Introduction
Patients' involvement in healthcare and research has been a growing area in the last few decades. The World Health Organization (WHO) emphasizes the importance of personalized care of the chronic diseases in order to optimize care and treatment for the individual patient (WHO, 2005). In rheumatology, this has been highlighted by different organizations, such as The European League against Rheumatism (EULAR) (de Wit et al., 2013) and Outcome Measures in Rheumatology (OMERACT) (Kirwan et al., 2009), in order to increase the involvement of patients' perspective in care and research.
The rheumatic diseases consist of 80–100 diagnoses, and about 1 million people in Sweden are affected. The most common rheumatic diseases are rheumatoid arthritis, ankylosing spondylitis, osteoarthritis and chronic pain/fibromyalgia. The common denominators of the rheumatic diseases are that they are usually long lasting and affect the daily life of the patient, including pain, fatigue and problems with physical activity and function.
Previous research has shown that patients' perspectives of rheumatic diseases are insufficiently illuminated and that there are differences between patients' and health professionals' perspectives in relation to the rheumatic diseases and their consequences (Fair, 2003; Gorter et al., 2002; Stinson et al., 2008; Zangi et al., 2011). For example, patients focus on their illness experience and health professionals focus on the diseases in a general way. The quality of an encounter depends on the health professional's communications skills (Fair, 2003). Studies have shown that patients with rheumatic disease have needs that are not met by health services. Unmet needs are described as a lack of continuity, a lack of discussion with patients about the physical consequences of their disease and the need of patients to be treated as a person rather than as a disease (Bergsten et al., 2011; Kjeken et al., 2006; Lacaille et al., 2007; Leung et al., 2009; Sanderson et al., 2011). Patients' interests in health care and in research are highlighted as important aspects of the future of healthcare.
The Swedish Rheumatism Association (the national patient organization) and the Foundation of Research and Development at Spenshult decided to carry out a joint project to develop patient-initiated research into the rheumatic diseases. The project aimed to follow the working process of involving patients in a project group and to describe the research issues that were important from the patient's point of view.
The process of working with patients in the project group
The Swedish Rheumatism Association has educated patients to be research partners as a resource for researchers in the rheumatology field. Five research partners were asked to join the project group, together with a project leader with a formal research experience (a rheumatology nurse with a PhD). The research partners had experiences of different rheumatic diseases, such as rheumatoid arthritis, psoriasis arthritis, Sjögren's syndrome and fibromyalgia. As a method to enable and promote patients' interest, the dialogue model, developed by Abma et al. (Abma, 2006; Nierse et al., 2011) was chosen. This model involves a gradual and systematic approach to stimulate and maintain a dialogue between different stakeholders' issues and has been used in other disease areas, such as kidney disease, asthma, burns, diabetes, etc. (Abma, 2006; Nierse et al., 2011). It consists of six phases, comprising exploration, consultation, prioritization, integration, programming and implementation.
The exploration phase in this project included the setting up of the project as a joint project between the national patient organization and a research and development centre with a focus on clinical research in the field of rheumatology and with the creation of the project team.
The next phase was the consultation, which included identification of research ideas. As a first inventory of research ideas, a focus group interview was conducted within the project team. In order to get more views and ideas, three focus group interviews were conducted. The focus group interviews were directed by the project leader, together with one or two of the research partners who had been active observers at the group interview. The groups were created by different local patient organizations in order to generate more research ideas. The individuals who participated in the focus groups were in the age range 50–75 years, and comprised six men and 12 women with various rheumatic disorders, all of whom were engaged as members of the patient organization. As there were no younger participants in the focus groups, younger members from the local patient organizations were asked to participate for a personal interview and/or write down their thoughts and ideas. One person responded positively to this request and sent a written reply. The focus group interviews were recorded on audio tape and the interviews were also summarized and the data material analysed according to content analysis (Hsieh and Shannon, 2005). The work process also included a literature search after this phase in order to explore the existing evidence in the areas that were brought up. This literature search was done by the project leader and the result was shared with and discussed within the project group.
The processes of prioritization and integration were combined. The project group set an agenda of the research ideas from the results together with a prioritization and discussed the results and prioritization list with research members from the research department. The meeting with other researchers included presenting the results of the consultation phase, together with a preliminary prioritization. The integration phase led to new approaches to developing the ideas/areas into more elaborated research questions. The results of this discussion led to a new prioritization and moved the project on to the next phase, which was programming. This project ended with the phase of programming with a report to the Swedish Rheumatology Association, with the aim of taking this question further, into the last step of implementation.
New ideas in focus: when the patients set the agenda
The inventory of research ideas and areas of importance from the patient perspective resulted in several aspects of living of a chronic disease being highlighted, mostly focused on the patient's dignity, identity and quality of life (see Figure 1). The recurring theme was: ‘How can a person maintain or improve their quality of life despite a chronic illness?’ Persons who participated in the focus groups communicated their experiences of having a rheumatic disease, central to which is the impact that the condition has on all domains of life. Dignity was related to identity but these aspects were also separated from each other. The lack of holistic care was expressed as a feeling of being only partly human. The rheumatologist concentrated on the physical symptoms of the condition rather than the overall impact. Patients experienced a lack of whole-person care and expressed a feeling of not being treated with respect. Identity was related to the different roles in life, such as family, work and society. This could have consequences such as not being able to work or experiencing a demand to go to work without having the energy. This was related to the identity of being human. Quality of life was a concept that was discussed several times and in different contexts. The discussion in the project group at the prioritizing and integration phase ended with a research question: ‘what is quality of life for those of us living with rheumatic diseases?’ The way of measuring quality of life in healthcare was discussed and questioned. Do conventionally used questionnaires focus on the disease or on patients' perspectives of health? It became clear that patients experienced gaps in the support and assistance provided by health services and society in order to create quality of life.
Figure 1.
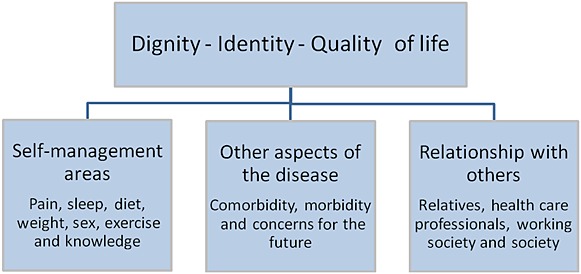
An overview of research ideas and areas of importance from the patient perspective
After the inventory of important research areas, a literature review showed that evidence existed for some areas that were highlighted but was lacking in other areas. The new areas of research involved the themes of dignity and identity, and questions were raised about how this was related to the personal experiences and what effect this could have on family life and/or working life. Evidence is lacking on the way that the loss of identity interferes with self-management strategies or affects a person's ability to continue work and be part of the society. The need to implement already known evidence became obvious. Areas that were highlighted, along with existing evidence in the literature on self-management strategies, included: pain, fatigue, life styles factors, exercise, sexuality and patient education. These strategies were not totally implemented in the provision of health care, according to the experiences of the patients in the present study. The implementation of new evidence is a difficult process and there is a well-known gap between the knowledge translation of research findings and clinical practice (Grimshaw et al., 2012). The present project showed that the need for knowledge translation about the consequences of living with rheumatic diseases is also relevant in other agencies in the community, such as workplaces and social insurance.
Conclusion
It is possible to involve patients in the early phase of research in order to gain new research ideas. The working process should preferably be well structured, and the present project was inspired by the dialogue model. This model clarified the steps in the process and helped to engage all stakeholders in the dialogue on an equal basis. As a result of the project, patients' views of important areas for research and implementation came into focus. This project is unique, in seeking to define research ideas that have sprung from patients' perspectives, which can lead to entirely new approaches. Since 2002, there has been a tradition in OMERACT to involve patient participation, and the results of this involvement have led to a widening of the research agenda. Important issues have been highlighted by this patient participation, such as fatigue, sleep disturbance and flares (de Wit et al., 2013). A study of patients' priorities in the area of neuromuscular diseases showed similar results and identified quality of life, self-management, cure and prevention as important issue that need further acknowledgment (Abma and Broerse, 2010). The involvement of patients, in a structured way, in research could help researchers to stay in tune with patients' needs (Gooberman-Hill et al., 2013). Chronic diseases demand different actions to acute diseases, and society, as well as healthcare organizations, need to adapt new approaches in order to manage chronic diseases in the future (WHO, 2005). The involvement of the people who are affected by the diseases in the planning of their healthcare, as well as in the field of research, could be a way to develop healthcare in chronic diseases.
REFERENCES
- Abma TA. Patients as partners in a health research agenda setting: The feasibility of a participatory methodology. Evaluation & the Health Professions. 2006;29:424–39. doi: 10.1177/0163278706293406. [DOI] [PubMed] [Google Scholar]
- Abma TA, Broerse JEW. Patient participation as dialogue: Setting research agendas. Health Expectations. 2010;13:160–73. doi: 10.1111/j.1369-7625.2009.00549.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergsten U, Bergman S, Fridlund B, Arvidsson B. “Striving for a good life” – The management of rheumatoid arthritis as experienced by patients. Open Nursing Journal. 2011;5:95–201. doi: 10.2174/1874434601105010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit M, Abma T, Koelewijn-van Loon M, Collins S, Kirwan J. Involving patient research partners has a significant impact on outcomes research: A responsive evaluation of the international OMERACT conferences. British Medical Journal Open. 2013;3:e002241. doi: 10.1136/bmjopen-2012-002241. doi: 10.1136/bmjopen-2012-002241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fair BS. Contrasts in patients' and providers' explanations of rheumatoid arthritis. Journal of Nursing Scholarship. 2003;35:339–44. doi: 10.1111/j.1547-5069.2003.00339.x. [DOI] [PubMed] [Google Scholar]
- Gooberman-Hill R, Burston A, Clark E, Johnson E, Nolan S, Wells V, Betts L PEP-R. Involving patients in research: Considering good practice. Musculoskeletal Care. 2013;11:187–90. doi: 10.1002/msc.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorter S, Scherpbier A, Brauer J, Rethans J-J, van der Heijde D, Houben H, van der Vleuten C, van der Linden S. Doctor-patient interaction: Standardized patients' reflections from inside the rheumatological office. Journal of Rheumatology. 2002;29:1496–500. [PubMed] [Google Scholar]
- Grimshaw JM, Eccles MP, Lavis J, Hill S, Squires J. Knowledge translation of research findings. Implementation Science. 2012;7:1–17. doi: 10.1186/1748-5908-7-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Kirwan JR, Newman S, Tugwell P, Wells G. Patient perspective on outcomes in rheumatology – A position paper for OMERACT 9. Journal of Rheumatology. 2009;36:2067–70. doi: 10.3899/jrheum.090359. [DOI] [PubMed] [Google Scholar]
- Kjeken I, Dagfinrud H, Mowinckel P, Uhlig T, Kvien T, Finset A. Rheumatology care: Involvement in medical decisions, received information, satisfaction with care, and unmet health care needs in patients with rheumatoid arthritis and ankylosing spondylitis. Arthritis and Rheumatism. 2006;55:394–401. doi: 10.1002/art.21985. [DOI] [PubMed] [Google Scholar]
- Lacaille D, White MA, Backman C, Gignac M. Problems faced at work due to inflammatory arthritis: New insights gained from understanding patients' perspective. Arthritis and Rheumatism. 2007;57:1269–79. doi: 10.1002/art.23002. [DOI] [PubMed] [Google Scholar]
- Leung YY, Tam LS, Lee KW, Leung MH, Kun EW, Li EK. Involvement, satisfaction and unmet health care needs in patients with psoriatic arthritis. Rheumatology (Oxford) 2009;48:53–6. doi: 10.1093/rheumatology/ken410. [DOI] [PubMed] [Google Scholar]
- Nierse CJ, Schipper K, van Zadelhoff E, van de Griendt J, Abma T. Collaboration and co-ownership in research: Dynamics and dialogues between patient research partners and professional researchers in a research team. Health Expectations. 2011 doi: 10.1111/j.1369-7625.2011.00661.x. doi: 10.1111/j.1369-7625.2011.00661.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson T, Calnan M, Morris M, Richards P, Hewlett S. Shifting normalities: Interactions of changing conceptions of a normal life and the normalisation of symptoms in rheumatoid arthritis. Sociology of Health & Illness. 2011;33:618–33. doi: 10.1111/j.1467-9566.2010.01305.x. [DOI] [PubMed] [Google Scholar]
- Stinson JN, Toomey PC, Stevens B, Kagan S, Duffy C, Huber A, Malleson P, McGrath P, Yeung R, Feldman B. Asking the experts: Exploring the self-management needs of adolescents with arthritis. Arthritis and Rheumatism. 2008;59:65–72. doi: 10.1002/art.23244. [DOI] [PubMed] [Google Scholar]
- WHO. Preparing a health care workforce for the 21st century. 2005. Available at http://www.who.int/chp/knowledge/publications/workforce_report.pdf [Accessed 14 April 2014]
- Zangi HA, Hauge MI, Steen E, Finset A, Hagen KB. “I am not only a disease, I am so much more”. Patients with rheumatic diseases' experiences of an emotion-focused group intervention. Patient Education and Counseling. 2011 doi: 10.1016/j.pec.2010.12.032. Available at http://dx.doi.org/10.1016/j.pec.2010.12.032. [DOI] [PubMed] [Google Scholar]


