Figure 3.
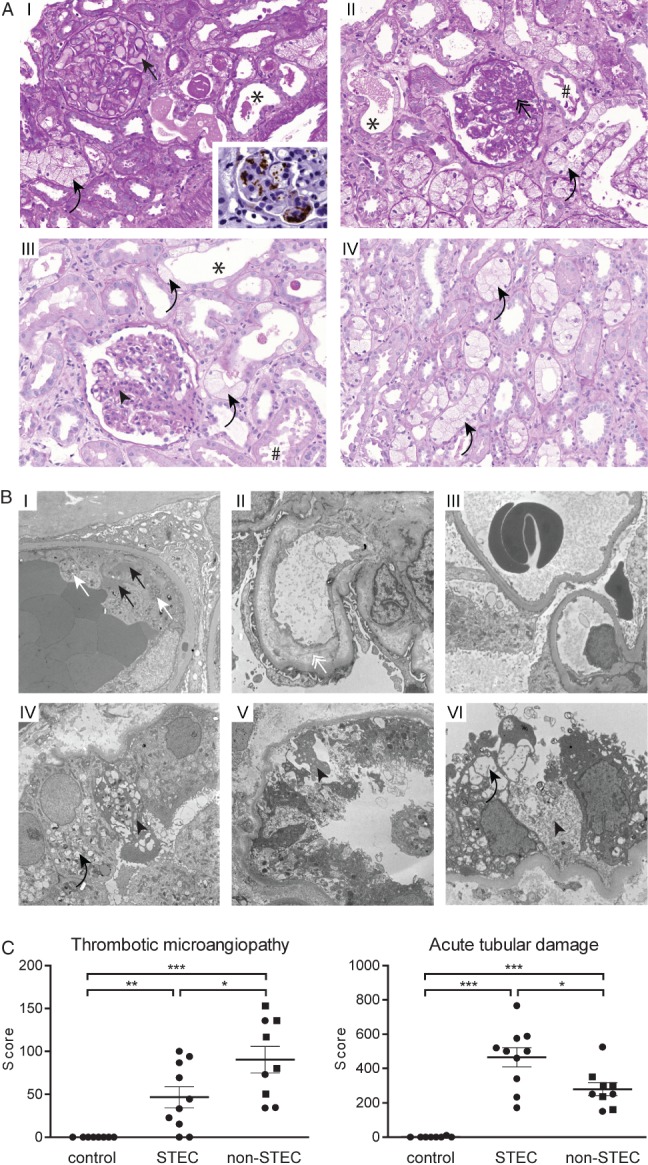
In addition to TMA, STEC-infection caused a profound tubular injury in man. (A) Light microscopy: a part of the biopsies showed glomeruli with congested capillaries filled with red bold cells (I, black arrow) and platelet-containing thrombotic material, visualized as a brown signal in CD61 immunohistochemistry (I, inlay). Other cases predominantly showed glomeruli with segmental sclerosis and wrinkling and collapse of capillaries (II, black double arrow), indicating a preceding but not active TMA. Glomeruli of other biopsies had almost normal architecture, with only a slight mesangial matrix increase (III, black arrowhead). A constant finding in all biopsies was a pronounced acute tubular damage, manifested as epithelial flattening (*) and/or presence of intraluminal cell detritus (#) and/or pronounced vacuolization (I–IV, black curved arrows); PAS staining, magnification = ×250. (B) Transmission electron microscopy of glomeruli (I–III) and tubular epithelium (IV–VI). Active TMA was documented by the presence of thrombotic material composed of platelets (I, white arrows) and fibrin strands (I, black arrows) in glomerular capillaries. Endothelial damage was manifested as absence of endothelial fenestrae and widening of the subendothelial space (II, white double arrow). In two patients the glomeruli showed normal architecture (III). Ultrastructural correlates of the pronounced tubular damage manifested as vacuolization (IV and VI, black curved arrows) and epithelial necrosis (IV–VI, black arrowheads); electron micrographs, lead citrate/uranyl acetate staining; magnification = (glomeruli) × 5000; (tubules) × 6300. (C) The extent of the glomerular TMA and acute tubular damage were compared between normal kidney tissue (tumour-free parts of tumour nephrectomies, control, n = 8), kidney biopsies from STEC-infected patients (STEC, n = 10) and randomly chosen biopsies from patients with STEC-unrelated TMA (non-STEC, n = 9; individuals > 45 years are depicted as squares). Glomerular TMA was semi-quantified on a PAS-stained slide by scoring the extent of TMA in each glomerulus. Acute tubular damage was assessed by building a score reflecting the following three criteria: brush border loss in proximal tubules; epithelial cell flattening; and vacuolization. Although the extent of TMA was less, the tubular damage was significantly higher in the STEC group than in the non-STEC group; data are shown as mean ± SEM; statistical differences were tested by two-tailed Mann–Whitney test; *p < 0.05; **p < 0.01; ***p < 0.001
