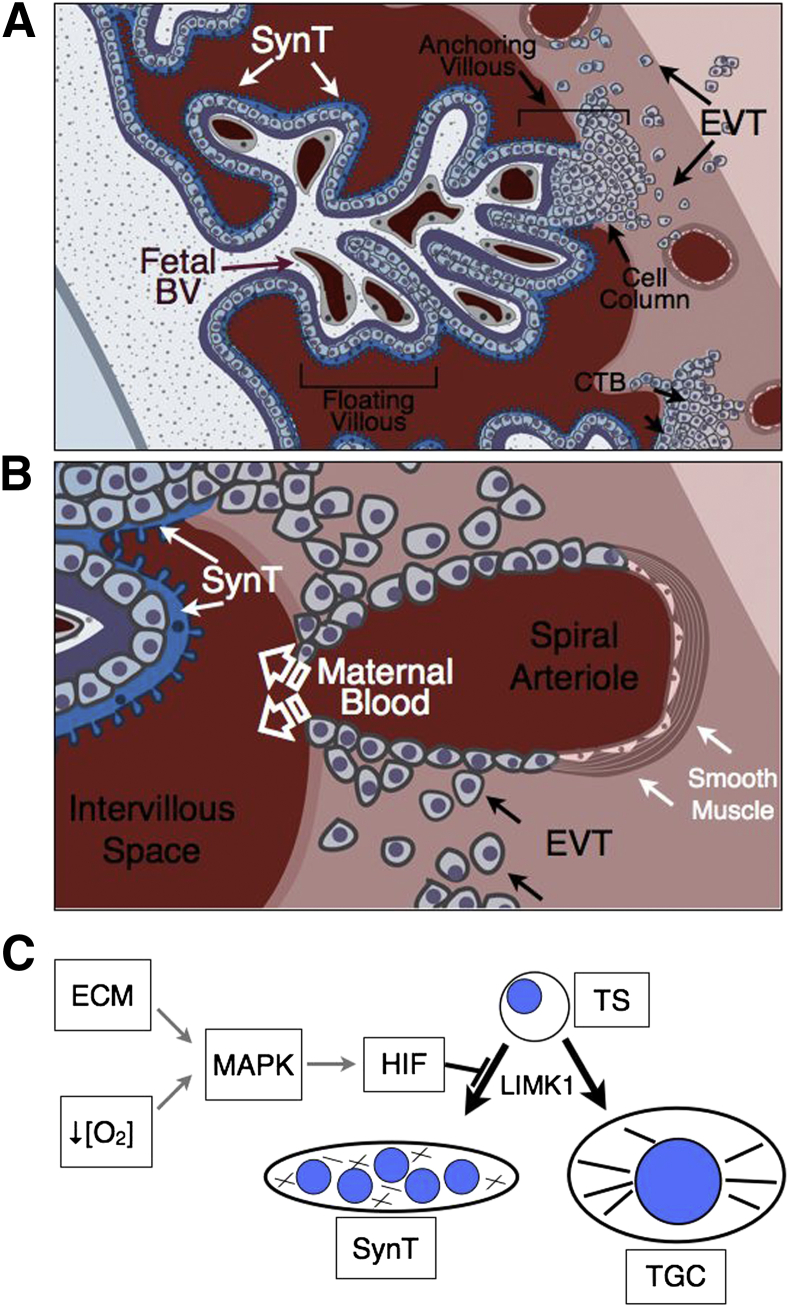
Figure 1.
A and B: Schematic representation of the human maternal–vascular interface created by the placenta as a function of trophoblast invasion. A: In the human placenta, the primary anatomical subunit is composed of the chorionic villous, which can either be floating or anchoring. Floating villi are composed of highly branched finger-like projections that are surrounded by a layer of multinucleated SynT that perform the transport functions of the placenta. B: Occasionally, the tips of villi attach to the uterus (anchoring villous), triggering the expansion of a population of cytotrophoblasts within cell columns that gives rise to invasive EVTs. Invading EVTs migrate through uterine tissues in search of uterine arterioles that are remodeled by them. During this process, EVTs breach the spiral arterioles, triggering apoptotic death of existing endothelial and smooth muscle cells, and line the spiral arterioles while transdifferentiating into an endothelialized trophoblast cell type, expressing many cell surface markers characteristic of endothelial cells. This allows for blood flow from the arterioles into the intervillous space. C: Model depicting induction of HIF activity in mouse trophoblast stem (TS) cells by ECM composition or oxygen tension ([O2]). HIF induction blocks TS cell differentiation along the SynT lineage and promotes invasive trophoblast giant cell (TGC) differentiation via LIMK1 expression and subsequent promotion of cytoskeletal integrity. BV, blood vessel.