Abstract
Background/Aims
Percutaneous endoscopic gastrostomy (PEG) is a method of providing enteral nutrition using endoscopy. The PEG techniques differ according to the insertion method, and include the pull type, push type, and introducer type. The aim of this study was to compare the clinical outcomes associated with the pull-type and introducer-type PEG insertion techniques, which included the adverse events, at our tertiary care center in Korea.
Methods
We retrospectively reviewed 141 cases that had undergone PEG insertion at our center from January 2009 to June 2012. The indications for PEG insertion and the acute and chronic complications caused by each type of PEG insertion were analyzed.
Results
The indications for PEG insertion in our cohort included neurologic disease (58.7%), malignancy (21.7%), and other indications (19.6%). Successful PEG insertions were performed on 136 cases (96.5%), and there were no PEG-associated deaths. Bleeding was the most frequent acute complication (12.8%), and wound problems were the most frequent chronic complications (8.8%). There were no statistically significant differences between the pull-type and introducer-type PEG insertion techniques in relation to complication rates in our study population.
Conclusions
PEG insertion is considered a safe procedure. The pull-type and introducer-type PEG insertion techniques produce comparable outcomes, and physicians may choose either of these approaches according to the circumstances.
Keywords: Percutaneous endoscopic gastrostomy, Pull type, Introducer type, Complication, Indication for PEG
INTRODUCTION
Percutaneous endoscopic gastrostomy (PEG) is a technique that creates a route for providing enteral nutrition using an endoscopic approach.1,2 PEG is a safe and effective procedure for patients who require enteral tube feeding for longer than 1 month.3,4 It was introduced in 1980 as an alternative operative gastrostomy procedure.5 More patients require PEG insertion as a feeding intervention, because life expectancies and the incidence of senile diseases have increased in recent times.
There are several PEG insertion techniques that include the pull- (Ponsky-Gauderer), push- (Sacks-Vine), and introducer- (Russell) methods.6,7 At the Asan Medical Center, the pull-type and introducer-type PEG insertion techniques are employed. The pull-type PEG insertion technique involves placing the gastrostomy tube through the mouth and oral cavity, while the introducer-type PEG insertion technique involves placing the gastrostomy tube via a direct puncture of the abdomen without passing it through the oral cavity. Endoscopic insertion is required twice for the pull-type PEG insertion technique.
In this study, we investigated whether complications arising from PEG insertion differed according to the insertion techniques used. We also aimed to assess whether the introducer-type PEG insertion technique, which has been adopted more recently by our hospital, might replace the pull-type PEG insertion technique.
MATERIALS AND METHODS
Study population
Our study cohort comprised patients who were older than 18 years and had undergone PEG insertion for the first time between January 1, 2009 and June 30, 2012 at Asan Medical Center, a tertiary medical center in Seoul, Korea. A population of 138 patients satisfied these criteria and the cohort comprised 141 cases who had undergone PEG insertion. We analyzed the patients' records and collected information relating to age, sex, body mass index, the insertion point, the indication for the PEG procedure, and any comorbidities, including diabetes mellitus, hypertension, and atrial fibrillation. We also reviewed acute complications such as bleeding, wound infections, peritonitis, aspiration pneumonia, and ileus, and chronic complications including wound problems, leakages, tube obstructions, spontaneous removals, and buried bumper syndrome that resulted from PEG insertion. The Institutional Review Board of the Asan Medical Center approved our study protocol.
Outcomes
The primary study outcomes were the different complications associated with the PEG insertion techniques and their frequencies. The secondary study outcomes we evaluated were the complication rates associated with each PEG insertion technique. We also evaluated the success rates of the PEG insertion techniques and the frequencies of severe complications that required intensive care unit interventions or significantly altered the vital signs and resulted in shock.
PEG insertion technique
The pull-type and introducer-type PEG insertion techniques were performed at our hospital and were evaluated in this study. A 20-Fr or a 22 Fr-PEG tube (US Endoscopy, Mentor, OH, US) was used for the pull-type insertion technique and a 15-Fr PEG tube (Create Medic Co., Ltd., Yokohama, Japan) was used for the introducer-type insertion technique. Pull-type PEG insertions only were performed at our center until January 2010, after which the introducer-type PEG insertion technique was additionally adopted. However, the pull type was still predominantly used until October 2011, after which about 93% of the PEG procedures at our hospital. Between January 2010 and October 2011 when the pull type and the introducer type PEG insertion were used together, there were no limitations in both types of PEG insertions. The operator decided which technique to use according to his preference. After October 2011, the clinicians at our center agreed to use the introducer-type PEG insertion technique only, and the pull-type PEG insertion technique was conducted when patients or guardians specifically requested this type of PEG insertion. They wanted the pull type PEG since the length of the gastrostomy tube was longer compared to the introducer type PEG.
PEG insertion using the pull-type technique requires two endoscopic insertions and the placement of the gastrostomy tube through the mouth and esophagus. This method is aided by the insertion of a transilluminated endoscope that enables the clinicians to decide where to site the PEG tube. The guide-wire is then punctured through this site. Using biopsy forceps, the guidewire is removed through the oral cavity and the gastrostomy tube is connected. The other end of the guidewire is then retracted from the abdominal wall to position the gastrostomy tube. To confirm whether the tube is correctly positioned, the endoscope is inserted again.
PEG insertion using the introducer-type technique uses a trochar, and the gastrostomy tube is placed directly from the exterior through the abdominal wall and it does not pass through the gastrointestinal tract. At our center, all introducer-type PEG insertions are performed using an endoscope to visualize the stomach cavity. This approach differs from the pull-type insertion technique, because the tube is inserted directly into the abdominal wall without passing through the oral cavity and esophagus. For fixation of the tube with this method, saline is used for ballooning, whereas a mushroom type tube is used in the pull type technique. Given the differences between the insertion techniques and the tube shapes, we aimed to determine whether these procedures were associated with different complication rates.
In our study cohort, the patients were administered routine injections of cefazolin (2 g), 30 minutes before PEG insertion. For patients who were receiving concomitant antibiotics, these antibiotics were not changed unless they did not cover gram-positive cocci.
Of the 132 cases within our study cohort for whom adverse events were analyzed, medical fellows performed most of the PEG insertion procedures (80.2%). Twenty-six of the PEG insertion procedures (19.7%) were performed by a single experienced physician and a coauthor of this paper (JHL). Experienced physician performed the procedure in cases where difficulties were anticipated following PEG such as the postoperative status, bleeding issues or procedure failure.
Definitions of complications
We categorized complications as being either acute or chronic, based on whether they occurred within or after 7 days of the PEG insertion procedure, respectively. Patients were excluded from the study cohort if they removed their gastrostomy tubes themselves.
Bleeding, peritonitis, wound infections, aspiration, ileus, and procedure-related deaths were classified as acute complications. With respect to chronic complications, we reviewed delayed wound infections, the presence of granulation tissue, leakages at the anastomoses sites, tube obstructions, sponta neous removals, and buried bumper syndrome, which is a syndrome that is caused by long-term pressure and results in the bolster becoming buried in the gastric wall.
Among the acute complications associated with PEG insertion, bleeding was categorized as being major or minor. When bleeding was successfully treated using simple procedures or supportive care, it was categorized as minor. Major bleeding was defined as unstable vital signs or a reduction in the hemoglobin level that was greater than 2 mg/dL.
Aspiration was defined as vomiting after tube feeding that was accompanied by an increased oxygen requirement or the detection of findings that were indicative of aspiration pneumonia on a chest radiograph during the 7 days that followed the PEG insertion procedure. Ileus was defined as abdominal pain after tube feeding, a reduction in bowel sounds, findings indicative of ileus on abdominal radiographs, and problems arising after tube feeding, including the regurgitation of food materials or leakage through the anastomosis site.
The presence of granulation tissue or wound infections was considered a chronic complication if the medical records indicated the occurrence of these adverse events. Most patients who undergo PEG insertions at our center receive home health care subsequently. Nurses who are specialized in wound care and sampling blood regularly visit these patients and update their medical charts, and in some circumstances, these nurses administer antibiotics to the patients after consultation with a doctor. We reviewed the patients' home health care charts to precisely determine the incidence rates of granulation tissue and wound infection.
Statistical analyses
Analysis of the data from the patients' medical records was performed using IBM SPSS version 20 (IBM Co., Armonk, NY, USA). To compare complications, Fisher exact test or the chi-square test were used. A p-value of less than 0.05 was considered statistically significant.
RESULTS
The clinical and laboratory characteristics of the patients are shown in Table 1. The mean age of the patients in the study cohort was 62.7 years, and 65.2% of the cohort comprised men. The laboratory data from these subjects, including white blood cell counts, hemoglobin levels, platelet counts, albumin levels, C-reactive protein levels, and prothrombin times, were evaluated (Table 1). The differences between the pull-type and the introducer-type PEG insertion techniques in relation to the patients' characteristics are presented in Table 1. The albumin levels differed significantly between the patients who underwent pull-type PEG insertions and those who underwent introducer-type PEG insertions (3.0 g/dL vs. 3.4 g/dL; p=0.001).
Table 1.
Clinical and Laboratory Characteristics of Patients Received Percutaneous Endoscopic Gastrostomy Insertion
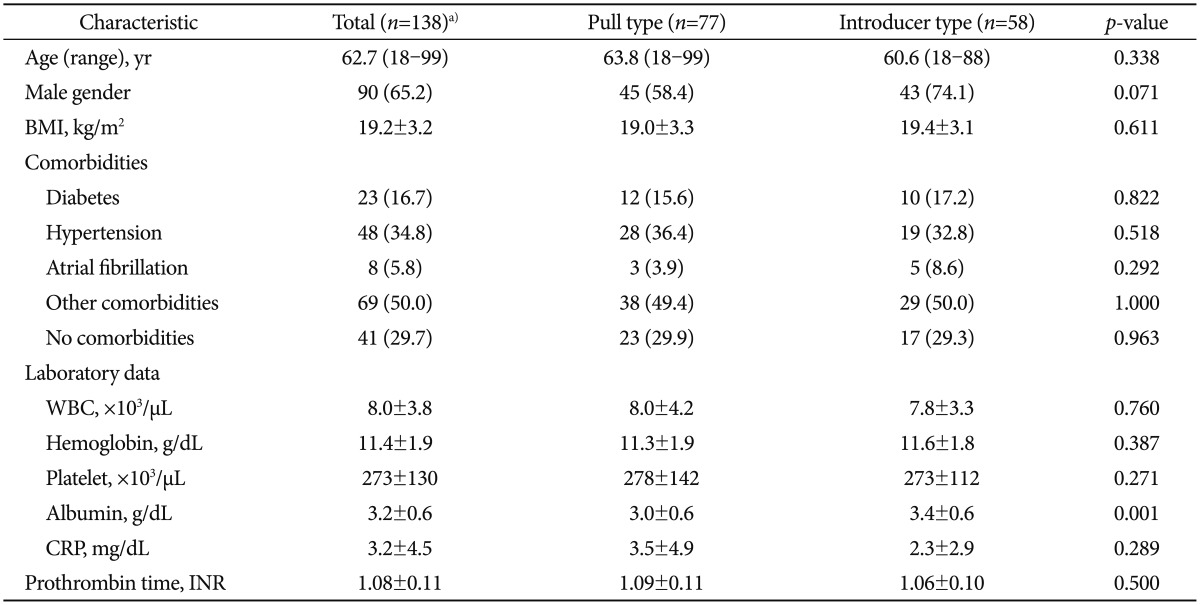
Values are presented as number (%) or mean±SD.
BMI, body mass index; WBC, white blood cell; CRP, C-reactive protein; INR, international normalized ratio.
a)Total 138 subjects underwent percutaneous endoscopic gastrostomy (PEG) insertion procedure. Three of them failed to have PEG insertion. Seventy seven among the remaining 135 subjects received pull type PEG insertion, and 58 subjects received introducer type PEG insertion.
The 138 patients in our cohort underwent 141 procedures to insert PEGs. One patient underwent two PEG insertions because he removed the PEG tube himself 4 days after the first procedure. Two other patients experienced insertion failures when the PEG tubes were initially inserted, because of increases in the pneumoperitoneum after puncture and difficulties finding an appropriate puncture site. Subsequent PEG insertions performed by a more experienced physician were successful in both of these patients, one of whom underwent the pull-type insertion procedure and the other underwent the introducer-type insertion procedure. Among the 141 PEG insertions performed on this study cohort, there were five failures, which amounted to a 96.5% success rate. Pull-type PEG insertions were conducted in 77 subjects and introducer-type PEG insertions were undertaken in 58 subjects.
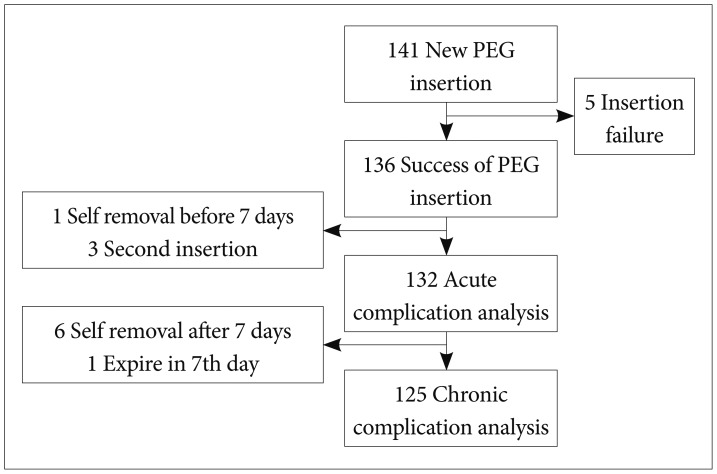
Further analysis of the study cohort is provided in Fig. 1. Of the 136 successful PEG procedures in our study population. One patient received introducer type PEG insertion twice due to self-removal in 7 days, and these two cases were excluded. In addition, the first PEG insertions failed and the second PEG insertions were successful in two patients who were excluded from our evaluations of acute complications. One patient who died because of the aggravation of an underlying disease and six patients who removed their gastrostomy tubes themselves after the they had been in place for 7 days, were excluded from the evaluation of chronic complications. Hence, 125 cases were analyzed in relation to chronic complications.
Fig. 1.
Number of percutaneous endoscopic gastrostomy (PEG) insertion cases assessed for complication in the analysis
The mean follow-up period for these patients was 216 days (range, 6 to 773), and 55% of the patients had a follow-up period that was less than 6 months. The end of the follow-up period was defined as the last date on a patient's outpatient medical records, the last discharge date following a patient's last admission, or the date of death if the patient died at our center.
Indications for PEG insertions
The indications for PEG insertion were divided into neurologic disease, malignancy, and "other" indications, and 58.7%, 21.7%, and 19.6% of the patients, respectively, were assigned to these categories (Table 2).
Table 2.
Indications for Percutaneous Endoscopic Gastrostomy Insertion (n=138)
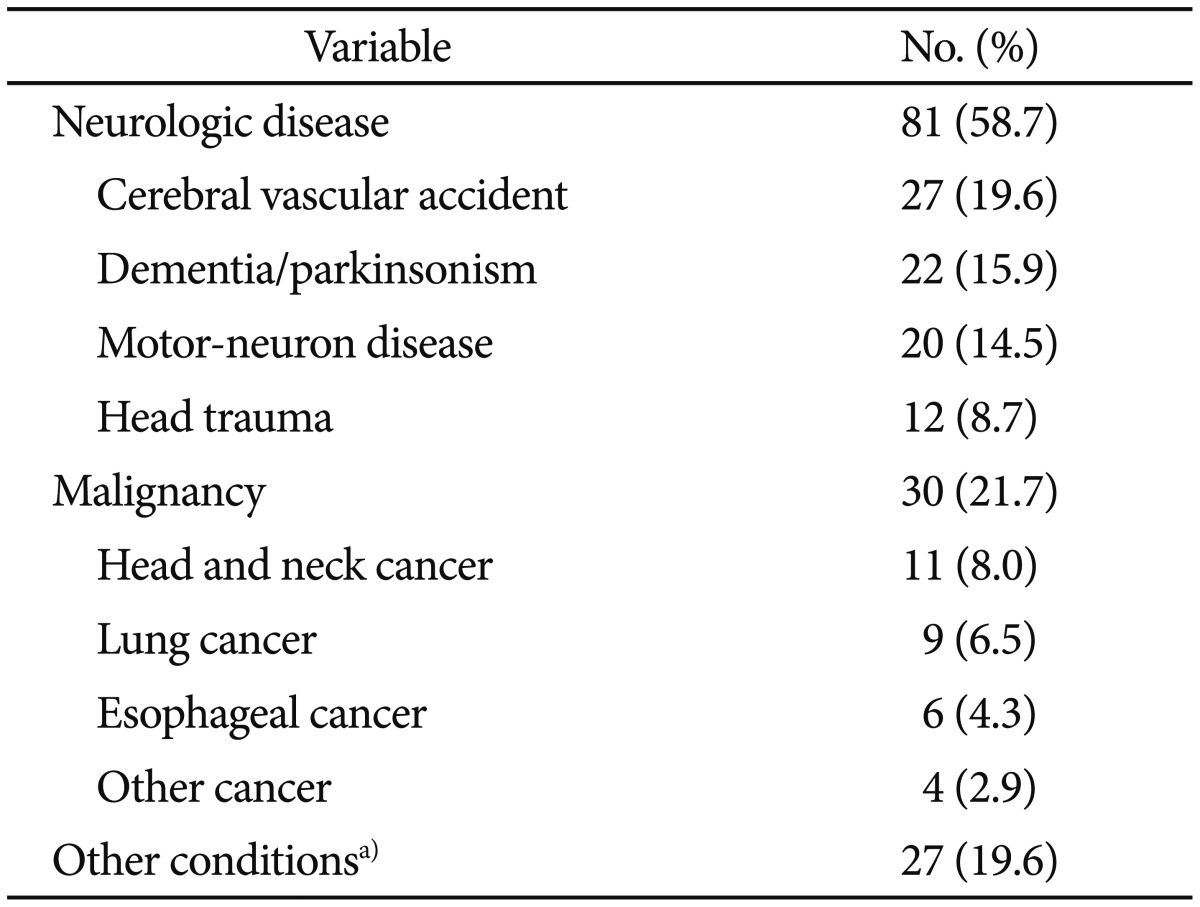
a)Esophago-pleural fistula, nasogastric tube injury to the esophagus, poor general condition, and mental change due to hepatic encephalopathy, cardio pulmonary cerebral resuscitation survivor.
Neurologic disease was the most common indication for PEG insertion (58.7%), and within the neurologic disease category a cerebrovascular accident was the most frequent indication for PEG insertion (27 cases, 19.6%). Malignancy was recorded as the indication for PEG insertion for 30 cases (21.7%), and head and neck cancer was recorded for 11 cases (8.0%). The "other" indications category incorporated 27 cases (19.6%) and it was comprised of a variety of conditions, including esophagopleural fistulae or nasogastric tube injuries to the esophagus, poor general health, psychological changes resulting from hepatic encephalopathy, and cardiopulmonary resuscitation survival.
PEG insertion failures
PEG insertions failed in five cases in our study cohort. One patient could not hold the mouthpiece in his mouth to enable the insertion of the endoscope, and he later underwent a radiology-guided percutaneous gastrostomy. It was not possible to locate suitable puncture sites in three patients. One of these three patients was given a pull-type PEG insertion. This patient had previously received subtotal gastrectomy with Billroth I procedure. Introducer-type PEG insertions were attempted in the other two patients, but anatomic variations led to failures to puncture the stomach cavities of these patients. Subsequently, a more experienced physician performed the introducer-type PEG insertion procedure in one of these patients, which was successful. An introducer-type PEG insertion procedure had to be stopped in the remaining patient because of pneumoperitoneum after the puncture, and an introducer-type PEG insertion was completed successfully the next day.
Complications associated with PEG insertions
We analyzed and compared the two PEG techniques in relation to their complication rates (Tables 3, 4). Seventy-one cases (56.8%) had no recorded complications, and no significant differences were evident between the PEG insertion types with respect to complications. There were no procedure-related deaths in our study population. Life-threatening complications that led to shock or transfer to the intensive care unit occurred in three cases (2.3%), which included major bleeding and peritonitis.
Table 3.
Acute Complications by Percutaneous Endoscopic Gastrostomy Insertion Types
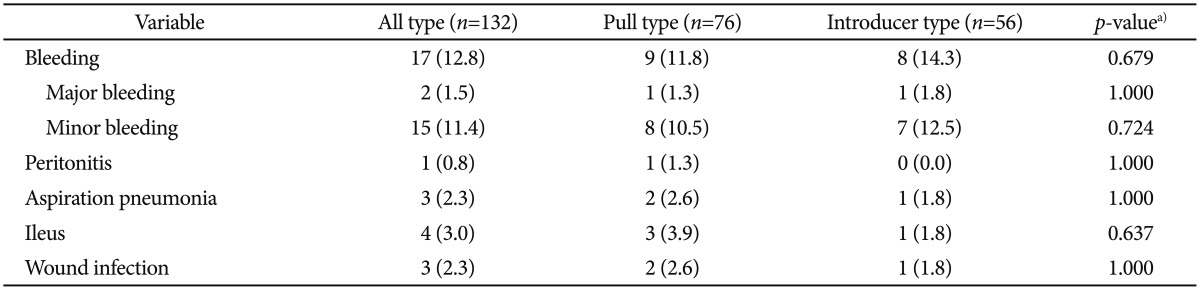
a)p-value was calculated by chi-square test and Fisher's exact test.
Table 4.
Chronic Complications by Percutaneous Endoscopic Gastrostomy Insertion Types
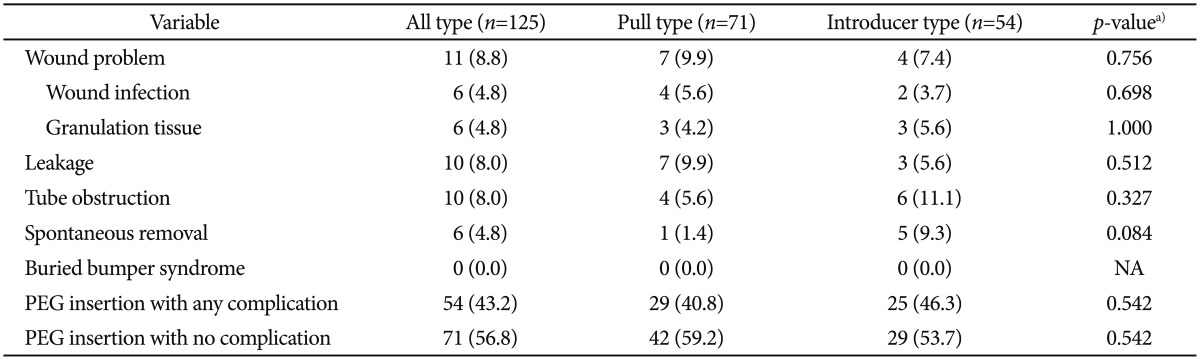
PEG, percutaneous endoscopic gastrostomy; NA, not available.
a)p-value was calculated by chi-square test and Fisher's exact test.
The most common acute complication was bleeding that occurred in 17 cases (12.8%). Most of these cases experienced minor bleeding; however, two cases experienced life-threatening bleeding complications, and of these, one patient had undergone a pull-type PEG insertion and the other had undergone an introducer-type PEG insertion. One of these patients experienced hemoperitoneum that required admission to the intensive care unit and embolization of the left gastric artery. The other case of major bleeding involved a patient whose PEG insertion site bled into the gastric lumen. An experienced physician had performed the endoscopic insertion in this case, but he could not find the focus of the bleeding. The patient later recovered with supportive care. Acute wound infections occurred in three cases (2.3%), and no significant difference was found between the pull-type and the introducer-type PEG insertions with respect to the acute wound infection rate.
Among the chronic complications that we assessed, wound problems were the most common with 11 cases (8.8%) affected. Wound problems were categorized into wound infections and the presence of granulation. Leakage tended to be more closely associated with the pull-type PEG insertion technique, with seven cases (9.9%) who had undergone pull-type PEG insertions and three cases (5.6%) who had undergone introducer-type PEG insertions affected, but this difference was not statistically significant. On the other hand, in comparing the pull type and introducer type PEG insertion subjects, tube obstruction occurred in four cases (5.6%) and six cases (11.1%), respectively, and spontaneous tube removal occurred in one case (1.4%) and five cases (9.3%), respectively, showing that they were more common following introducer type PEG procedure. However, this was also not statistically significant. In our current analysis also, no buried bumper syndrome nor PEG insertion related deaths were recorded.
During the follow-up period, 55 patients in our cohort died because of underlying diseases and other causes that included infection. The 30-day mortality rate was 6.5%. However, no procedure-related deaths were recorded on the patients' charts.
DISCUSSION
PEG insertion is a common intervention for a variety of medical conditions. Most of the cases who underwent PEG insertions in our study had underlying neurological diseases (58.7%), and malignancy (21.7%) was the second most common indication for PEG insertion in our cohort. These proportions may have arisen because this study was implemented in a tertiary hospital. PEG insertion is an established and a relatively safe procedure for feeding patients, but it is also associated with several potential complications.4
Low serum albumin levels might be a risk factor associated with complications or mortality arising from PEG insertions8,9,10 and most studies have reported an increased risk of complications when albumin levels decline to less than 3.0 g/dL. In our study, the baseline albumin levels differed between the pull-type and the introducer-type PEG insertion groups (3.0 g/dL vs. 3.4 g/dL; p=0.001). It is unclear; however, whether the albumin levels in patients who underwent pull-type PEG insertions had any influence on the frequency of complications.
When a puncture is performed during the PEG insertion procedure, there is a risk of bleeding. Bleeding to the peritoneum may occur, but a diagnosis of hemoperitoneum may be masked for a period of time. If there are no hemodynamic changes, it is difficult to detect bleeding using a routine test such as a simple abdominal X-ray. In a Turkish study involving 81 PEG insertion cases, there was one case (1%) of a bleeding-related death, which is comparable with the major bleeding rate of 1.5% in the present study.11 The most commonly reported reason for bleeding after PEG insertion is ulceration of the gastric mucosa that is inferior to the internal bumper.12 Although uncommon, other causes of gastrointestinal bleeding after PEG insertion include esophageal trauma, gastric erosions, and unrelated peptic ulcer disease.12,13 Overall, the bleeding incidence in the current study cohort was 12.8%, which is higher than that described in earlier reports (2.5% to 2.8%).13,14,15 However, no interventions were required for most of the cases of bleeding following PEG insertions because bleeding is a natural consequence of puncture; therefore, it is possible that some of the bleeding events in the patients who had undergone PEG insertions that were categorized as complications were not genuine complications. The incidence of major bleeding was low (1.5%) in the current study cohort. An earlier large-scale study undertaken by Richter-Schrag et al.16 that involved 1,041 patients, reported a bleeding incidence of 0.5%. In that study, bleeding was defined as the occurrence of hematemesis, passing blood anally, or passing blood via the stoma or the PEG tube.
Wound infections typically occur in 5% to 36% of patients when the pull-type insertion method is used, despite the use of prophylactic antibiotics.17,18,19,20,21,22 In relation to the pull-type PEG insertion method, it has been suggested that the normal flora of the oral cavity is moved to the puncture site when the gastrostomy tube passes through the oral cavity.23 Consequently, the pull-type PEG insertion technique is considered to carry a higher risk of wound infection. In our study cohort, however, there were only three recorded cases (2.3%) of wound infections during the acute phase after PEG insertion, and no significant differences were found between the pull-type and the introducer-type PEG insertion techniques in this regard (2.6% vs. 1.8%).
Overall, the problems that were associated with the wounds related to the chronic management of the PEG tubes. The most common long-term complication in our study population related to chronic wound problems, and these had frequencies of 9.9% in the cases that had undergone pull-type PEG insertions, 7.4% in the cases that had undergone introducer-type PEG insertions, and 8.8% overall.
In our analysis, leakages seemed to be higher in the pull-type PEG insertion group and tube obstruction tended to be more common in the introducer-type PEG insertion group, but neither finding was statistically significant. The initial tube diameter used was greater in the pull-type insertion technique (20 or 22 Fr) compared with the introducer-type insertion technique (15 Fr), and the difference in the sizes may have been associated with the leakages and tube obstructions. According to The European Society for Clinical Nutrition and Metabolism guidelines, a 15-Fr PEG tube is recommended because a smaller diameter may result in obstructions.4 In the current study, the obstruction rates were 11.1% for the 15-Fr PEG tube and 5.6% for the 20- or 22-Fr PEG tube, indicating a lower tendency for obstruction when the PEG tube diameter was above 15 Fr (p=0.327). A previous study reported that clogging of the PEG tube occurred in up to 45% of patients unless sufficient care was taken.20 The long-term management of the PEG insertion site is important to prevent clogging.
Spontaneous removal was more frequent in the introducer-type PEG insertion group than in the pull-type PEG insertion group, but this difference was not statistically significant (p=0.084). In the introducer-type PEG insertion group, the most likely reason for spontaneous removal was the spontaneous rupture of the balloon. In this method, the balloon was filled with saline and it had a lower durability than the mushroom-type bumper used in the pull-type PEG insertion technique. Van Dyck et al.23 reported that spontaneous removals were significantly higher for the introducer-type PEG insertion technique (17%) than the pull-type PEG insertion technique (0%; p<0.05).23
In the current study, there was no evidence of buried bumper syndrome within the cohort, which may have been a consequence of the fixed location of the tube. Generally, buried bumper syndrome is attributed to excessive traction of the tube towards the exterior of the patient. Previous studies have reported buried bumper syndrome at rates of between 2% and 6.1%.24,25 Comparing our data with those from medical centers that have reported buried bumper syndrome may help to further elucidate the causes underlying buried bumper syndrome.
There are several notable limitations to this study that are described next. The study was retrospective in its design and the data were gathered from patients' medical records only. There was also some follow-up loss in our cohort. For chronic complications such as granulation tissue or wound infection, there may be the possibility of some missed cases since some patients may have visited other hospitals following PEG complications. Acute complications were judged by chart review alone, so there is a possibility of incorrect assessment in this regard. The mortality caused by PEG insertion was also based on chart reviews. Regarding chronic-phase diseases and comorbidities, the causes of death could not be determined with certainty for some patients. Furthermore, issues associated with the PEG insertion sites, for example, infections or other delayed problems, may have been omitted. Another limitation of our analysis was the small number of complications and the numbers of cases that were compared were small, which together may have led to a lack of statistical power; therefore, future larger scale studies are required.
In conclusion, PEG insertion is considered a safe procedure to enable physiologic feeding of patients who are unable to eat normally. No procedure-related deaths occurred among the 141 cases who underwent PEG insertions in this study. In addition, most of the recorded complications were minor and no statistical differences were found between the pull-type and introducer-type PEG insertion methods with respect to the complication rates. Following PEG insertion, however, frequent vital sign checks are necessary during the first 24 hours to exclude uncommon but serious complications such as hemoperitoneum, even if symptoms of gastrointestinal bleeding are not evident.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Kirby DF, Delegge MH, Fleming CR. American Gastroenterological Association technical review on tube feeding for enteral nutrition. Gastroenterology. 1995;108:1282–1301. doi: 10.1016/0016-5085(95)90231-7. [DOI] [PubMed] [Google Scholar]
- 2.Larson DE, Burton DD, Schroeder KW, DiMagno EP. Percutaneous endoscopic gastrostomy. Indications, success, complications, and mortality in 314 consecutive patients. Gastroenterology. 1987;93:48–52. [PubMed] [Google Scholar]
- 3.ASPEN Board of Directors and the Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr. 2002;26(1 Suppl):1SA–138SA. [PubMed] [Google Scholar]
- 4.Loser C, Aschl G, Hébuterne X, et al. ESPEN guidelines on artificial enteral nutrition: percutaneous endoscopic gastrostomy (PEG) Clin Nutr. 2005;24:848–861. doi: 10.1016/j.clnu.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Gauderer MW, Ponsky JL, Izant RJ., Jr Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872–875. doi: 10.1016/s0022-3468(80)80296-x. [DOI] [PubMed] [Google Scholar]
- 6.Odelowo OO, Dasaree L, Hamilton Y, et al. Is repeat endoscopy necessary after percutaneous endoscopic gastrostomy. J Assoc Acad Minor Phys. 2002;13:57–58. [PubMed] [Google Scholar]
- 7.Russell TR, Brotman M, Norris F. Percutaneous gastrostomy. A new simplified and cost-effective technique. Am J Surg. 1984;148:132–137. doi: 10.1016/0002-9610(84)90300-3. [DOI] [PubMed] [Google Scholar]
- 8.Lang A, Bardan E, Chowers Y, et al. Risk factors for mortality in patients undergoing percutaneous endoscopic gastrostomy. Endoscopy. 2004;36:522–526. doi: 10.1055/s-2004-814400. [DOI] [PubMed] [Google Scholar]
- 9.Nair S, Hertan H, Pitchumoni CS. Hypoalbuminemia is a poor predictor of survival after percutaneous endoscopic gastrostomy in elderly patients with dementia. Am J Gastroenterol. 2000;95:133–136. doi: 10.1111/j.1572-0241.2000.01673.x. [DOI] [PubMed] [Google Scholar]
- 10.Blomberg J, Lagergren P, Martin L, Mattsson F, Lagergren J. Albumin and C-reactive protein levels predict short-term mortality after percutaneous endoscopic gastrostomy in a prospective cohort study. Gastrointest Endosc. 2011;73:29–36. doi: 10.1016/j.gie.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 11.Ermis F, Ozel M, Oncu K, et al. Indications, complications and long-term follow-up of patients undergoing percutaneous endoscopic gastrostomy: a retrospective study. Wien Klin Wochenschr. 2012;124:148–153. doi: 10.1007/s00508-011-0082-0. [DOI] [PubMed] [Google Scholar]
- 12.Cappell MS, Abdullah M. Management of gastrointestinal bleeding induced by gastrointestinal endoscopy. Gastroenterol Clin North Am. 2000;29:125–167. doi: 10.1016/s0889-8553(05)70110-2. [DOI] [PubMed] [Google Scholar]
- 13.Schapiro GD, Edmundowicz SA. Complications of percutaneous endoscopic gastrostomy. Gastrointest Endosc Clin N Am. 1996;6:409–422. [PubMed] [Google Scholar]
- 14.Luman W, Kwek KR, Loi KL, Chiam MA, Cheung WK, Ng HS. Percutaneous endoscopic gastrostomy: indications and outcome of our experience at the Singapore General Hospital. Singapore Med J. 2001;42:460–465. [PubMed] [Google Scholar]
- 15.Richter JA, Patrie JT, Richter RP, et al. Bleeding after percutaneous endoscopic gastrostomy is linked to serotonin reuptake inhibitors, not aspirin or clopidogrel. Gastrointest Endosc. 2011;74:22–34. doi: 10.1016/j.gie.2011.03.1258. [DOI] [PubMed] [Google Scholar]
- 16.Richter-Schrag HJ, Richter S, Ruthmann O, Olschewski M, Hopt UT, Fischer A. Risk factors and complications following percutaneous endoscopic gastrostomy: a case series of 1041 patients. Can J Gastroenterol. 2011;25:201–206. doi: 10.1155/2011/609601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faias S, Cravo M, Claro I, Lage P, Nobre-Leitão C. High rate of percutaneous endoscopic gastrostomy site infections due to oropharyngeal colonization. Dig Dis Sci. 2006;51:2384–2388. doi: 10.1007/s10620-006-9216-z. [DOI] [PubMed] [Google Scholar]
- 18.Sangster W, Cuddington GD, Bachulis BL. Percutaneous endoscopic gastrostomy. Am J Surg. 1988;155:677–679. doi: 10.1016/s0002-9610(88)80142-9. [DOI] [PubMed] [Google Scholar]
- 19.Gossner L, Keymling J, Hahn EG, Ell C. Antibiotic prophylaxis in percutaneous endoscopic gastrostomy (PEG): a prospective randomized clinical trial. Endoscopy. 1999;31:119–124. doi: 10.1055/s-1999-13658. [DOI] [PubMed] [Google Scholar]
- 20.Mathus-Vliegen LM, Koning H. Percutaneous endoscopic gastrostomy and gastrojejunostomy: a critical reappraisal of patient selection, tube function and the feasibility of nutritional support during extended follow-up. Gastrointest Endosc. 1999;50:746–754. doi: 10.1016/s0016-5107(99)70153-7. [DOI] [PubMed] [Google Scholar]
- 21.McClave SA, Chang WK. Complications of enteral access. Gastrointest Endosc. 2003;58:739–751. doi: 10.1016/s0016-5107(03)02147-3. [DOI] [PubMed] [Google Scholar]
- 22.Zopf Y, Konturek P, Nuernberger A, et al. Local infection after placement of percutaneous endoscopic gastrostomy tubes: a prospective study evaluating risk factors. Can J Gastroenterol. 2008;22:987–991. doi: 10.1155/2008/530109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Dyck E, Macken EJ, Roth B, Pelckmans PA, Moreels TG. Safety of pull-type and introducer percutaneous endoscopic gastrostomy tubes in oncology patients: a retrospective analysis. BMC Gastroenterol. 2011;11:23. doi: 10.1186/1471-230X-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma MM, Semlacher EA, Fedorak RN, et al. The buried gastrostomy bumper syndrome: prevention and endoscopic approaches to removal. Gastrointest Endosc. 1995;41:505–508. doi: 10.1016/s0016-5107(05)80012-4. [DOI] [PubMed] [Google Scholar]
- 25.Finocchiaro C, Galletti R, Rovera G, et al. Percutaneous endoscopic gastrostomy: a long-term follow-up. Nutrition. 1997;13:520–523. doi: 10.1016/s0899-9007(97)00030-0. [DOI] [PubMed] [Google Scholar]