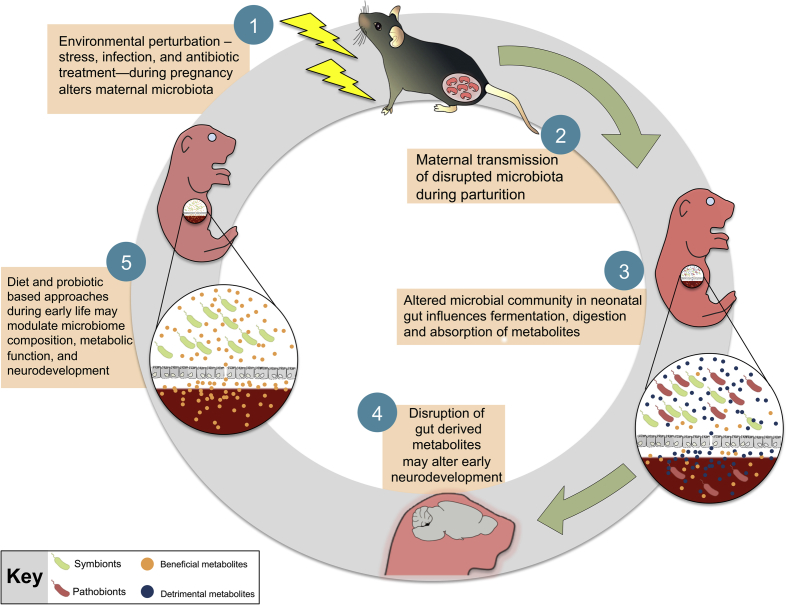
Fig. 1.
A proposed model for the role of maternal microbial transmission in early life programming and neurodevelopment. Environmental perturbations, such as stress or infection, during pregnancy destabilize the vaginal ecosystem that may lead to dysbiosis of the vaginal flora characterized by a shift from a Lactobacillus-dominant (symbionts) environment to overgrowth of opportunistic pathogens (pathobionts). Vertical transmission of a disrupted microbiota may compromise key developmental processes of the neonate, including the synthesis and absorption of microbe-derived metabolites, maturation of the gastrointestinal tract, and immune function. Outcompetition by pathobionts in the neonatal gut may increase production of detrimental metabolites and alter downstream neurodevelopmental events, including development of the hypothalamic-pituitary-adrenal (HPA) stress axis, as its development overlaps with early colonization patterns of the neonatal gut. Disruption during this critical window may result in long-term programming that persists even after stable core microbiota has been established. Administration of probiotics or dietary factors that promote maturation of the neonatal gut provide a promising avenue of therapeutic treatments by which to modulate microbiota composition, metabolic function, and neurodevelopment of the host.