Abstract
Background:
The use of transcutaneous electrical nerve stimulation (TENS) in dentistry was first described in 1967, by Shane and Kessler, but it has yet to gain widespread acceptance in dentistry. A study was undertaken to evaluate the effectiveness of TENS therapy as an adjuvant modality and to compare it with the conventional medication in controlling pain in temporomandibular disorder (TMD) patients.
Materials and Methods:
The study was carried out in the Department of Oral Medicine and Radiology, Yenepoya Dental College and Hospital, Mangalore. A total of 40 patients with the clinical symptom of pain associated with TMDs were randomly divided into two groups. Group A (control) patients were treated with medication (analgesics and muscle relaxants) alone, while group B patients were treated with TENS therapy in combination with medication. The intensity of the pain was assessed using the Visual Analog Scale (VAS). The results were analyzed with the student's ‘t’ test. A P-value < 0.05 was considered as significant.
Results:
A significant improvement was observed in both the TENS and the control group in terms of pain control. On comparative analysis, adjuvant TENS therapy was found to be more effective than medication alone, in controlling pain. (P value = 0.019).
Conclusion:
The observed data suggest that TENS therapy can be used as an adjuvant modality in the management of pain associated with TMDs. This study justifies the use of TENS therapy in the management of TMD.
Keywords: Temporomandibular disorder, temporomandibular joint, transcutaneous electrical nerve stimulation
INTRODUCTION
Temporomandibular disorders (TMD) represent a heterogeneous group of pathologies affecting the temporomandibular joints, the jaw muscles, or both.[1] They are the most common orofacial pain conditions of non-dental origin. They are frequently encountered in clinical practice, and their prevalence in the general population has been reported as being as high as 12%.[2] Pain can be present at any stage of TMDs and is a significant part of the symptoms that prompt patients to seek treatment. Treatments for TMDs are wide-ranging and directed primarily toward relief from persistent orofacial pain.
A wide variety of therapies proposed for TMD are orthopedic stabilization, intraoral appliances, behavioral therapy, placebo, and pharmacotherapy with analgesics, muscle relaxants, and antidepressants. An alternative mode of management is Transcutaneous Electric Nerve Stimulation (TENS). It is a method of pain relief by the application of an electronic device, which produces pulsed biphasic electrical waves through the electrodes placed on the skin surface. TENS is defined as the application of electrical stimulation to the skin for pain control. It is a well-known form of physical therapy, which is useful for the relief of pain. It is a safe, non-invasive, effective, and swift method of analgesia, and the potential adverse reactions of other methods of pain control are eliminated.[3] The purpose of this study was to determine the effectiveness of TENS as an adjuvant modality in the management of pain in TMD patients and to compare the effectiveness of the adjuvant TENS therapy with that of analgesic therapy in patients with TMD.
MATERIALS AND METHODS
The present study was carried out in the Department of Oral Medicine and Radiology, over a period of one-and-a-half years, on subjects reporting to the Dental Outpatient Department (OPD). Ethical clearance was acquired from the Ethical Committee of the Yenepoya Medical College, Yenepoya University, before the onset of the study. A total of 40 patients with a clinical symptom of pain associated with TMD were included in the study. Patients with a history of maxillofacial trauma, orofacial infections, and developmental anomalies of the maxillofacial region were excluded. General contraindications of the TENS therapy, such as, the presence of a cardiac pacemaker or a serious/unstable heart condition, epilepsy or allergy to adhesive tape or electrodes of the TENS machine were also considered as exclusion criteria.
The selected patients were randomly allocated into two equal groups. Prior informed consent was taken from all the patients. The patients in Group A were treated with medication [combination of analgesics and muscle relaxants — (ultrazox tablet-chlorzoxazone 250 mg, diclofenac potassium 50 mg, paracetamol 325 mg; manufactured by Ranbaxy Laboratories Ltd, Gurgaon, India) thrice daily, for five days], while patients in Group B were subjected to TENS (TENS machine manufactured by Bharat Medical Systems, Chennai, India) therapy in two sessions of 30 minutes each, separated five days apart, along with the above medication. The intensity of the pain was assessed using the Visual Analog Scale (VAS) before and after the treatment and the values were recorded. All the data obtained from all the patients were subjected to statistical analysis. Student's paired and unpaired t tests were used. A P value <0.05 was considered as significant.
RESULTS
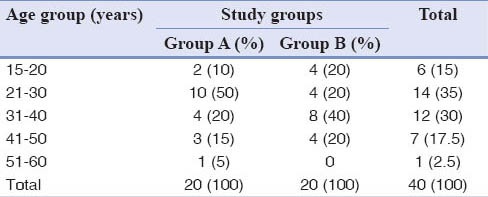
In this study, maximum number of patients was in the third decade of life with the youngest patient aged 20 years and the oldest patient was aged 55 years. There were six patients [15%] of age 20 years. Fourteen patients [35%] were in the age group of 21-30 years. Twelve patients [30%] were within 31-40 years of age. Eight patients [20%] were above 40 years of age, out of which only one patient was above 50years [2.5%] [Table 1].
Table 1.
Evaluation of the age group patterns in Group A and Group B
Out of the total 40 patients, 40% (16) were males and 60% (24) were females [Table 2].
Table 2.
Evaluation of the gender distribution in Group A and Group B

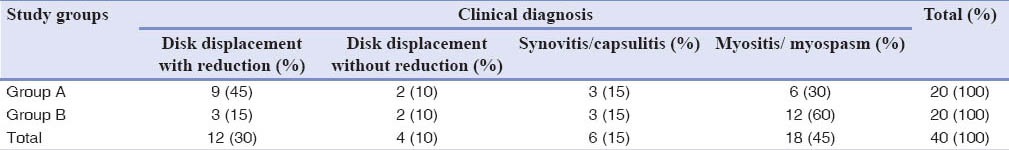
In this study there were 12 cases of disk displacement with reduction, four cases of disk displacement without reduction, six patients with synovitis/capsulitis, and 18 patients with myositis/myospasm [Table 3].
Table 3.
Evaluation of the sample distribution based on the clinical diagnosis
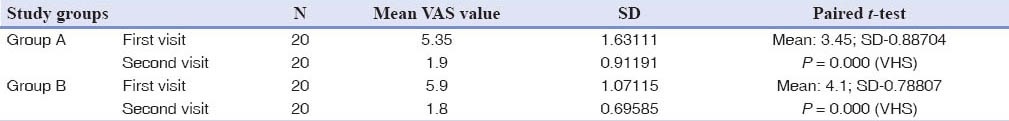
The mean pre-treatment VAS value in group A was 5.35 and the mean value for post-treatment VAS was 1.9. The mean paired difference was 3.45 ± 0.88704. The paired difference was statistically significant on the student's paired t-test. The P-value was <0.001. The mean pre-treatment VAS value in group B was 5.9 and the mean post-treatment VAS value was 1.8. The mean paired difference was 4.1 ± 0.78807. The paired difference was statistically significant on the student's paired t-test. The P-value was <0.001 [Table 4].
Table 4.
Evaluation of the pre-treatment and post-treatment VAS values
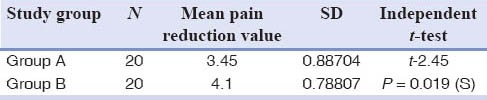
The mean pain reduction (VAS value of the first visit - VAS value of the second visit) in group A was 3.45 ± 0.88704; while in the group B it was 4.1 ± 0.78807. These data were subjected to the student's independent t-test and the difference was statistically significant. (P-value = 0.019) [Table 5].
Table 5.
Comparison of pain reduction in Group A and Group B
DISCUSSION
Analyzing the results of our study, the age of the patients ranged from 20 to 55years. Maximum patients were in the third (35%) and fourth (30%) decades of life, which is consistent with other studies done by Riden,[4] Juniper,[5] Okeson,[6] and Moger et al.,[7] where the common age of occurrence was reported to be in the second to fourth decades of life.
In this study, the maximum number of patients was female, that is, 24 (60%) were females and 16 (40%) were male patients. This female predilection is consistent with the studies done by Isacsson et al.,[8] Dworkin et al.,[9] and Jensen et al..[10] In recent times, Manfredini et al.[11] have also reported disk displacement in the absence of degenerative disorders, with a female : male ratio of 5 : 1. Similarly, Warren and Fried[12] and Nekora-Azak[13] have shown the highest prevalence among women of reproductive age, with the pattern of onset after puberty and lowered prevalence rates in the postmenopausal years, which suggests that the female reproductive hormones may play an etiological role in TMDs. LeResche et al.[14] have hypothesized that the presence of estrogen receptors in the TMJ of women, modulates the metabolic functions in relation to the laxity of the ligaments, and this could be relevant in TMD. Estrogens would act by increasing vigilance in relation to pain stimuli, modulating the activity of the limbic system neurons.
In our study, the mean pre-treatment VAS value in group B was 5.9 and the mean post-treatment VAS value was 1.8. The mean pain reduction (VAS value of the first visit- VAS value of the second visit) in group B was 4.1 ± 0.78807; while in group A it was 3.45 ± 0.88704. Statistical analysis showed that the difference in the mean pain reduction was significant, which implied that adjuvant TENS therapy was more effective than medication alone in relieving the pain associated with TMDs.
This was similar to the observations drawn from many other studies.
Rodrigues et al.[15] carried out a study to evaluate the effect of TENS on pain in the jaw elevator muscles in 35 TMD patients and found that a single TENS application is effective in pain reduction. Kato et al.[16] conducted a study in 18 TMD patients and found that TENS therapy significantly reduced pain and discomfort. Rajpurohit et al.[17] conducted a study to assess the effectiveness of TENS on the masticatory muscle pain in bruxism patients and found that TENS could be used as an effective pain-relieving modality in the treatment of masticatory muscle pain due to bruxism. In a study conducted on 45 patients with TMD, by Moger et al.[7], it was found that TENS therapy helped in relieving pain, especially muscular and chronic pain.
However, our result was not consistent with that of some other studies.
Kruger et al.[18] conducted a study to determine the effect of TENS plus conservative therapy (ibuprofen, bite plate, and self-physiotherapy) on myofascial pain dysfunction (MPD) and found that subthreshold TENS did not increase the symptom relief produced by conservative treatment. In a study conducted on 24 patients with bruxism, byAlvarez-Arenal et al.[19], it was found that use of an occlusal splint and TENS did not significantly improve the signs and symptoms of TMD.
The difference in pain reduction in the above studies compared to our study could be attributed to the disparity between the samples with regard to differences in biological, psychological, and social components affecting the TMDs, as well as the stimulation parameters used in the TENS therapy.
CONCLUSION
This study justifies the use of TENS therapy as an adjuvant modality in controlling pain associated with TMDs. The small size of the sample in the present study requires replication of these findings in a larger sample of patients with longer follow-up periods. The most important factor that has to be borne in mind by the clinician is that TENS therapy is only an initial symptomatic approach and not a definite or radical means of managing the TMDs.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Guarda-Nardini L, Piccotti F, Mogno G, Favero L, Manfredini D. Age-related differences in temporomandibular disorder diagnoses. Cranio. 2012;30:103–9. doi: 10.1179/crn.2012.015. [DOI] [PubMed] [Google Scholar]
- 2.Li LC, Wong RW, Rabie AB. Clinical effect of a topical herbal ointment on pain in temporomandibular disorders: A randomized placebo-controlled trial. J Altern Complement Med. 2009;15:1311–7. doi: 10.1089/acm.2009.0129. [DOI] [PubMed] [Google Scholar]
- 3.Giessler PR, McPhee PM. Electrostimulation in the treatment of pain in the mandibular dysfunction syndrome. J Dent. 1986;14:62–4. doi: 10.1016/0300-5712(86)90053-9. [DOI] [PubMed] [Google Scholar]
- 4.Riden DK. A clinical approach to pain. (448-9).Dental Update. 1986;13:439–46. [PubMed] [Google Scholar]
- 5.Juniper RP. Temporomandibular joint dysfunction: Facts and fallacies. Dental Update. 1986;13:479–80. [PubMed] [Google Scholar]
- 6.Okeson JP. 5th edition. Toronto: Mosby; 2003. Management of temporomandibular disorders and occlusion; p. 150. [Google Scholar]
- 7.Moger G, Shashikanth MC, Sunil MK, Shambulingappa P. Transcutaneous electrical nerve stimulation therapy in temporomandibular disorder: A clinical study. J Indian Aca Oral Med Radiol. 2011;23:46–50. [Google Scholar]
- 8.Isacsson G, Linde C, Isberg A. Subjective symptoms in patients with temporomandibular joint disk displacement versus patients with myogenic craniomandiublar disorders. J Prosthet Dent. 1989;61:70–7. doi: 10.1016/0022-3913(89)90112-1. [DOI] [PubMed] [Google Scholar]
- 9.Dworkin SF, Huggins KH, LeResche L, Von Korff M, Howard J, Truelove E, et al. Epidemiology of signs and symptoms in temporomandibular disorders: Clinical signs in cases and controls. J Am Dent Assoc. 1990;120:273–81. doi: 10.14219/jada.archive.1990.0043. [DOI] [PubMed] [Google Scholar]
- 10.Jensen R, Rasmussen BK, Pedersen B, Lous I, Olesen J. Prevalence of oromandibular dysfunction in a general population. J Orofac Pain. 1993;7:175–82. [PubMed] [Google Scholar]
- 11.Manfredini D, Piccotti F, Ferronato G, Guarda-Nardini L. Age peaks of different RDC/TMD diagnoses in a patient population. J Dent. 2010;38:392–9. doi: 10.1016/j.jdent.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Warren MP, Fried JL. Temporomandibular disorders and hormones in women. Cells Tissues Organs. 2001;169:187–92. doi: 10.1159/000047881. [DOI] [PubMed] [Google Scholar]
- 13.Nekora-Azak A. Temporomandibular disorders in relation to female reproductive hormones: A literature review. J Prosthet Dent. 2004;91:491–3. doi: 10.1016/j.prosdent.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 14.LeResche L, Saunders K, Von Korff MR, Barlow W, Dworkin SF. Use of exogenous hormones and risk of temporomandibular disorder pain. Pain. 1997;69:153–60. doi: 10.1016/s0304-3959(96)03230-7. [DOI] [PubMed] [Google Scholar]
- 15.Rodrigues D, Siriani AO, Bérzin F. Effect of conventional TENS on pain and electromyographic activity of masticatory muscles in TMD patients. Braz Oral Res. 2004;18:290–5. doi: 10.1590/s1806-83242004000400003. [DOI] [PubMed] [Google Scholar]
- 16.Kato MT, Kogawa EM, Santos CN, Conti PC. TENS and low-level laser therapy in the management of temporomandibular disorders. J Appl Oral Sci. 2006;14:130–5. doi: 10.1590/S1678-77572006000200012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rajpurohit B, Khatri SM, Metgud D, Bagewadi A. Effectiveness of transcutaneous electrical nerve stimulation and microcurrent electrical nerve stimulation in bruxism associated with masticatory muscle pain — a comparative study. Indian J Dent Res. 2010;21:104–6. doi: 10.4103/0970-9290.62816. [DOI] [PubMed] [Google Scholar]
- 18.Kruger LR, van der Linden WJ, Cleaton-Jones PE. Transcutaneous electrical nerve stimulation in the treatment of myofascial pain dysfunction. S Afr J Surg. 1998;36:35–8. [PubMed] [Google Scholar]
- 19.Alvarez-Arenal A, Junquera LM, Fernandez JP, Gonzalez I, Olay S. Effect of occlusal splint and transcutaneous electric nerve stimulation on the signs and symptoms of temporomandibular disorders in patients with bruxism. J Oral Rehabil. 2002;29:858–63. doi: 10.1046/j.1365-2842.2002.00923.x. [DOI] [PubMed] [Google Scholar]


