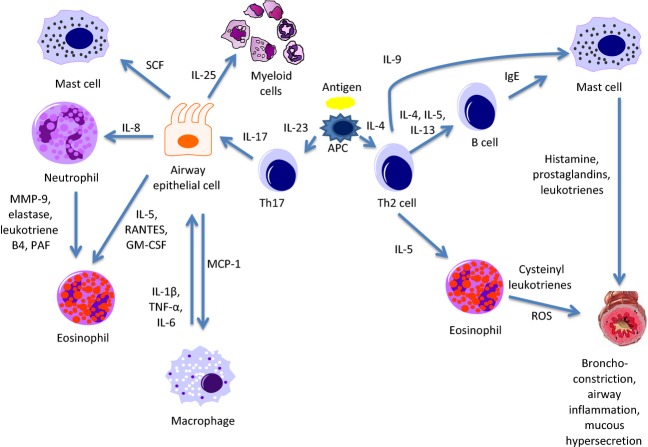
Figure 1.
Th2 and Th17 allergen responses in the asthmatic airway. Upon allergen presentation to Th0 cells by antigen-presenting cells (APC), Th cells differentiate into Th2 cells in the presence of IL-4, and Th17 cells in the presence of IL-23. Th2 cells then go on to produce IL-4-, IL-5-, and IL-13-activating B cells to release IgE which attaches to the surface of mast cells. When stimulated by antigen, mast cells release histamine, prostaglandins, and leukotrienes resulting in smooth muscle bronchoconstriction, airway inflammation, and mucous hypersecretion. Eosinophils activated by IL-5 produce cysteinyl leukotrienes and reactive oxygen species (ROS), which act in a similar manner on the airways, and additionally contribute to oxidative stress. Th17 cells producing IL-17 act on airway epithelial cells to stimulate the release of multiple factors. These factors include macrophage chemoattractant protein-1 (MCP-1) which recruits macrophages, IL-5, regulated on activation, normal T cell expressed and secreted (RANTES), and GM-CSF (granulocyte–macrophage colony-stimulating factor) which activate eosinophils, IL-8 which mobilizes neutrophils, stem cell factor (SCF) which works to promote mast cell survival, and IL-25 which induces myeloid cells to release Th2-type cytokines. Neutrophils release matrix metalloproteinase 9 (MMP9), elastase, leukotriene B4, and platelet-activating factor (PAF), which work to enhance the activity of eosinophils. Activated macrophages release IL-1, tumor necrosis factor alpha (TNF-α), and IL-6 which interact with other inflammatory cells and result in a positive feedback loop with airway epithelial cells.