Abstract
Background
Unlike the widely used self rated health, the self rated mental health was found unsuitable as a proxy for mental illness. This paper analyses the relationships between the self ratings of physical health, mental health and overall health, and their association of with the objective indicators for physical and mental health.
Design and methods
The study is a secondary analysis of data from a nationwide representative sample of the non-institutionalized adult residents of Israel in 2003 that was collected via computer-assisted personal interview methods [n=4859].
Results
The self rated physical health and the self rated mental health were strongly related to each other yet the self rated mental health was not related to chronic physical conditions and the self rated physical health was not related to mental disorders. In a multiple logistic regression analysis, those with positive self rated mental health had 93 times the odds of reporting positive overall health whereas those with positive self rated physical health had 40 times the odds of reporting positive overall health.
Conclusions
The self rating of mental health presents a qualitatively different dimension from mental illness. The self rated mental health is two times more important than the self rated physical health in predicting the self rated overall health
Significance for public health.
The present study is an original study on the self rated physical, mental and overall health measures. Because of the wide range of associations with other health indicators, and the simplicity with which they are collected, self-rated health measures are widely used in large population surveys.
The present study questions the automatic assumption that the self rated mental health functions as a proxy measure of psychiatric morbidity, and suggests that the self rated mental health is more closely related to subjective well-being. The results show that self rated mental health predicts self rated general health better than self rated physical health.
Key words: self-report, mental-health, population surveys
Introduction
One of the most frequently used measures of health status is the question How would you rate your health?, a single question asking people to evaluate their overall health on a scale from excellent to poor. This single item measure has been demonstrated to be a robust predictor of health outcomes, including mortality, independent of health indicators of physical health.1-5
Because of the wide range of associations with other health indicators, and the simplicity with which it is collected, self-rated health is widely used in large population surveys as a proxy measure for general health status.6-10 Earlier studies assumed that the answer to this single question embodied a simple summation of all objective states, and therefore focused on the differences in prediction between the objective measures and the subjective self report.11
When the subjective self perception of health remained a strong predictor of mortality regardless of the statistical control of numerous objective health variables, it became clear that the simple question is not as simple as was originally thought.11
The attempts to understand what lies behind this measure produced studies that included mental/emotional variables in addition to physical health variables,11-16 and one explanation for the ability of the self rated health to predict mortality was that the single question of how would you rate your health is interpreted by subjects as referring to their overall health, including psychosocial aspects and not only to their physical health.11-16
Two studies showed that mental health was the mediator in the relationship between physical health and self reported general health.14,15
In one case, mental health was measured by the Anxiety and Depression Scale HADS and the study was done on 449 adults undergoing hip or knee replacement in hospitals in Canada.15 In the other case, mental health was measured by the Geriatric Depression Scale GDS in a longitudinal study of 150 older American adults.14
Another general population study from Germany found that in healthier individuals,16 positive affect was more important than physical functioning in predicting self rated general health, whereas among less healthy individuals the opposite was found. Positive affect in that study was measured by the Positive and Negative Affect Schedule (PANAS).
The single question How would you rate your mental health? was used in surveys much less than the single question about general health.17-21 Ahmad et al.20 conducted a review of the literature and found fifty-seven studies that included a measurement of self rated mental health (SRMH) but only four of these studies tried to validate the SRMH against known measures of mental health.
Self-rated mental health was associated with use of mental health services and of medical care services.11,20 When checked against other mental health indicators the use of SRMH as a proxy for mental morbidity was not recommended.18-20
Flieshman and Zuvekas examined the associations between SRMH and measures of psychological distress, activity limitations and social role functioning.18 They found that the measures of emotional/psychological distress were correlated with each other much more strongly than they were with SRMH, while SRMH was related to physical health. Their conclusion was that the self rated mental health was not a pure measure of mental morbidity and that it cannot be used as the sole indicator of psychological distress in surveys.
Mawani and Gilmour checked the associations between the SRMH, mental health diagnoses, WMH-CIDI diagnoses and measures of psychological distress.19 They found that a sizeable percentage of respondents who were classified as having mental disorders perceived their mental health as good; on the other hand, respondents who did not pass the threshold for diagnoses perceived their mental health as fair/poor. Their conclusion was that the SRMH should not be used as a proxy for mental morbidity because it underestimates the prevalence of mental morbidity, and may reflect other factors as well.19 To our knowledge, there were no studies that checked simultaneously the self ratings of physical health, mental health and overall health. Using data from a large representative sample of the adult population of Israel,22 that included the three self rating scales as well as other objective health status indicators, we tried to understand what is the contribution of the self rating of mental health to the self rating of general health.
Design and methods
The Israel National Health Survey followed procedures established by the World Mental Health Survey (WMH) of the World Health Organization (WHO).23 The sample was extracted from Israel’s National Population Register and constituted non-institutionalized legal residents aged 21 and over. The sample was designed to reflect the population distribution by age, gender and three population sectors: Arabs; post-1990 Jewish immigrants from the former Soviet Union; and Jews and others, including Jewish immigrants from countries other than the former Soviet Union.
The sample interviewed for the Israel National Health Survey was weighted back to the total population to compensate for unequal selection probabilities resulting from disproportionate stratification, clustering effects, and non-response. The weights were adjusted to make sample totals conform to known population totals taken from reliable Central Bureau of Statistics sources. On first personal contact with each potential survey respondent, the interviewer explained the survey and obtained verbal informed consent.16 Overall, 73% of those contacted agreed to be interviewed (88% of Arab-Israelis and 71% of Jewish-Israelis). If a person refused to participate, no replacement was made. A total of 4859 face-to-face interviews were conducted in Arabic, Hebrew or Russian at respondents’ homes from May 2003 to April 2004. Professional survey interviewers, who were trained and supervised by the Central Bureau of Statistics, used a laptop computer and computer-assisted personal interview methods. Interviews lasted an average of 60 minutes. The Human Subjects Committee based at Eitanim-Kfar Shaul hospital approved the survey and the field procedures in November 2000.22
The analyses presented here are based on the following sections of the interview schedule.
Diagnostic assessment
The diagnostic instrument used in the WHO-WMH was the Composite International Diagnostic Interview (CIDI).23
The survey assessed for: anxiety disorders [panic disorder, generalized anxiety disorder (GAD), agoraphobia without panic disorder, and post-traumatic stress disorder (PTSD)]; mood disorders (major depressive disorder, dysthymia, bipolar I and II disorders); and substance abuse disorders (alcohol abuse, alcohol dependency, drug abuse, drug dependency). The presence of a disorder was determined by whether respondents’ past or current symptoms met 30 days, 12-month or lifetime diagnostic criteria for a DSM IV disorder. For each disorder, a screening section was administered to the respondent. When a respondent endorsed a specific screening item, he or she was asked all the questions in the CIDI diagnostic section for that disorder to establish the presence of a current disorder. Organic exclusion criteria were taken into account in the determination of the DSM-IV diagnoses.
The validity of the WHO-WMH CIDI as a diagnostic tool was assessed in France, Italy, Spain, and the United States by a clinical reappraisal study which found that the individual-level concordance between the SCID and CIDI for 12-month prevalence of any mood disorder, any anxiety disorder, and any disorder overall was substantial (area under the curve in the range of 0.8 to 0.9.24 For the analyses reported here, respondents were grouped into those with or without any mood or anxiety disorder, because of a large overlap between the two groups of diagnoses. The present analysis distinguished between respondents with and without mood or anxiety disorder in the 30 days before the interview.
Chronic general medical conditions
The survey included a checklist of chronic general medical disorders and chronic pain. The conditions listed were heart attack, heart disease, stroke, high blood pressure, asthma, chronic obstructive pulmonary disorder, emphysema or other lung disease, tuberculosis, diabetes, kidney disease, neurological conditions, thyroid disease, cancer, chronic back or neck pain, arthritis or rheumatism, headaches, or any other chronic pain. In this analysis, respondents with chronic physical conditions were grouped into two categories: those reporting any one of the conditions and those reporting none.
Methodological research has shown that such checklists provide useful information about treated or currently untreated chronic conditions.25
Disability measure
The WHODAS is a disability scale that includes six scales: i) Role Functioning, ii) Cognition, iii) Mobility, iv) Self-care, v) Social Interaction and vi) Participation. The four questions that assessed Role Functioning were all frequency questions while other domains consist mostly of severity items. The calculation of the total score followed the method described in Buist-Bouwman:26 the resulting total score ranged between a score of 0 indicating no disability and 100 indicating maximum disability with intermediate scores indicating the percentage of the maximum possible score. In the present analysis, the total score was grouped into three categories: maximum disability =100, 9% of the entire sample, no disability =0.47% of the entire sample and partial disability 0> score <100, 44% of the entire sample.
Self report of physical health, mental health and general health
The rating of physical, mental and overall health were measured using the standard items How would you rate your …. excellent, very good, good, fair, or poor? Since the connotation of good was neither very good nor bad, the present analysis followed others and grouped all three variables into two categories: positive excellent/very good and negative good/fair/poor.13,14,27
The control variables included the socio-demographic characteristics: age groups, gender, marital status, education, income and population groups [classified as i) Arabs ii) post-1990 Jewish immigrants from the former Soviet Union iii) Jews and others, including Jewish immigrants from countries other than the former Soviet Union].
Statistical analysis
The data were weighted to adjust for the differential probabilities of respondents’ selection and non-response and for differences between the sample and the adult population in Israel. Cross tabulation of age groups by positive self rated physical health, positive self rated mental health ,presence of chronic physical conditions and presence of any depression or anxiety disorders was done to show how these measures change with age.
Logistic regression analyses were conducted to estimate the association between dichotomous positive/negative outcomes of self rated health measures and the socio-demographic and health status indicators. Estimates of odds ratios (ORs), the corresponding standard errors and 95% confidence intervals (CI) were also obtained from logistic regression using SUDAAN.28
Results
A total of 4859 men and women aged 21 and above completed the survey. Table 1 presents the distribution of the socio-demographic and health status indicators used in the analysis.
Table 1.
The study population: socio-economic and medical conditions, and self rated mental, physical, overall health (% of population ± standard error).
| N. | % (SE) | |
|---|---|---|
| Females | 2479 | 51 (0.5) |
| Age groups | ||
| 21-34 | 1585 | 34.9 (0.3) |
| 35-49 | 1317 | 27.8 (0.4) |
| 50-64 | 1080 | 21.5 (0.4) |
| 65+ | 877 | 15.8 (0.2) |
| Population groups | ||
| Jews & others | 3332 | 71.4 (0.4) |
| Arabs | 659 | 12.8 (0.3) |
| Immigrants | 844 | 15.8 (0.3) |
| Income | ||
| Low | 773 | 18.0 (0.6) |
| Low-average | 1472 | 32.0 (0.7) |
| High-average | 1717 | 33.9 (0.7) |
| High | 897 | 15.9 (0.5) |
| Marriage status | ||
| Married | 3229 | 67.8 (0.6) |
| Divorced/separated | 730 | 13.4 (0.5) |
| Never married | 900 | 18.7 (0.5) |
| Educational level | ||
| Low | 1068 | 21.7 (0.6) |
| Low-average | 1728 | 36.9 (0.7) |
| High-average | 800 | 16.2 (0.5) |
| High | 1263 | 25.2 (0.7) |
| Functioning in previous month (WHO-DAS) | ||
| Complete disability | 428 | 8.7 (0.4) |
| Partial disability | 2130 | 43.6 (0.7) |
| No disability | 2301 | 47.7 (0.7) |
| Self rated health | ||
| Self rated mental health (positive) | 2985 | 63.8 (0.6) |
| Self rated physical health positive) | 2311 | 49.8 (0.7) |
| Self rated overall health (positive) | 2553 | 55.6 (0.7) |
| WMH-DSM-IV mental disorder in previous month (yes) | 149 | 3.1 (0.3) |
| WMH-DSM-IV mental disorder in past year (yes) | 470 | 9.8 (0.4) |
| Any chronic physical condition (yes) | 2391 | 48.2 (0.7) |
SE, standard error.
We found that the 63% of the total sample rated their mental health as positive, 55% rated their overall health as positive but only 49% rated their physical health as positive. Men rated their health consistently better than females: 66.5% of the males rated their mental health as positive compared to 61% of the females (χ2=14.7; P<0.001), 52% of the males rated their physical health as positive compared to 48% of the females (χ2=11.8; P<0.01) and 58% of the males rated their overall health as positive compared to 53% of the females (χ2=11.2; P<0.01). Immigrants rated their health consistently lower (18%, 26%, 16% positive on the overall, mental and the physical health respectively) than the Arabs (55%, 61%, 54%) and the Jews and Others (64%, 73%, 56%) (P<0.001). Those with high income rated their health consistently better (60%, 69%, 54%) than those with low income (49%, 56%, 45%) (P<0.005). Those in the 21-34 age group rated their health consistently better (77%, 81%, 73%) than those in the 65+ age group (18%, 35%, 13%) (P<0.001). Those who never married rated their health consistently better (75%, 78%, 71%) than those who were divorced or separated (27%, 38%, 25%) (P=0.000) and those with high education rated their health consistently better (62%, 69%, 54%) than those with low education (36%, 45%, 31%) (P<0.005).
The relationship between health conditions, and self rated physical and mental health
Table 2 presents the associations between health status indicators and the self rated physical health (HSR) and mental health (MHSR). The odds ratios presented in the table were adjusted in the logistic regression for age, population groups, income, educational level and disability status. Table 2 shows that self rated positive physical health is strongly related to chronic physical conditions but much less to mental disorders. Likewise, self rated positive mental health is strongly related to mental disorders, but much less to chronic physical conditions.
Table 2.
Predictors of positive self rated physical and mental health status indicators: odds ratios and 95% confidence intervals.
| MHSR | HSR | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | Wald F | P | OR | 95% CI | Wald F | P | |
| Mental disorder in previous month | 7.8 | 4.65-13.07 | 60.64 | <0.001 | 0.74 | 1.22-3.21 | 1.1 | 0.30 |
| Any chronic physical condition | 0.92 | 0.77-1.1 | 0.75 | 0.39 | 3.64 | 3.07-4.32 | 216.9 | <0.001 |
| Age | 19.1 | <0.001 | 20.2 | <0.001 | ||||
| 21-34 | 4.3 | 2.9-6.3 | 4.4 | 3.0-6.4 | ||||
| 35-49 | 3 | 2.0-4.4 | 3.1 | 2.1-4.6 | ||||
| 50-64 | 2.3 | 1.6-3.4 | 2.4 | 1.6-3.5 | ||||
| 65+ | 1 | - | 1 | - | ||||
| WHO-DAS functioning in previous month | 4.8 | 0.01 | 6.1 | 0.01 | ||||
| Partial disability | 1.9 | 1.1-3.6 | 2.1 | 1.1-3.8 | ||||
| No disability | 2.5 | 1.3-4.6 | 2.7 | 1.5-4.9 | ||||
| 65+ | 1 | - | 1 | - | ||||
MHSR, self-related mental health; HSR, self-related physical health; OR, odds ratio; CI, confidence intervals. All predictions were adjusted to population groups, income and educational level.
The difference between self rated physical health and self rated mental health
Figure 1 shows how chronic physical conditions, mental disorders and the self rating scales of physical and mental health change with age. Figure 1 shows that the percentage of those with chronic conditions goes up from 32% in the 21-35 age group to 78% in the 65+ group (χ2=653.9; P<0.001) while the poor self rated physical health follows the same pattern with a rise from 27% to 87% χ2=1402.39; P<0.001). On the other hand, the mental health measures do not follow the same pattern. The poor self rated mental health goes up from 19.5% in the 21-35 age group to 64.8% in the 65+ group (χ2=609.98; P<0.001) while the percentage of those with any mental disorder does not change at all.
Figure 1.
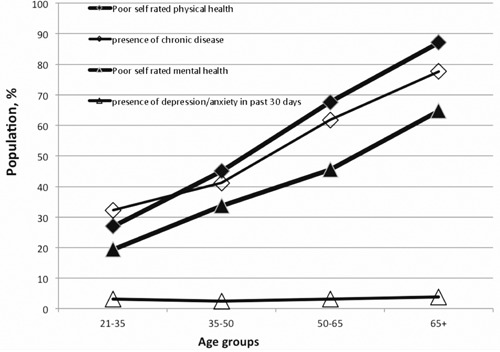
Rates of chronic physical conditions, depression/anxiety disorders, poor self rated physical and mental health, in four age groups.
The relationship of self rated overall health with the self rated physical and mental health
Table 3 presents the associations between self rated overall health (OSR) and the self rated physical and mental health in two models: with and without the health status indicators. The odds ratios presented here were adjusted in the logistic regression for the variables population groups, age groups and disability level.
Table 3.
Self rated physical and mental health status as predictors of positive overall self rated health: odds ratios and 95% confidence intervals.
| Model 1 | Model 1 | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | Wald F | P | OR | 95% CI | Wald F | P | |
| Self rated physical health, positive | 39.8 | 28.5-55.6 | 467.2 | <0.001 | 42.1 | 30.6-57.8 | 528.3 | <0.001 |
| Self rated mental health, positive | 93.5 | 65.6-133.3 | 630.7 | <0.001 | 97.2 | 68.1-138.9 | 633.2 | <0.001 |
| Mental disorder in previous month | 5.4 | 2.0-14.2 | 11.45 | <0.001 | - | - | - | - |
| Any chronic physical condition | 1.3 | 1.0-1.7 | 4.48 | 0.03 | - | - | - | - |
| Age | 19.1 | <0.001 | 20.2 | <0.001 | ||||
| 21-34 | 4.3 | 2.9-6.3 | 4.4 | 3.0-6.4 | ||||
| 35-49 | 3 | 2.0-4.4 | 3.1 | 2.1-4.6 | ||||
| 50-64 | 2.3 | 1.6-3.4 | 2.4 | 1.6-3.5 | ||||
| 65+ | 1 | - | 1 | - | ||||
| WHO-DAS functioning in previous month | 4.8 | 0.01 | 6.1 | 0.01 | ||||
| Partial disability | 1.9 | 1.1-3.6 | 2.1 | 1.1-3.8 | ||||
| No disability | 2.5 | 1.3-4.6 | 2.7 | 1.5-4.9 | ||||
All predictions were adjusted to gender population groups, income, marriage status and educational level. OR, odds ratio; CI, confidence interval.
Table 3 shows that self rated mental and physical health are much stronger predictors of OSR than the health status indicators of chronic conditions, mental disorders and disability. Those with positive self rated mental health have 93 times the odds of reporting good positive overall health whereas those with positive self rated physical health have 40 times the odds of reporting positive overall health. After accounting for the self rated health measures HSR and MHSR, the predictive value of the health status indicators is much smaller: those with no mental disorders are six times more likely to have a positive OSR, those with no disability have 2.5 times the odds of reporting positive OSR and those with no chronic condition have only 1.33% times the odds of reporting positive OSR. Yet, the age group is still a significant predictor of OSR beyond the self rating measures and the health status indicators. Table 3 showed that after accounting for the main health variables, positive self rated mental health was twice as important as positive physical health in the prediction of positive overall health. The odds for positive overall health were 93 higher if the rating of mental health was positive compared to 40 times higher if the rating of physical health was positive.
Discussion and conclusions
Data from the Israel National Health Survey based on a representative sample of the adult population was used to investigate the differences between the three self rated measures of health. The general distribution of the self rated measures of health replicates results obtained in previous large population surveys showing that rates of positive self rated health are lower among females compared to males,29 that older individuals rate their health as less positive compared to younger individuals and that socio demographic variables such as education and income are related to the self rating of mental, physical and overall health.3,11,30-34
The main findings from the present study show that the three self rating scales represent three different domains of health: the self rating mental health and the self rating physical health maintain their distinctiveness: self rated mental health is not related to chronic physical conditions (as does self rated physical health), and self rated physical health is not related to mental disorders (as does self rated mental health).
The self rating of physical health has a monotonic relationship with the objective indicator of physical health. The self rating of mental health does not have a monotonic relationship with the absence of mental illness. The good self rating of mental health goes down with age even though there is no age difference in mental disorders.
The self rated physical health and the self rated mental health are both strong predictors of the self rated overall health, independent of the objective measures of health. This was shown when the odds of predicting the self rating of the overall health remained the same regardless of whether the objective measures of health were included in the regression equation.
The self rated mental and physical health are 10 times stronger in predicting self rated overall health than any of the objective health indicators. The self rated mental health is two times more important than the self rated physical health in predicting the self rated overall health.
The stronger weight of the self rated mental health implies that the mental component in the self rating of overall health is stronger than the physical one. This result reinforces conclusions of previous studies: in a cross-national survey of university students in Germany, Bulgaria, and Poland, the overall self rated health status was assessed along with physical and psychological health as well as with social and socio demographic variables.34 That study found that psychosomatic complaints were the most important indicator in predicting the self rated health status. A similar finding was reported by Ormel et al.35 from a study using a large sample of late middle-aged and older persons living independently. They found that the unique contribution of depressive symptoms on poor health perception outranked those of the medical conditions.35
In a survey with a follow-up period of 1-5 years, elderly people were asked each year to provide their assessment of their health. Benyamini et al.36 found that those who were happier and more energetic at baseline rated their health better in the next 5 years, even after accounting for age, negative health indicators at baseline, disease status and functioning. Moreover, positive indicators of functioning; such as physical activity, work, and exercise; did not significantly predict future self assessment of health. The only strong predictor was the positive mood.
Mental health versus mental illness
Our results show a different age trajectory between mental health and mental illness.
Mental disorder was defined in our study by the presence of any mood or anxiety disorder in the past 30 days and its prevalence was the same in the four age groups.
Two major surveys checked the one year prevalence of any mood or anxiety and found it to be significantly less prevalent in older age groups.37,38
On the other hand, mental health which refers to hedonic well-being: feelings of happiness, satisfaction and interest in life, and to eudemonic well-being – optimal functioning and self –actualization, was more prevalent in younger age groups.
In their review of studies on the concept of mental health, Westerhof and Keyes found that older age was correlated with lower positive affect, less feeling of personal growth and purpose in life, less meaning in life and less social coherence and social contribution.39
The empirical separation between mental health and mental illness was found also by Weich et al.40 who used principal component analysis to describe the underlying factor structure of mental wellbeing. They found also that well-being and mental disorders are correlated but independent dimensions. Mental health is therefore a different concept from mental illness.
The use of three separate self rating scales for mental health, physical health and overall health enabled us to observe the unique contribution of the mental health component to the self rating of overall health. Further studies should investigate prospectively which of the three dimensions better predicts mortality, morbidity, hospitalizations or use of services.
Strengths and limitations
A key strength of this study was the utilization of a large representative sample of the entire adult population with a relatively high response rate. Trends observed in this type of sample are more likely to appear in other large population samples.
The main limitations of this study are that all the health information was self-reported and that the health indicators used may not have covered all the ill health domains. This could potentially explain the partial independence of the self rating scales.
Another limitation might be the wording of the self rating questions. It is not clear whether a more comparative wording compared to your age group would have changed the clear age gradient that was found in this study.
Acknowledgements
The national health survey was funded by the Ministry of Health with additional support from the Israel National Institute for Health Policy and Health Services Research and the National Insurance Institute of Israel. The views and opinions expressed in this chapter are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, or of the Government. The Israel Health Survey was carried out in conjunction with the World Health Organization/World Mental Health (WMH) Survey Initiative. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centers for assistance with instrumentation, fieldwork and consultation on data analysis. These activities were supported by the National Institute of Mental Health (NIMH; R01 MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, GlaxoSmithKline, and Bristol-Myers Squibb. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centers for assistance with instrumentation, fieldwork, and consultation on data analysis. None of the funders had any role in the design, analysis, interpretation of results, or preparation of this paper. A complete list of all within-country and cross-national WMH publications can be found at http://www.hcp.med.harvard.edu/wmh.
References
- 1.Idler EL, Benyamini Y.Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav 1997;38:21-37. [PubMed] [Google Scholar]
- 2.Sargent-Cox KA, Anstey KJ, Luszcz MA.The choice of self-rated health measures matter when predicting mortality: evidence from 10 years follow-up of the Australian longitudinal study of ageing. BMC Geriatr 2010;10:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeSalvo KB, Bloser N, Reynolds K, et al. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med 2006;21:267-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shadbolt B, Barresi J, Craft P.Self-rated health as a predictor of survival among patients with advanced cancer. J Clin Oncol 2002;20:2514-9. [DOI] [PubMed] [Google Scholar]
- 5.Tamayo-Fonseca N1, Quesada JA, Nolasco A, et al. Self-rated health and mortality: a follow-up study of a Spanish population. Public Health 2013;127:1097-104. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Available from: http://www.cdc.gov/brfss/questionnaires.htm. Accessed on: November 2014. [Google Scholar]
- 7.UK Data Survey. The general household survey. Available from: http://discover.ukdataservice.ac.uk/catalogue/?sn=5804&type=Data%20catalogue [Google Scholar]
- 8.Gray L, Merlo J, Mindell J, et al. International differences in self reported health measures in 33 major metropolitan areas in Europe. Eur J Public Health 2012;22:40-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.French DJ, Browning C, Kendig H, et al. A simple measure with complex determinants: investigation of the correlates of self-rated health in older men and women from three continents. BMC Public Health 2012;12:649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mavaddat N, Kinmonth AL, Sanderson S, et al. What determines Self-Rated Health (SRH)? A cross-sectional study of SF-36 health domains in the EPIC-Norfolk cohort. J Epidemiol Community Health 2011;65:800-6. [DOI] [PubMed] [Google Scholar]
- 11.Idler EL, Kasl S.Health perceptions and survival: do global evaluations of health status really predict mortality? J Gerontol 1991;46:S55-65 [DOI] [PubMed] [Google Scholar]
- 12.Arnadottir SA, Gunnarsdottir ED, Stenlund H, Lundin-Olsson L.Determinants of self-rated health in old age: a population-based, cross-sectional study using the International Classification of Functioning. BMC Public Health 2011;11:670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caetano SC, Silva CM, Vettore MV.Gender differences in the association of perceived social support and social network with self-rated health status among older adults: a population-based study in Brazil. BMC Geriatr 2013;13:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Segerstrom SC.Affect and self-rated health: a dynamic approach with older adults. Health Psychol 2014;33:720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perruccio AV, Davis AM, Hogg-Johnson S, Badley EM.Importance of self-rated health and mental well-being in predicting health outcomes following total joint replacement surgery for osteoarthritis. Arthritis Care Res (Hoboken) 2011;63:973-81. [DOI] [PubMed] [Google Scholar]
- 16.Schüz B, Wurm S, Schöllgen I, Tesch-Römer C.What do people include when they self-rate their health? Differential associations according to health status in community-dwelling older adults. Qual Life Res 2011;20:1573-80. [DOI] [PubMed] [Google Scholar]
- 17.Lee Y.The predictive value of self assessed general, physical, and mental health on functional decline and mortality in older adults. J Epidemiol Community Health 2000;54:123-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fleishman JA, Zuvekas SH.Global self-rated mental health: associations with other mental health measures and with role functioning. Med Care 2007;45:602-9. [DOI] [PubMed] [Google Scholar]
- 19.Mawani FN, Gilmour H.Validation of self-rated mental health. Available from: http://www.statcan.gc.ca/pub/82-003-x/2010003/article/11288-eng.pdf [PubMed] [Google Scholar]
- 20.Ahmad F, Jhajj AK, Stewart DE, Burghardt M, Bierman AS.Single item measures of self-rated mental health: a scoping review. BMC Health Serv Res 2014;14:398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang W, Ta VM.Social connections, immigration-related factors, and self-rated physical and mental health among Asian Americans. Soc Sci Med 2009;12:2104-12. [DOI] [PubMed] [Google Scholar]
- 22.Levinson D, Paltiel A, Nir M, et al. The Israel-world mental health survey: issues and methods. Isr J Psychiatry Related Sci 2007;44:85-93. [PubMed] [Google Scholar]
- 23.Kessler RC, Ustun TB.The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004;13:93-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health Surveys. Int J Methods Psychiatr Res 2006;15:167-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levinson D, Karger CJ, Haklai Z.Chronic physical conditions and use of health services among persons with mental disorders: results from the Israel National Health Survey. Gen Hosp Psychiatry 2008;30:226-32. [DOI] [PubMed] [Google Scholar]
- 26.Buist-Bouwman MA, Ormel J, de Graaf R, et al. Psychometric properties of the World Health Organization Disability Assessment Schedule used in the European Study of the Epidemiology of Mental Disorders. Int J Methods Psychiatr Res 2008;17:185-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Galenkamp H, Braam AW, Huisman M, Deeg DJ.Seventeen-year time trend in poor self-rated health in older adults: changing contributions of chronic diseases and disability. Eur J Public Health 2013;23:511-7. [DOI] [PubMed] [Google Scholar]
- 28.RTI International. SUDAAN Maintenance Release 8.0.2. Research Triangle Park: Research Triangle Institute; 2003. [Google Scholar]
- 29.Benyamini Y, Blumstein T, Lusky A, Modan B.Gender differences in the self-rated health-mortality association: is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist 2003;43:396-403. [DOI] [PubMed] [Google Scholar]
- 30.Chen H, Cohen P, Kasen S.Cohort differences in self-rated health: evidence from a three-decade, community-based, longitudinal study of women. Am J Epidemiol 2007;166:439-46. [DOI] [PubMed] [Google Scholar]
- 31.Zack MM, Moriarty DG, Stroup DF, et al. Worsening trends in adult health-related quality of life and self-rated health - United States, 1993-2001. Public Health Rep 2004;119:493-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singh-Manoux A, Martikainen P, Ferrie J, et al. What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. J Epidemiol Community Health 2006;60:364-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahs A, Westerling R.Self-rated health in relation to employment status during periods of high and of low levels of unemployment. Eur J Public Health 2006;16:294-304 [DOI] [PubMed] [Google Scholar]
- 34.Mikolajczyk RT, Brzoska P, Maier C, et al. Factors associated with self-rated health status in university students: a cross-sectional study in three European countries. BMC Public Health 2008;18;8:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ormel J, Kempen GI, Deeg DJ, et al. Functioning, well-being, and health perception in late middle-aged and older people: Comparing the effects of depressive symptoms and chronic medical conditions. J Amer Geriatrics Soc 1998;46:39-48. [DOI] [PubMed] [Google Scholar]
- 36.Benyamini Y, Idler EL, Leventhal H, et al. Positive affect and function as influences on self-assessments of health: expanding our view beyond illness and disability. J Gerontol B Psychol Sci Soc Sci 2000;55:107-16. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Birnbaum HG, Shahly V, et al. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depress Anxiety 2010;27:351-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trollor JN, Anderson TM, Sachdev PS, et al. Age shall not weary them: mental health in the middle-aged and the elderly. Aust N Z J Psychiatry 2007;41:581-9. [DOI] [PubMed] [Google Scholar]
- 39.Westerhof GJ, Keyes CL.Mental Illness and mental health: the two continua model across the lifespan. J Adult Dev 2010;17:110-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weich S, Brugha T, King M, et al. Mental well-being and mental illness: findings from the Adult Psychiatric Morbidity Survey for England 2007. Br J Psychiatry 2011;199:23-8. [DOI] [PubMed] [Google Scholar]


