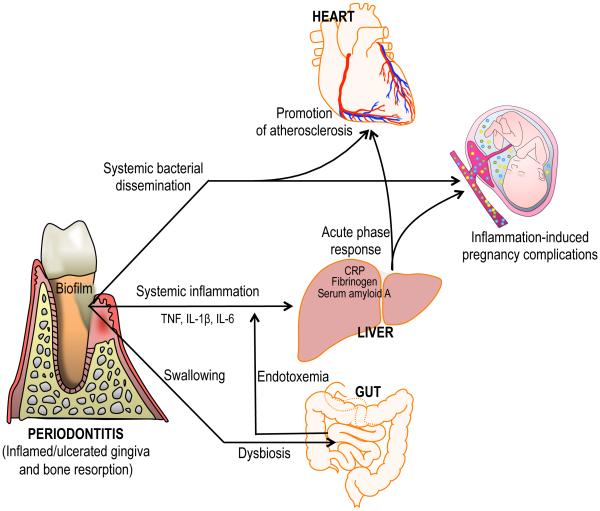
Figure 3. Biologically plausible mechanisms linking periodontitis to systemic inflammation and disease.
In periodontitis, locally produced pro-inflammatory cytokines can enter the systemic circulation and induce an acute-phase response in the liver — which is characterized by increased levels of C reactive protein, fibrinogen and serum amyloid A — in turn contributing to atherosclerosis or exacerbating intra-uterine inflammation. Moreover, gingival ulceration in periodontal pockets enables the egress and systemic dissemination of periodontal bacteria. Certain bacteria including Porphyromonas gingivalis have been detected in circulating leukocytes and in atherosclerotic lesions, where they may act as pro-atherogenic stimuli. Other periodontal bacteria such as Fusobacterium nucleatum have been detected in the placenta where they can cause adverse pregnancy outcomes. Large quantities of oral bacteria are constantly swallowed on a daily basis via the saliva into the gut. In this context, an alternative, or additional, mechanism linking periodontitis to systemic inflammation was recently proposed: Swallowed P. gingivalis causes alterations to the gut microbiota, thereby leading to increased gut epithelial permeability and endotoxemia, which causes systemic inflammation. Although independent, the depicted events are not mutually exclusive but could in principle occur simultaneously. CRP, C-reactive protein; IL, interleukin; TNF, tumor necrosis factor.