperative status was associated with an increased risk for postoperative AKI.
Introduction
Acute kidney injury (AKI) occurs both frequently after liver transplantation, reportedly in 29 to 60% recipients [1-3] and, irrespective of severity, confers an increased risk of death [4]. This increase in risk of mortality extends from the early postoperative period (28 days) and up to one year after transplantation [1]. The National Institute of Diabetes and Digestive and Kidney Disease (NIDDK) long-term follow-up study ascribed a 2.66 hazard ratio (HR) directly attributable to renal dysfunction developing after liver transplantation [5].
Previously described risk factors for AKI in liver recipients are greater severity of illness pretransplant (higher model for end-stage liver disease (MELD) scores, intensive care unit (ICU) admission, and coagulopathy), vasopressors, and greater transfusions in the immediate perioperative period [5-13]. However, very little is known about the effects of intravenous fluid selection (chloride-liberal versus chloride-restrictive) or the effects of fluid balance on the risk of renal injury. An overall fluid overload state leads to renal congestion, compromised renal blood flow and reductions in glomerular filtration rate (GFR) [14]. In critically ill patients, a positive fluid balance has been associated with increased mortality [15,16] and poorer outcomes once AKI develops [17-19]. Recent evidence has highlighted the possible nephrotoxic effects of ‘chloride-liberal’ fluids (0.9% saline). Animal and human controlled studies have shown that infusions of chloride-liberal or solutions with supraphysiological chloride concentrations cause vasoconstriction of renal afferent arterioles, cortical hypoperfusion and decreased GFR [20-22]. In a recent pre- and postintervention study, restriction to chloride-restrictive fluids was associated with lower AKI and need for renal replacement therapy (RRT) as compared to chloride-liberal fluids [23]. Therefore, perioperative intravenous fluid selection and volume may prove to be a modifiable risk factor for the prevention of AKI. No similar data exists for liver transplant recipients. These patients clearly are at an increased risk of renal injury with mortal consequences. We hypothesized that AKI occurring in the early postoperative period after liver transplant may be associated with the use of chloride-liberal fluids and overall fluid overload causing renal congestion.
Material and methods
This study is reported following the STROBE statement checklist for observational studies [24]. All studies at our institution require ethical approval; the Office of Research Affairs (ORA) and ORA Research Ethics Committee approved the study (RAC no. 2131 073). Patient consent was waived by the Research Ethics Committee.
Study design and setting
This was an observational study of liver transplant recipients carried out at a tertiary care, university hospital over a 33-month period between January 2010 and September 2013.
Operational definitions
AKI was defined according to the risk, injury, failure, loss, end-stage renal failure (RIFLE) classification [25] of renal dysfunction, that is using both increases in creatinine from preoperative values and urine output measured as urine volume in milliliters/patient’s baseline weight in kilograms/hour. Serum creatinine values were measured preoperatively and daily for up to the third postoperative day. Serum creatinine was measured using the COBAS Integra Creatinine plus ver. 2 assay (Roche Diagnostics Corp, Basel, Switzerland). This is an enzymatic method based on the determination of hydrogen peroxide after conversion of creatinine with the aid of creatininase, creatinase, and sarcosine oxidase. Patients were screened for the development of postoperative AKI on a daily basis until the third day.
Prolonged ICU stay was defined a priori as a cutoff value of the mean (or median for skewed data) ICU days after transplantation. Delayed weaning from mechanical ventilation was defined as <3 > days of invasive ventilation.
Chloride-liberal fluids were fluids containing supraphysiological concentrations of chloride (0.9% saline, 20% and 5% albumin); chloride-restrictive fluids were fluids with chloride concentrations closer to plasma (0.45% saline, Ringer’s lactate).
Participants
Consecutive adult liver transplant recipients within the specified study period were included. Patients undergoing multiorgan transplantation were excluded.
Crystalloids used in the study patients were: lactated Ringer’s (sodium chloride, potassium chloride, sodium lactate and calcium chloride) injection, 0.9% sodium chloride injection, USP, 0.45% sodium chloride injection, USP, manufactured by Baxter Healthcare Corp, Deerfield IL, USA. Colloids used were: human albumin 5% and 20% manufactured by Biotest Pharma GmbH, Dreieich, Germany.
Variables
The primary outcome variable was the development of postoperative AKI. Other outcome variables studied were delayed weaning from mechanical ventilation, prolonged ICU stay (as defined above), ICU mortality, and 28-day mortality. Other variables collected were recipient demographic data, etiology of cirrhosis, comorbidities, posttransplant acute physiologic and chronic health evaluation II (APACHE II) scores, routine hematological, biochemical and organ dysfunction/physiological (AKI, vasopressors, RRT, mechanical ventilation) data, fluid balance, fluids and blood products received at admission to ICU and daily up to day 3 posttransplantation.
Data sources/measurement
In our ICU, patient data is routinely entered into an ICU database. Data entry is by a critical care nurse dedicated to the database. Patient data required for the study and missing from the database was extracted by the research team (AH, HS, BB, AN) from the patient’s electronic medical records and laboratory computerized results.
Statistical analysis
Continuous data was tested for normality: measures of central tendency were compared as means ± standard deviations (SD) using the Student’s t test for normally distributed variables and as medians (interquartile range, IQR) using the Mann-Whitney U test for skewed data. Categorical variables were compared using the chi-square test or the Fisher exact test for n <5. Fluid volumes were dealt with as continuous variables while fluid types were classified into either ‘chloride-liberal’ or ‘chloride-restrictive’ and correspondingly dealt with as continuous variables. Logistic regression analysis was performed to determine the predictive ability of variables for AKI, prolonged ICU stay and prolonged mechanical ventilation. Univariate and multivariate techniques were used, and for multivariate regression, a backward mode with a threshold 0.15 was used for elimination. Multivariate associations were reported as odds ratios (OR) with 95% confidence intervals (CIs). A two-sided P value of <0.05 was considered as statistically significant. All analyses were carried out using IBM SPSS version 22.0 (IBM Corp, Armonk, NY, USA).
Results
Participants and descriptive data
One hundred and fifty-eight liver transplants were performed during the study period. Of these, 104 (65.8%) were living donor-related transplants, 53 (33.5%) cadaveric and 1 (0.6%) was a retransplant. Mean age of transplant recipients was 52.3 ± 13.3 years and 66 (42%) were female, mean body mass index (BMI) was 26.8 ± 6 (range 14, 49). Mean MELD score at time of transplantation was 19.4 ± 7.7 (range 6, 45), with mean baseline creatinine 88.7 micromol/L ± 56 (range 27, 350). Transplant recipients had end-stage liver disease caused by: hepatitis C in 60 (38%) patients, hepatitis B in 34 (21.5%), cryptogenic liver disease in 41 (25.9%), autoimmune disease in 9 (5.7%) and others (bilharziasis, congenital hepatic cirrhosis, Budd-Chiari, Wilson’s disease) in 14 (9%) recipients. Fifty-two (32.9%) patients had hepatocellular carcinomas.
All patients were transferred to the ICU posttransplant. On arrival, transplant recipients were in a positive fluid balance of 8.48 ± 2.3 liters fluid, having received 1.7 ± 0.26 L packed red cells, 3.8 ± 0.143 L blood products (plasma, cryoprecipitate, platelets) and a mean of 7.8 ± 6.3 L crystalloids of which 5.6 ± 4.0 L were chloride-liberal and 2.4 ± 1.4 L were chloride-restrictive fluids. Mean APACHE II score was 15.9 ± 5.4 (range 4, 48), serum procalcitonin level 2.4 ngm/ml (IQR 3.1), proBNP 476 pg/mL (IQR 2,510) and 120 (76%) patients were on a norepinephrine infusion. Seventy-eight (49.4%) had pleural effusions; pleural drainage by pigtail catheters was carried out in 23 out of 78 patients (29.4%). In the first 72 hours of ICU stay, transplant recipients were in a cumulative positive fluid balance of 12.7 ± 7.8 L with 9 ± 6 L crystalloids, 6.4 ± 3.5 L colloids (5%, 20% albumin) and 25 ± 11.9 L chloride-liberal (0.9% saline, 5% albumin, 20% albumin) received. Blood products transfused were 4 L (IQR 4.8). There was no significant difference between the mean serum chloride levels in the chloride-liberal group compared to the chloride-restrictive group, 114 ± 5.8 versus 113 ± 5.9, P >0.05. No significant correlation was found between the mean serum chloride concentrations and the cumulative volumes of chloride-liberal fluids given, P >0.05 (see Table 1 and Figure 1).
Table 1.
Chemical compositions of fluids used in liver transplant recipients
| Fluid-type | Composition per 1 liter | Manufacturer |
|---|---|---|
| crystalloids | ||
| 0.9% Sodium chloride, USP | 154 mEq Sodium | Baxter Healthcare Corp, Deerfield, IL, USA |
| 154 mEq Chloride | ||
| 0.45% Sodium chloride, USP | 77 mEq Sodium | Baxter Healthcare Corp, Deerfield, IL, USA |
| 77 mEq Chloride | ||
| Lactated Ringer’s injection, USP | 130 mEq Sodium | Baxter Healthcare Corp, Deerfield, IL, USA |
| 4 mEq Potassium | ||
| 3 mEq Calcium | ||
| 109 mEq Chloride | ||
| 28 mEq Sodium lactate | ||
| Colloids | ||
| Human albumin 5% biotest | Plasma protein 50gm (96% albumin), caprylate (4 mmol/l), N-acetyl-DL-tryptophanate (4 mmol/l), sodium ions (145 mmol/l), water for injections ad 1,000 ml | Biotest Pharma GmbH |
| Dreieich, Germany | ||
| Human albumin 20% biotest (given diluted in 0.9% normal saline) | 200 g/l (at least 95% is human albumin) | Biotest Pharma GmbH |
| Dreieich, Germany |
Figure 1.
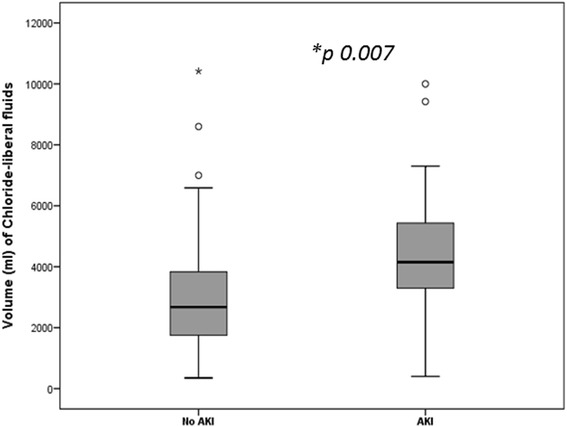
Relative volumes of chloride-liberal fluids received by liver transplant recipients with and without acute kidney injury (AKI).
Median ICU length of stay was five days (IQR 6), mean 8.4 ± 12.5 days. Patients were ventilated for a median of two days (IQR 2) with nine (5.7%) patients subsequently undergoing tracheostomy. ICU mortality was 8.2% (13 patients); 28-day survival was 140 (88.6%). Eight (5%) recipients were readmitted to the ICU for the following: respiratory failure two, sepsis three, bleeding three. Mean time to readmission was 3.5 ± 1.1 days (2, 5).
Outcomes
AKI developed in 58 (36.4%) patients; classified as risk in 30 (52%), injury in 12 (21%) and failure in 16 (27%) patients. Ninety percent (53 patients) developed AKI within the first two postoperative days. All liver transplant patients, both the group that developed AKI and those that did not were on the calcineurin inhibitor, tacrolimus. Drug levels were routinely monitored and dosing adjusted accordingly. Thirty-nine (68.4%) patients recovered fully, 13 (22.8%) developed chronic renal failure and 10 (17.5%) required long-term hemodialysis. AKI was significantly associated with ICU mortality, P = 0.001 and 28-day mortality, P <0.001. Mean serum chloride levels on the second postoperative day were significantly greater in patients who developed AKI compared to those who did not; 114 ± 7.2 versus 112 ± 4.4, P = 0.01. The mean chloride levels on days one and three were not significantly different. There were no significant associations between mean serum chloride levels and the severity of renal failure (see Table 2).
Table 2.
Characteristics of liver transplant patients grouped by acute kidney injury according to the RIFLE classification
| No AKI (n = 101) | AKI (n =57) | P value | |
|---|---|---|---|
| Age, years | 51 ± 14.2 | 54 ± 11.3 | 0.13 |
| BMI | 26.4 ± 6 | 27.7 ± 6.6 | 0.19 |
| Pretransplant creatinine, micromol/L | 76.2 ± 40.2 | 110.8 ± 72.6 | 0.001 |
| Pretransplant MELD score | 19.2 ± 5.4 | 21.8 ± 9.1 | 0.001 |
| Volume of chloride-liberal fluids, liters (IQR) | |||
| Operating room | 4.7 (5.7) | 6 (6.8) | 0.23 |
| 24 hours | 2.1 (1.2) | 3.8 (2.7) | <0.001 |
| 48 hours | 0.64 (1.06) | 1.7 (1.5) | 0.007 |
| 72 hours | 0.35 (0.65) | 1.07 (0.87) | 0.55 |
| Volume of chloride-restrictive fluids, liters (IQR) | |||
| Operating room | 2 (2) | 2 (1.2) | 0.46 |
| 24 hours | 1.9 (1.28) | 1.8 (1.4) | 0.32 |
| 48 hours | 2.0 (0.76) | 1.9 (1.6) | 0.86 |
| 72 hours | 1.3 (1.0) | 1.6 (1.1) | 0.67 |
| Volume of colloids, liters (IQR) | |||
| Operating room | 1.5 (1) | 2.1 (2.5) | 0.013 |
| 24 hours posttransplant | 1.2 (1.03) | 1.9 (1.4) | 0.001 |
| 48 hours posttransplant | 0.45 (0.85) | 0.95 (0.71) | 0.016 |
| 72 hours posttransplant | 0.35 (0.65) | 1.0 (0.87) | 0.05 |
| Volume of packed RBC transfusions, liters (IQR) | |||
| Operating room | 1.5 (1.2) | 2.2 (1.9) | 0.022 |
| 24 hours | 0.76 (0.44) | 1.14 (5.8) | 0.19 |
| 48 hours | 0.53 (0.38) | 0.72 (0.53) | 0.08 |
| 72 hours | 0.38 (0.71) | 0.38 (0.06) | 0.89 |
| Volume of blood products transfused, liters (IQR) | |||
| Operating room | 3.2 (2.3) | 3.8 (3.2) | 0.17 |
| 24 hours | 0.95 (2.1) | 2.1 (4.8) | 0.14 |
| 48 hours posttransplant | 0.72 (0.53) | 0.97 (1.2) | 0.63 |
| 72 hours posttransplant | 0.63 (1.5) | 0.51 (0.32) | 0.78 |
| Volume of crystalloids infused, liters (IQR) | |||
| Operating room | 6 (5.6) | 6 (6) | 0.8 |
| 24 hours | 2.5 (1.3) | 3.1 (1.9) | 0.15 |
| 48 hours | 2.1 (0.72) | 2.4 (1.4) | 0.22 |
| 72 hours | 1.6 (0.96) | 1.7 (1.1) | 0.30 |
| Fluid balance, liters (IQR) | |||
| Operating room | 6.4 (4.7) | 6.7 (5.4) | 0.76 |
| 24 hours | 2.9 (2.6) | 3.7 (4.8) | 0.09 |
| 48 hours | 1.6 (1.5) | 1.7 (2.4) | 0.06 |
| 72 hours | 0.947 (2.07) | 0.623 (1.54) | 0.93 |
| Serum lactate, mmol/L | |||
| Day 1 | 4.2 ± 2.9 | 4.8 ± 3.9 | 0.26 |
| Day 2 | 1.8 ± 1.1 | 2.1 ± 1.6 | 0.09 |
| Day 3 | 1.4 ± 0.5 | 1.9 ± 0.3 | 0.046 |
| Serum sodium, mmol/L | |||
| Day 1 | 146 ± 5.2 | 146.5 ± 5.0 | 0.57 |
| Day 2 | 143 ± 5.7 | 145 ± 3 | 0.016 |
| Day 3 | 144 ± 2.3 | 146 ± 2.6 | 0.002 |
| Serum chloride, mmol/L | |||
| Day 1 | 114 ± 5.7 | 113 ± 5.9 | 0.76 |
| Day 2 | 112 ± 4.4 | 114 ± 7.2 | 0.01 |
| Day 3 | 110 ± 4.6 | 111 ± 4.8 | 0.18 |
| Vasopressor requirement | |||
| At admission | 73 (72%) | 47 (82.5%) | 0.25 |
| Day 1 | 3 (3%) | 1 (1.8%) | 0.64 |
| Day 2 | 15 (14.8%) | 21 (36.8%) | 0.002 |
| Day 3 | 4 (4%) | 8 (14%) | 0.056 |
| Days on mechanical ventilation | 2.3 ± 3.6 | 6 ± 7.1 | 0.001 |
| Length of ICU stay after transplant | 5.5 ± 4.7 | 13.4 ± 19 | 0.003 |
AKI, acute kidney injury; BMI, body mass index; ICU, intensive care unit; IQR, interquartile range; MELD, model for end-stage liver disease; RIFLE, risk, injury, failure, loss, end-stage renal failure.
Univariate outcome data
On univariate regression analysis, AKI was significantly associated with greater than 3,200 ml of chloride-liberal fluids infused within the first postoperative day (HR 5.9, 95% CI 2.64, 13.2, P <0.001), greater than 1,500 ml colloids received in the OR (HR 1.97, 95% CI 1.01, 3.8, P = 0.046), vasopressor requirement for 48 hours posttransplant (HR 3.34, 95% CI 1.55, 7.21, P = 0.002), hyperchloremia at day 2 (HR 1.09, 95% CI 1.01, 1.18, P = 0.015) and preoperative MELD score (HR 1.08, 95% CI 1.03, 1.13, P = 0.001).
Delayed weaning from mechanical ventilation was associated with higher volumes of chloride-liberal fluids, P = 0.02, higher colloid volumes, P = 0.015, blood products transfused, P = 0.017 and a cumulative positive fluid balance, P = 0.026. Higher pretransplant MELD scores, P = 0.001, male gender, P = 0.015, transplant for hepatocellular carcinoma, P = 0.014, crystalloid volume received in the first 72 hours, P = 0.034, need for vasopressors at 48 hours, P <0.001 and 72 hours, P = 0.031, AKI, P <0.001 and pleural effusion, P = 0.001 were significantly associated with a prolonged ICU admission. Drainage of effusion was significantly associated with a reduced ICU stay, P = 0.007 (see Tables 3 and 4).
Table 3.
Demographic, fluids and outcome variables in liver transplant patients grouped by ICU length of stay
| <5 days ICU stay (n = 78) | ≥5 days ICU stay (n = 80) | P value | |
|---|---|---|---|
| Male gender | 25 (32%) | 41 (51.2%) | 0.015 |
| HCC | 33 (42.3%) | 19 (23.1.7%) | 0.014 |
| Pretransplant MELD score | 17 ± 5.9 | 21.3 ± 8 | 0.001 |
| Volume of crystalloids received by 72 hours ml (IQR) | 1,675 (1,055) | 1,520 (1,066) | 0.034 |
| Volume of colloids received by ml (IQR) | |||
| 24 hours posttransplant | 1,247 (1,263) | 1,700 (1,188) | 0.046 |
| 48 hours posttransplant | 650 (713) | 950 (1095) | 0.015 |
| Undrained pleural effusion posttransplant | 28 (35.8%) | 50 (62.5%) | 0.001 |
| Vasopressors requirement | |||
| 48 hours posttransplant | 8 (10.3%) | 28 (35%) | 0.001 |
| 72 hours posttransplant | 2 (2.6%) | 10 (12.5%) | 0.031 |
| AKI | 17 (22%) | 40 (50%) | <0.001 |
| Early complications | 43 (55.1%) | 50 (62.5%) | 0.035 |
AKI, acute kidney injury; HCC, hepatocellular carcinoma; ICU, intensive care unit; IQR, interquartile range; MELD, model for end-stage liver disease.
Table 4.
Perioperative fluids in patients after liver transplant grouped by delayed weaning from mechanical ventilation
| <3 days mechanical ventilation (n = 104) | ≥3 days mechanical ventilation (n = 54) | P value | |
|---|---|---|---|
| Volume of blood products,* ml (IQR) | |||
| Operating room | 4,030 (2391) | 5,321 (4607) | 0.015 |
| 24 hours posttransplant | 920 (1551) | 3,028 (3893) | 0.017 |
| 48 hours posttransplant | 415 (470) | 827 (1194) | 0.048 |
| Volume of colloids, ml (IQR) | |||
| Operating room | 1,500 (1875) | 2,421 (850) | 0.032 |
| 24 hours posttransplant | 1,842 (1019) | 2,315 (1205) | <0.001 |
| 48 hours posttransplant | 625 (669) | 1,193 (933) | <0.001 |
| 72 hours posttransplant | 675 (881) | 700 (883) | 0.015 |
| Volume of chloride-liberal fluids, ml (IQR) | |||
| Operating room | 5,000 (7813) | 7,000 (8434) | 0.027 |
| 24 hours posttransplant | 3,397 (2868) | 3,725 (2473) | 0.020 |
| Fluid balance at 48 hours posttransplant, ml | 1,725 (1186) | 2,257 (2102) | 0.026 |
*Includes packed cells, fresh frozen plasma, platelets, cryoprecipitate. IQR, interquartile range.
Multivariate analysis
After adjusting for covariates, infusion of greater than 3,200 ml of chloride-liberal fluids (HR 6.25, 95% CI 2.69, 14.5, P <0.001) and preoperative MELD score (HR 1.08, 95% CI 1.02, 1.15, P = 0.004) remained significant predictors for AKI. Prolonged ICU stay was predicted by male gender, P = 0.014, vasopressors = 0.003 and the development of AKI, P = 0.013 (see Table 5).
Table 5.
Regression analysis for variables associated with acute kidney injury post-liver transplantation
| Hazard ratio | 95% CI | P value | |
|---|---|---|---|
| Univariate analysis | |||
| MELD score | 1.08 | 1.03,1013 | 0.001 |
| APACHE II score at admission to ICU | 1.08 | 1.03,1.15 | 0.018 |
| Colloids ≥1,500 ml received in OR | 1.97 | 1.01,3.8 | 0.046 |
| Chloride-liberal fluids ≥3,200 ml received within the first 24 hours posttransplant | 5.9 | 2.64,13.2 | 0.000 |
| Vasopressors requirement at 2 days posttransplant | 3.34 | 1.55,7.21 | 0.002 |
| Serum chloride level at day 2 | 1.09 | 1.01,1.18 | 0.015 |
| Multivariate analysis | |||
| Chloride-liberal fluids ≥3,200 ml received within the first 24 hours posttransplant | 6.25 | 2.69,14.5 | <0.001 |
| Preoperative MELD score | 1.08 | 1.02,1.15 | 0.004 |
APACHE II, acute physiology and chronic health evaluation II; CI, confidence interval; ICU, intensive care unit; MELD, model for end-stage liver disease; OR, operating room.
Discussion
In this observational study, we found that liver transplant recipients were more likely to develop AKI if they received larger volumes of chloride-liberal (hyperchloremic) fluids. This association was significant, after adjusting for baseline variables, for both 5% albumin in 0.9% saline and only 0.9% saline infusions. Patients who developed AKI had significantly higher serum chloride levels compared to transplant recipients that did not develop AKI.
‘Normal’ saline or 0.9% saline contains supraphysiological levels of chloride (154 mmol/L as compared to Hartmann’s solution, Ringer’s lactate or Plasma-Lyte 148, all of which contain chloride concentrations that are lower (94 to 111 mmol/L). Five percent albumin is available either as salt-poor or in sodium chloride (chloride concentration 128 mmol/L). Intravenous infusions of chloride-liberal fluids have been associated with hyperchloremia and metabolic acidosis when administered in large volumes [26].
Our results show a detrimental effect on renal function with use of chloride-liberal fluids in the immediate postoperative period (up to 48 hours). Support for our findings comes from animal studies that have demonstrated reductions in GFRs, renal arteriolar vasoconstriction [27], and human volunteer studies that have shown reduced renal cortical tissue perfusion, renal blood flow velocity after infusions of hyperchloremic solutions. [28]. In controlled trials, chloride-liberal fluids compared to chloride-poor fluids have been linked to longer time to micturition [21], lower urine output [29] and in a recent observational study of over 31,000 postoperative patients, 0.9% saline compared to ‘balanced’ crystalloids increased the risk of acute renal failure requiring dialysis [30]. Yunos et al., in a pre- and postintervention study on 1,530 critically ill patients found that a chloride-restrictive fluid strategy resulted in a significant reduction in AKI, need for RRT and increase in creatinine as compared to a control group given chloride-liberal fluids [23].
Possible explanations for this renal ‘toxicity’ of chloride-liberal fluids come from animal studies that have demonstrated renal vasoconstriction [22] and thromboxane release after chloride infusions [20]. Chloride infusions increase delivery to the macula densa that stimulates glomerulotubular feedback leading to afferent arteriole constriction, mesangial contraction and resultant decrease in GFR [31].
Patients in our study received both 5% albumin in saline and 20% albumin in saline. Though it is possible that the observed renal dysfunction resulted from hyperoncotic albumin, the data on 20% albumin is so far inconclusive. A recent cohort study on 1,000 patients found a higher risk of renal injury and failure with the use of hyperoncotic albumin (OR 5.99) [32], however, a contradictory result was reported from two meta-analyses that concluded no harmful effects of hyperoncotic resuscitation [33,34]. The SAFE study that compared albumin and saline found no difference in adverse outcomes [35].
Fluid overload leads to organ dysfunction due to interstitial edema and visceromegaly. The limited accommodative capacity of the encapsulated kidney causes increased interstitial hydrostatic pressures with reduced renal perfusion and filtration [36]. Additionally, a fluid overload state contributes to third spacing, ascitic fluid accumulation and abdominal compartment syndrome [37]. Cumulative fluid overload has been linked to poor outcomes in all groups (pediatric, septic, postoperative) of critically ill patients with prolonged days on mechanical ventilation, ICU stay and mortality [16,17,38-43]. Recovery of renal function in patients on RRT is also determined by overall fluid balance [17,38,42]. In our study, a cumulative positive fluid balance increased the duration of stay in ICU.
A limitation of our study is that the observational design does not establish a causal relationship of hyperchloremic fluid excess with the development of AKI in liver transplant recipients. These associations may be subject to bias from selection, confounding or random error. We attempted to control for confounders by using regression analysis. Another limitation is the external validity or generalizability of our results to other liver transplant recipients since we collected data only from a single institution.
Conclusions
In summary, large infusions of chloride-liberal fluids may predict a higher risk of AKI in liver transplant recipients. Our findings support the hypothesis that ‘routine’ intravenous fluids may not be routine and in themselves be associated with organ dysfunction. Our results can be used to build hypotheses for further controlled trials.
Key messages
Chloride-liberal fluids may cause renal dysfunction
Large volumes (>3,200 ml) of chloride-liberal fluids infused in the first 24 hours after liver transplantation were associated with a higher risk of AKI.
Acknowledgements
There was no special funding for the study. The design, collection, analysis and interpretation of data, plus writing and publication of the manuscript were done by the authors without participation or influence from any of the funding sources.
Abbreviations
- AKI
acute kidney injury
- APACHE II
acute physiologic and chronic health evaluation II
- BMI
body mass index
- CI
confidence interval
- GFR
glomerular filtration rate
- HR
hazard ratio
- ICU
intensive care unit
- IQR
interquartile range
- MELD
model for end-stage liver disease
- OR
odds ratio
- RIFLE
risk, injury, failure, loss, end-stage renal failure
- RRT
renal replacement therapy
- SD
standard deviation
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AN participated in the design of the study, collected the data, analyzed and interpreted the data, drafted the manuscript, and revised the manuscript critically for important intellectual content. NS conceived the study, participated in the design of the study, made the figures and table, analyzed and interpreted the data, drafted the manuscript, and revised the manuscript critically for important intellectual content. AH, MJ, HAS and BB participated in the design of the study, collected the data, and participated in the coordination of the study. YS and DB participated in the design and coordination of the study and participated in the critical review of the final manuscript. All authors have given final approval of the version to be published.
Contributor Information
Ashraf Nadeem, Email: ashmohnad@hotmail.com.
Nawal Salahuddin, Email: salahuddin.nawal@gmail.com.
Alyaa El Hazmi, Email: a.m.haz@live.com.
Mini Joseph, Email: mjoseph@kfshrc.edu.sa.
Balsam Bohlega, Email: bbohlega@kfshrc.edu.sa.
Hend Sallam, Email: sallam-h@hotmail.com.
Yasser Sheikh, Email: yelsheikh@kfshrc.edu.sa.
Dieter Broering, Email: dbroering@kfshrc.edu.sa.
References
- 1.Zhu M, Li Y, Xia Q, Wang S, Qiu Y, Che M, Dai H, Qian J, Ni Z, Axelsson J, Yan Y. Strong impact of acute kidney injury on survival after liver transplantation. Transplant Proc. 2010;42:3634–3638. doi: 10.1016/j.transproceed.2010.08.059. [DOI] [PubMed] [Google Scholar]
- 2.Karapanagiotou A, Kydona C, Dimitriadis C, Sgourou K, Giasnetsova T, Fouzas I, Imvrios G, Gritsi-Gerogianni N. Acute kidney injury after orthotopic liver transplantation. Transplant Proc. 2012;44:2727–2729. doi: 10.1016/j.transproceed.2012.09.096. [DOI] [PubMed] [Google Scholar]
- 3.O'Riordan A, Wong V, McQuillan R, McCormick PA, Hegarty JE, Watson AJ. Acute renal disease, as defined by the RIFLE criteria, post-liver transplantation. Am J Transplant. 2007;7:168–176. doi: 10.1111/j.1600-6143.2006.01602.x. [DOI] [PubMed] [Google Scholar]
- 4.Barri YM, Sanchez EQ, Jennings LW, Melton LB, Hays S, Levy MF, Klintmalm GB. Acute kidney injury following liver transplantation: definition and outcome. Liver Transpl. 2009;15:475–483. doi: 10.1002/lt.21682. [DOI] [PubMed] [Google Scholar]
- 5.Watt KD, Pedersen RA, Kremers WK, Heimbach JK, Charlton MR. Evolution of causes and risk factors for mortality post-liver transplant: results of the NIDDK long-term follow-up study. Am J Transplant. 2010;10:1420–1427. doi: 10.1111/j.1600-6143.2010.03126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei Y, Zhang L, Lin H, Li J, Li B, Yan L, Wen T, Zeng Y, Lu S. Factors related to post-liver transplantation acute renal failure. Transplant Proc. 2006;38:2982–2984. doi: 10.1016/j.transproceed.2006.08.156. [DOI] [PubMed] [Google Scholar]
- 7.Pawarode A, Fine DM, Thuluvath PJ. Independent risk factors and natural history of renal dysfunction in liver transplant recipients. Liver Transpl. 2003;9:741–747. doi: 10.1053/jlts.2003.50113. [DOI] [PubMed] [Google Scholar]
- 8.Chen J, Singhapricha T, Hu KQ, Hong JC, Steadman RH, Busuttil RW, Xia VW. Postliver transplant acute renal injury and failure by the RIFLE criteria in patients with normal pretransplant serum creatinine concentrations: a matched study. Transplantation. 2011;91:348–353. doi: 10.1097/TP.0b013e31820437da. [DOI] [PubMed] [Google Scholar]
- 9.Sanchez EQ, Gonwa TA, Levy MF, Goldstein RM, Mai ML, Hays SR, Melton LB, Saracino G, Klintmalm GB. Preoperative and perioperative predictors of the need for renal replacement therapy after orthotopic liver transplantation. Transplantation. 2004;78:1048–1054. doi: 10.1097/01.TP.0000137176.95730.5B. [DOI] [PubMed] [Google Scholar]
- 10.Bilbao I, Charco R, Balsells J, Lazaro JL, Hidalgo E, Llopart L, Murio E, Margarit C. Risk factors for acute renal failure requiring dialysis after liver transplantation. Clin Transpl. 1998;12:123–129. [PubMed] [Google Scholar]
- 11.Lima EQ, Zanetta DM, Castro I, Massarollo PC, Mies S, Machado MM, Yu L. Risk factors for development of acute renal failure after liver transplantation. Ren Fail. 2003;25:553–560. doi: 10.1081/JDI-120022546. [DOI] [PubMed] [Google Scholar]
- 12.Lebron Gallardo M, Herrera Gutierrez ME, Seller Perez G, Curiel Balsera E, Fernandez Ortega JF, Quesada Garcia G. Risk factors for renal dysfunction in the postoperative course of liver transplant. Liver Transpl. 2004;10:1379–1385. doi: 10.1002/lt.20215. [DOI] [PubMed] [Google Scholar]
- 13.Cabezuelo JB, Ramirez P, Rios A, Acosta F, Torres D, Sansano T, Pons JA, Bru M, Montoya M, Bueno FS, Robles R, Parrilla P. Risk factors of acute renal failure after liver transplantation. Kidney Int. 2006;69:1073–1080. doi: 10.1038/sj.ki.5000216. [DOI] [PubMed] [Google Scholar]
- 14.Herrler T, Tischer A, Meyer A, Feiler S, Guba M, Nowak S, Rentsch M, Bartenstein P, Hacker M, Jauch KW. The intrinsic renal compartment syndrome: new perspectives in kidney transplantation. Transplantation. 2010;89:40–46. doi: 10.1097/TP.0b013e3181c40aba. [DOI] [PubMed] [Google Scholar]
- 15.Alsous F, Khamiees M, DeGirolamo A, Amoateng-Adjepong Y, Manthous CA. Negative fluid balance predicts survival in patients with septic shock: a retrospective pilot study. Chest. 2000;117:1749–1754. doi: 10.1378/chest.117.6.1749. [DOI] [PubMed] [Google Scholar]
- 16.Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care. 2008;12:R74. doi: 10.1186/cc6916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422–427. doi: 10.1038/ki.2009.159. [DOI] [PubMed] [Google Scholar]
- 18.Bagshaw SM, Brophy PD, Cruz D, Ronco C. Fluid balance as a biomarker: impact of fluid overload on outcome in critically ill patients with acute kidney injury. Crit Care. 2008;12:169. doi: 10.1186/cc6948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reydellet L, Blasco V, Mercier MF, Antonini F, Nafati C, Harti-Souab K, Leone M, Albanese J. Impact of a goal-directed therapy protocol on postoperative fluid balance in patients undergoing liver transplantation: A retrospective study. Ann Fr Anesth Reanim. 2014;33:e47–e54. doi: 10.1016/j.annfar.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 20.Bullivant EM, Wilcox CS, Welch WJ. Intrarenal vasoconstriction during hyperchloremia: role of thromboxane. Am J Physiol. 1989;256:F152–F157. doi: 10.1152/ajprenal.1989.256.1.F152. [DOI] [PubMed] [Google Scholar]
- 21.Williams EL, Hildebrand KL, McCormick SA, Bedel MJ. The effect of intravenous lactated Ringer's solution versus 0.9% sodium chloride solution on serum osmolality in human volunteers. Anesth Analg. 1999;88:999–1003. doi: 10.1097/00000539-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Wilcox CS. Regulation of renal blood flow by plasma chloride. J Clin Invest. 1983;71:726–735. doi: 10.1172/JCI110820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012;308:1566–1572. doi: 10.1001/jama.2012.13356. [DOI] [PubMed] [Google Scholar]
- 24.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wakim KG. “Normal” 0.9 per cent salt solution is neither “normal” nor physiological. JAMA. 1970;214:1710. doi: 10.1001/jama.1970.03180090074027. [DOI] [PubMed] [Google Scholar]
- 27.Wan L, Bellomo R, May CN. Bolus hypertonic or normal saline resuscitation in gram-negative sepsis: systemic and regional haemodynamic effects in sheep. Crit Care Resusc. 2011;13:262–270. [PubMed] [Google Scholar]
- 28.Chowdhury AH, Cox EF, Francis ST, Lobo DN. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and plasma-lyte® 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg. 2012;256:18–24. doi: 10.1097/SLA.0b013e318256be72. [DOI] [PubMed] [Google Scholar]
- 29.Wilkes NJ, Woolf R, Mutch M, Mallett SV, Peachey T, Stephens R, Mythen MG. The effects of balanced versus saline-based hetastarch and crystalloid solutions on acid–base and electrolyte status and gastric mucosal perfusion in elderly surgical patients. Anesth Analg. 2001;93:811–816. doi: 10.1097/00000539-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Shaw AD, Bagshaw SM, Goldstein SL, Scherer LA, Duan M, Schermer CR, Kellum JA. Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann Surg. 2012;255:821–829. doi: 10.1097/SLA.0b013e31825074f5. [DOI] [PubMed] [Google Scholar]
- 31.Salomonsson M, Gonzalez E, Kornfeld M, Persson AE. The cytosolic chloride concentration in macula densa and cortical thick ascending limb cells. Acta Physiol Scand. 1993;147:305–313. doi: 10.1111/j.1748-1716.1993.tb09503.x. [DOI] [PubMed] [Google Scholar]
- 32.Schortgen F, Girou E, Deye N, Brochard L. The risk associated with hyperoncotic colloids in patients with shock. Intensive Care Med. 2008;34:2157–2168. doi: 10.1007/s00134-008-1225-2. [DOI] [PubMed] [Google Scholar]
- 33.Wiedermann CJ, Dunzendorfer S, Gaioni LU, Zaraca F, Joannidis M. Hyperoncotic colloids and acute kidney injury: a meta-analysis of randomized trials. Crit Care. 2010;14:R191. doi: 10.1186/cc9308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jacob M, Chappell D, Conzen P, Wilkes MM, Becker BF, Rehm M. Small-volume resuscitation with hyperoncotic albumin: a systematic review of randomized clinical trials. Crit Care. 2008;12:R34. doi: 10.1186/cc6812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247–2256. doi: 10.1056/NEJMoa040232. [DOI] [PubMed] [Google Scholar]
- 36.Stone HH, Fulenwider JT. Renal decapsulation in the prevention of post-ischemic oliguria. Ann Surg. 1977;186:343–355. doi: 10.1097/00000658-197709000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vidal MG, Ruiz Weisser J, Gonzalez F, Toro MA, Loudet C, Balasini C, Canales H, Reina R, Estenssoro E. Incidence and clinical effects of intra-abdominal hypertension in critically ill patients. Crit Care Med. 2008;36:1823–1831. doi: 10.1097/CCM.0b013e31817c7a4d. [DOI] [PubMed] [Google Scholar]
- 38.Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, Lee J, Lo S, McArthur C, McGuiness S, Norton R, Myburgh J, Scheinkestel C, Su S. An observational study fluid balance and patient outcomes in the Randomized Evaluation of Normal vs Augmented Level of Replacement Therapy trial. Crit Care Med. 2012;40:1753–1760. doi: 10.1097/CCM.0b013e318255d9a0. [DOI] [PubMed] [Google Scholar]
- 39.Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39:259–265. doi: 10.1097/CCM.0b013e3181feeb15. [DOI] [PubMed] [Google Scholar]
- 40.Brandstrup B, Tonnesen H, Beier-Holgersen R, Hjortso E, Ording H, Lindorff-Larsen K, Rasmussen MS, Lanng C, Wallin L, Iversen LH, Gramkow CS, Okholm M, Blemmer T, Svendsen PE, Rottensten HH, Thage B, Riis J, Jeppesen IS, Teilum D, Christensen AM, Graungaard B, Pott F. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641–648. doi: 10.1097/01.sla.0000094387.50865.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gillespie RS, Seidel K, Symons JM. Effect of fluid overload and dose of replacement fluid on survival in hemofiltration. Pediatr Nephrol. 2004;19:1394–1399. doi: 10.1007/s00467-004-1655-1. [DOI] [PubMed] [Google Scholar]
- 42.Heung M, Wolfgram DF, Kommareddi M, Hu Y, Song PX, Ojo AO. Fluid overload at initiation of renal replacement therapy is associated with lack of renal recovery in patients with acute kidney injury. Nephrol Dial Transplant. 2012;27:956–961. doi: 10.1093/ndt/gfr470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF, Jr, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]


