Highlights
-
•
Secondary chondrosarcoma in young Asian female arising from a benign solitary enchondroma in absence of multiple enchondromatosis is extremely rare.
-
•
Regular follow up including physical assessment and radiological imaging can result in earlier detection of malignant transformation obviating the need for aggressive surgical treatment involving multiple rib resections.
-
•
The aim of chest wall reconstruction is to avoid instability and prevent thoracic organs from being exposed.
-
•
Polypropylene mesh may be relatively weak in terms of mechanical support for the chest but if the defect is not too large, the laterally reflected pectoral muscle can provide enough support together with the mesh.
Keywords: Case reports, Chondrosarcoma, Enchondroma, Asian, Female
Abstract
INTRODUCTION
Enchondromas are benign tumours derived from cartilaginous tissue and they rarely undergo malignant transformation unless they occur in multiple sites such as in the case of Ollier disease.
PRESENTATION OF CASE
We report a rare case of a 36-year-old Chinese female, without any past medical history, who had a right chest wall tumour which was initially diagnosed to be benign, for which she was loss to follow up. The mass had been stable in size for the past 7 years until recently, when it gradually grew bigger. computed tomography (CT) scan of the thorax revealed that the mass had invaded the right chest wall suggestive of malignant change. She subsequently underwent an elective open right chest wall resection of the mass and chest wall reconstruction with mesh. A 3 cm by 3 cm tumour arising from the anterior aspect of the 4th rib was found intra-operatively. Post-operative course was uneventful. Histologically, the mass was confirmed to be chrondrosarcoma and resection margins were negative. The patient was discharged on 4th post-operative day and her latest CT thorax during follow up 2 years after operation did not show any tumour recurrence.
DISCUSSION
The aim of chest wall reconstruction is to avoid instability and prevent thoracic organs from being exposed if the defect size is ≥10 cm or at least three ribs are resected. Polypropylene mesh may be relatively weak in terms of mechanical support for the chest wall, however, in this case, the defect is not too large and the laterally reflected pectoral muscle can provide enough support together with the mesh.
CONCLUSION
Secondary chondrosarcoma in a young Asian female arising from a benign solitary enchondroma in the absence of multiple enchondromatosis, such as Ollier disease or Maffucci syndrome, is extremely rare. Regular follow up including physical assessment and radiological imaging can result in earlier detection of malignant transformation obviating the need for aggressive surgical treatment involving multiple rib resections.
1. Introduction
Chondrosarcomas involve the trunk often, but rarely arise from the chest. Surgical excision is the mainstay of treatment because they are not very responsive to radiotherapy or chemotherapy. The surgeon must ensure complete excision of the lesion with adequate margins to avoid recurrence, whilst not to injury surrounding structures and provide chest wall reconstruction to cover the defect if necessary.
2. Case
We describe a case of malignant transformation of a benign right chest wall tumour to chondrosarcoma in a young Asian female and the management of her condition.
A 36-year-old Chinese female presented with a seven-year history of a chest wall enchondroma, previously diagnosed via biopsy, that had enlarged in the recent months. She did not have any medical problems, neither did she smoke or drink. She was asymptomatic apart from the swelling. A chest radiograph was done at the clinic which showed a 3.3 cm × 3.8 cm opacity in the right middle zone with a well-defined inferior border and a poorly defined superior border. There was a marked increase in size compared to the chest radiograph seven years ago (Fig. 1). Computed tomography scan of the thorax revealed an extra-pulmonary soft tissue mass, measuring 4.2 cm × 3.8 cm, arising from anterior 3rd rib with some bony densities and specks of calcification, which was highly suggestive of a malignant lesion with invasion of the right chest wall (Figs. 2 and 3).
Fig. 1.
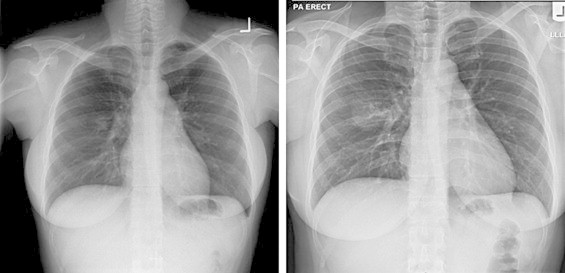
Comparison of chest radiographs of patient in 2006 (left) and 2013 (right).
Fig. 2.
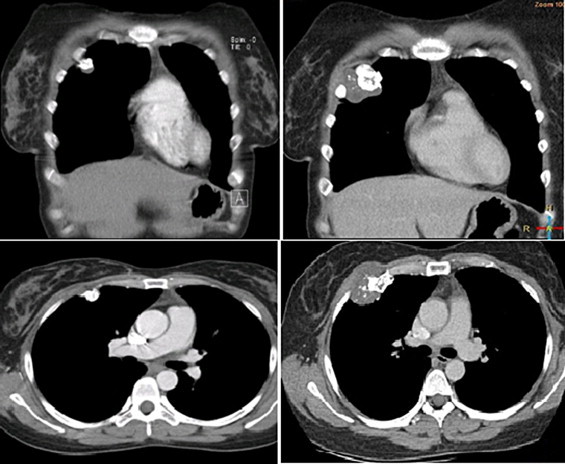
Comparison of computed tomography of thorax of patient in 2006 (left) and 2013 (right), coronal cuts (above), axial cuts (below).
Fig. 3.
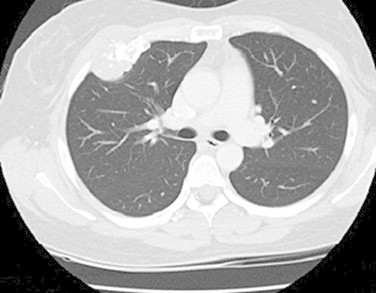
Lung window axial cut of computed tomography of thorax 2013.
She was then admitted electively for excision of the right chest wall tumour. Upon admission, her vitals were stable. On examination, she was well. There was a palpable hard mass approximately 3 cm × 3 cm over the right 3rd intercostal space which was mildly tender upon palpation and fixed to the chest wall. No other lump or axillary lymph node was palpable.
The patient subsequently underwent right chest wall tumour resection and reconstruction with mesh. Intra-operatively, a 3 cm × 3 cm tumour arising from the anterior aspect of the 4th rib was found which was removed en bloc including part of the 3rd to 5th ribs using diathermy and rib cutter with adequate margins of 3–4 cm (Fig. 4). The lungs, pleural and diaphragm were not involved by the tumour. The chest wall defect was about 6 cm × 8 cm and was reconstructed using a polypropylene mesh. Histologically, the mass was chondroid in nature, compatible with that of the diagnosis of grade 1–2 chondrosarcoma by the pathologist (Figs. 5 and 6). The margins of the specimen were negative of malignancy.
Fig. 4.

Gross image of resected chondrosarcoma (showing lesion posteriorly).
Fig. 5.
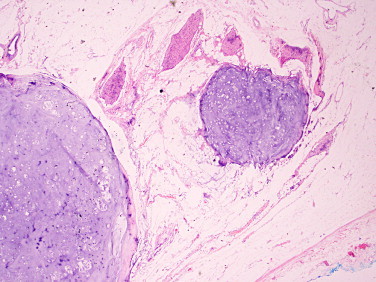
Histopathological findings of chondrosarcoma with soft tissue invasion.
Fig. 6.
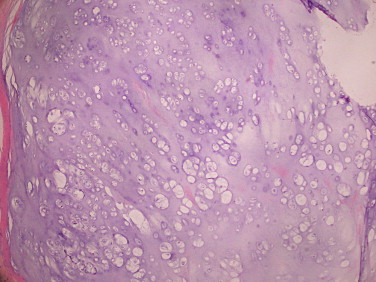
Histopathological findings of chondrosarcoma medium with grade 1–2 cytological features.
Her post-operative course was uneventful. Patient was subsequently discharged on 4th post-operative day and her latest CT scan on follow up 2 years after surgery did not show any recurrence.
3. Discussion
Chondrosarcomas generate chondroid matrix and are malignant. They can be primary, arising de novo, or secondary from pre-existing enchondroma or osteochondroma which underwent malignant transformation.1,2 They are the commonest primary chest wall tumour.3 The peak incidences for primary chondrosarcoma and secondary chondrosarcoma are 40–60 years of age and 25–45 years of age respectively.3 The usual presentation of a chest wall chondrosarcoma may include palpable mass or localised chest wall tenderness.4 Usual sites of secondary chondrosarcomas are anterior costochondral junction, costal angles, sternum and vertebral body.4 Computed tomography of the thorax depicts bony densities and specks of calcification.4 For this patient, the extensive resection with a margin of 3–4 cm was considered as sufficient.5 According to King and colleagues,6 the best outcomes were seen in patients who underwent extensive resection however in some cases, the safety margins may be difficult to achieve in view of location of tumour.
The surgeon has to watch out for the neurovascular bundle inferior to the ribs in resection of chest wall chondrosarcoma to avoid complications such as bleeding or nerve injury.
The chest wall has to be reconstructed to avoid instability and prevent thoracic organs from being exposed if the defect size is ≥10 cm or at least three ribs are resected.6,7 Artificial materials such as polypropylene mesh, composite mesh combined with expanded polytetrafluoroethylene seat, and autologous materials like musculocutaneous flaps are options for chest wall reconstruction. Polypropylene mesh may be relatively weak in terms of mechanical support for the chest wall, however, in this case, the defect is not too large and the laterally reflected pectoral muscle can provide enough support together with the mesh.
4. Conclusion
Secondary chondrosarcoma in a young Asian female arising from a benign solitary enchondroma in the absence of multiple enchondromatosis, such as Ollier disease8 or Maffucci syndrome, is extremely rare. Regular follow up including physical assessment and radiological imaging can result in earlier detection of malignant transformation obviating the need for aggressive surgical treatment involving multiple rib resections.
Conflict of interest
The authors declare that there is no conflict of interest.
Funding
There is no funding for the research.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author's contributions
Nieh Chih Chiang – formulation of the topic to write, literature review, writing manuscript, assisted in the operation.
Chua Yang Chong – assisted in the operation, gave ideas to improve the case report.
Thirugnanam Agasthian – vetting the report, and senior consultant in-charge of patient, also the person who operated on the patient.
Moe Htet Hlwan – vetting the report, assisted in the operation of the patient.
Acknowledgements
We would like to thank the NUH Radiology and Pathology Departments, in particular, Dr. Victor Lee, for their assistance in management of the patient and obtaining the histological specimens.
References
- 1.Mazanet R., Antman K.H. Sarcomas of soft tissue and bone. Cancer. 1991;68:463–473. doi: 10.1002/1097-0142(19910801)68:3<463::aid-cncr2820680304>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 2.Cakir O., Topal U., Bayram A.S. Sarcomas: rare primary malignant tumors of the thorax. Diagn Interv Radiol. 2005;11:23–27. [PubMed] [Google Scholar]
- 3.Terry S., Canale J.H.b. 11th ed. Mosby Elsevier; Philadelphia: 2008. Campbell's operative orthopaedics. [Google Scholar]
- 4.Shimoyama T., Suzuki R., Yoshiya K. Chondrosarcoma of the rib. Jpn J Thorac Cardiovasc Surg. 2003;51:167–171. doi: 10.1007/s11748-003-0056-x. [DOI] [PubMed] [Google Scholar]
- 5.McAfee M.K., Pairolero P.C., Bergstralh E.J. Chondrosarcoma of the chest wall: factors affecting survival. Ann Thorac Surg. 1985;40:535–541. doi: 10.1016/s0003-4975(10)60344-x. [DOI] [PubMed] [Google Scholar]
- 6.King R.M., Pairolero P.C., Trastek V.F. Primary chest wall tumors: factors affecting survival. Ann Thorac Surg. 1986;41:597–601. doi: 10.1016/s0003-4975(10)63067-6. [DOI] [PubMed] [Google Scholar]
- 7.Weyant M.J., Bains M.S., Venkatraman E. Results of chest wall resection and reconstruction with and without rigid prosthesis. Ann Thorac Surg. 2006;81:279–285. doi: 10.1016/j.athoracsur.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Choh S.A., Choh N.A. Multiple enchondromatosis (Ollier disease) Ann Saudi Med. 2009;29:65–67. doi: 10.5144/0256-4947.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]


