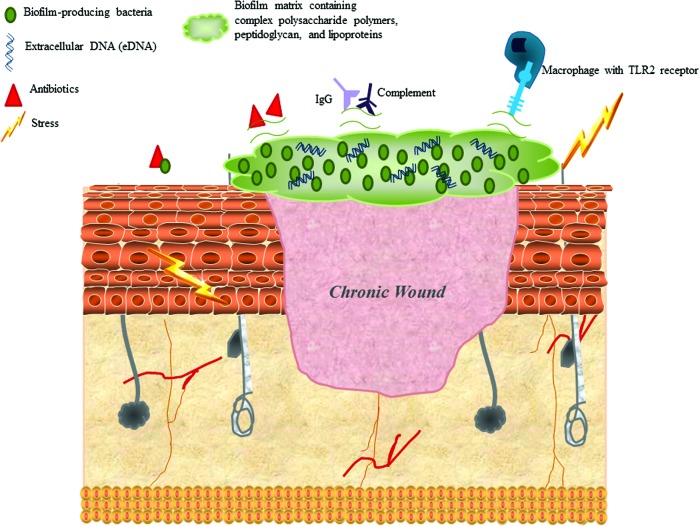
Figure 2.
Biofilm characteristics that are influenced by stress and allow bacteria to proliferate and survive. The most common biofilm-forming bacteria include Enterococcus faecalis, Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus viridans, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, and Pseudomonas aeruginosa. The biofilm matrix consists of complex polysaccharide polymers, peptidoglycan, lipoproteins, and extracellular DNA (eDNA), which may interfere with optimal engagement of potential ligands, such as toll-like receptors (TLRs). Some biofilms impair IgG and complement deposition, resulting in increased resistance to opsonization and phagocyte-mediated killing. Bacterial cells in the biofilm are in a different physiological status compared with planktonic cells, which minimizes sensitivity to antibiotics that target active cell processes. The biofilm matrix may also represent a diffusion barrier for some types of antibiotics. Stress is known to increase formation of biofilms in S. aureus, S. epidermidis, and E. coli by increasing adherence factors, altering iron availability, and enhancing virulence. Glucocorticoids and catecholamines alter host cytokine and proinflammatory response to biofilms and modulate bacterial metabolism. These modifications ultimately block the recognition of bacterial proteins by macrophage TLRs and impair bacterial clearance. These stress mediators also enhance the expression of bacterial surface proteins (e.g., adhesion molecules), which interferes with the interactions between host IgG and complement with bacterial targets.66 To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound