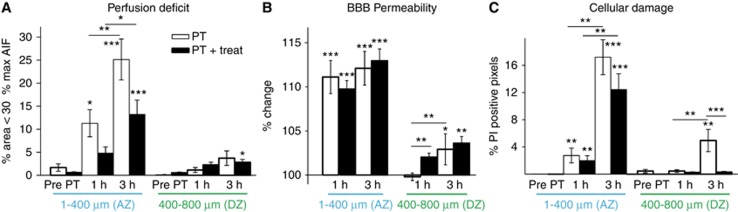
Figure 6.
Quantification of perfusion deficit, blood–brain barrier (BBB) permeability, and cell damage after photothrombosis—involvement of free radical signaling. (A) Perfusion deficit was assessed as percentage of area not crossing 30% of the maximum of the arterial input function (maxAIF). Although under control conditions <1% of the area was subthreshold (‘hypoperfused', combined groups PT (n=7) and PT+treat (n=9)), the hypoperfused area increased in both the treated and nontreated group. Treatment reduced the hypoperfused area, however, not reaching significance. The distant peri-ischemic zone (400 to 800 μm from ischemic core) remained largely unaffected. (B) Blood–brain barrier permeability increased early and robustly in the adjacent peri-ischemic zone with progression to the distant peri-ischemic zone 3 hours after photothrombosis. Blood–brain barrier alterations remained unaffected by treatment. (C) Mild increases in cell damage were observed early in the adjacent peri-ischemic zone becoming more profound and progressing to the distant peri-ischemic zone after 3 hours. Cell damage in the distant peri-ischemic zone was reduced by inhibition of free radical signaling. Statistical analysis was performed with nonparametric paired Friedman's analysis of variance for related samples and Mann–Whitney U-test for independent samples including Bonferroni post hoc correction. Each ring of 100 μm width was represented by one mean value. ***P<0.001; **P<0.01; *P<0.05. AZ, adjacent zone; DZ, distant peri-ischemic zone; PT, photothrombosis.