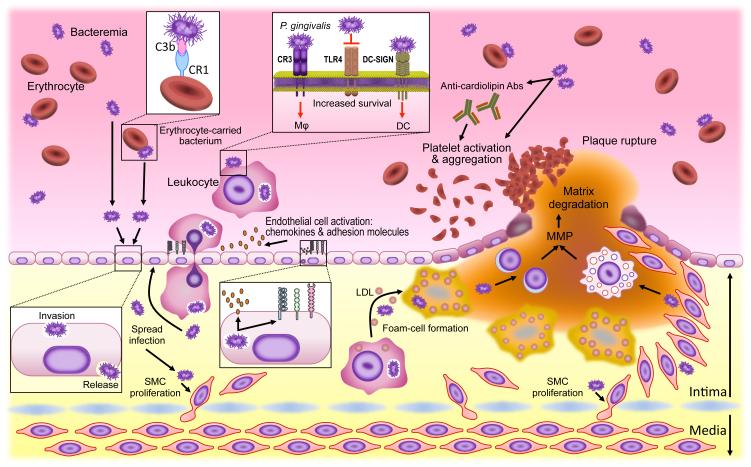
Figure 4. Microbial immune subversion in atherogenesis.
In addition to a bacteraemic route, periodontal bacteria may hijack leukocytes or erythrocytes (to which they attach via a C3b–CR1 interaction) to disseminate from the oral mucosa to aortic tissues. Bacteria not only invade but also activate endothelial cells (upregulation of cell adhesion molecules and chemokines) in ways that promote the transmigration of leukocytes that may harbour viable intracellular bacteria. The bacteria can spread to deeper tissues where they can induce smooth-muscle-cell proliferation in the intima. The uptake of low-density lipoprotein (LDL) by transmigrated macrophages is enhanced in the presence of bacteria leading to accelerated foam cell formation and atherogenesis. At later stages, atherosclerotic plaque rupture can be facilitated by bacterially induced production of matrix metalloproteinases (MMPs) by lymphocytes or myeloid cells. Bacteria-induced platelet aggregation (directly or through the induction of prothrombotic autoantibodies) may contribute to thrombotic vessel occlusion. Most of these studies supporting the above-discussed model utilized Porphyromonas gingivalis as model pathogen, the survival of which within leukocytes depends in part upon Toll-like receptor 4 (TLR4) evasion as well as on its capacity to exploit CR3 (in macrophages) or DC-SIGN (in dendritic cells) for safe intracellular entry. Abs, antibodies; CR1, complement receptor-1; CR3, complement receptor-3; DC, dendritic cell; DC-SIGN, DC-specific ICAM-3 grabbing nonintegrin; SMC, smooth muscle cell; TLR4, Toll-like receptor 4.