Abstract
Health literacy is related to a broad range of health outcomes. This study was designed to develop a psychometrically sound instrument designed to measure cancer health literacy along a continuum (CHLT-30), to develop another instrument designed to determine whether a patient has limited cancer health literacy (CHLT-6), and to estimate the prevalence of limited cancer health literacy. The Cancer Health Literacy Study involving 1,306 Black and White cancer patients was conducted between April 2011 and April 2013 in the Virginia Commonwealth University Massey Cancer Center and surrounding oncology clinics. A continuous latent variable modeling framework was adopted to dimensionally represent cancer health literacy, whereas discrete latent variable modeling was used to estimate the prevalence rates of limited cancer health literacy. Self confidence about engaging in health decisions was used as the primary outcome in external validation of new instruments. Results from a comprehensive analysis strongly supported the construct validity and reliability of the CHLT-30 and CHLT-6. For both instruments, measurement invariance tests ruled out item/test bias to explain gender and race/ethnicity differences in test scores. The limited cancer health literacy rate was 18%, a subpopulation consisting of overrepresented Black, undereducated, and low-income cancer patients. Overall, the results supported the conclusion that the CHLT-30 accurately measures cancer health literacy along a continuum and that the CHLT-6 efficiently identifies patients with limited cancer health literacy with high accuracy.
The Institute of Medicine defines health literacy as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions (Ratzan & Parker, 2000). Patients with limited health literacy tend to overuse emergency services and experience high rates of disease recurrence, both of which lead to high hospitalization rates and extended hospital stays (DeWalt, Berkman, Sheridan, Lohr, & Baker, 2004; Paasche-Orlow & Wolf, 2007). Health literacy is critically important for cancer patients who must make a complex set of diagnostic and treatment-based decisions at times of physical and emotional distress (Katz, Belkora, & Elwyn, 2014; Thome, Oliffe, Stajduhar, 2013; Walter & Covinsky, 2001).
The current state of knowledge on health literacy of cancer patients relies heavily on scores from two instruments: The Test of Functional Health Literacy in Adults and its short version (TOFHLA and S-TOFHLA, respectively; Parker, Baker, Williams, & Nurss; 1995) and the Rapid Estimate of Adult Literacy in Medicine (REALM; Davis et al., 1991). For both instruments, test scores are commonly used to infer the extent of health literacy and also to identify individuals with limited health literacy using a cut-score. However, we found no evidence of the association between TOFHLA and REALM scores and engagement in health decisions for persons with cancer. This is a major limitation of these instruments because the ability to make appropriate health decisions is the primary outcome of health literacy (Ratzan & Parker, 2000). Furthermore, the content of these instruments covers primarily reading proficiency, not specifically health literacy, emphasizes word recognition, as opposed to understanding, and are biased toward certain subpopulations (Dumenci, Matsuyama, Kuhn, Perera, & Siminoff, 2013; Pleasant, 2009). Last, these instruments were not designed specifically for persons with cancer and no instruments were found that were specifically designed to measure cancer health literacy. An instrument specific to cancer is useful because of the complex treatment choices patients face along with the increased demand for self-care. Given the extensive human suffering and other costs of cancer diagnosis and care, a health literacy instrument designed for patients with cancer appears to be needed. Other chronic illnesses that require an engaged patient to assure optimal outcomes, such as diabetes and hypertension, may also warrant specific health literacy measures.
The primary objective of this study was to develop two instruments, one designed to measure cancer health literacy along a continuum and the other designed to identify patients with limited cancer health literacy. The continuous latent variable framework (Joreskog, 1969) was adopted for measuring the construct of cancer health literacy along a continuum in the first instrument. To circumvent problems associated with arbitrarily assigning cutpoints (Dumenci, 2011; Rindskopf & Rindskopf, 1986; Rupp, Templin, & Henson, 2010), the discrete latent variable framework (Goodman, 1974), a model-based approach, was adopted to distinguish the categories of cancer health literacy in the second instrument. An instrument designed to efficiently identify a subgroup of patients with limited cancer health literacy has important clinical implications. Notifying physicians and pharmacists early on in care delivery, for example, would allow for timely interventions designed to reduce risk of adverse health outcomes for patients with limited cancer health literacy.
Method
Participants
The target population consisted of English-speaking cancer patients 18 years of age or older. Excluded from the study were individuals with Eastern Cooperative Oncology Group performance states score of 4, a history of referral to hospice care, or those unable to complete the task as determined by their oncologists. The exclusion criteria were adopted to minimize patient burden. We enrolled 1,306 cancer patients (age range = 18–93 years; M = 58.5, SD = 11.9). Patients almost exclusively self-identified as either non-Hispanic Black (37.7%) or non-Hispanic White (61.7%). The sample was heterogeneous in terms of educational attainment, cancer diagnosis, health insurance and marital status (see Table 1). This study was approved by the Institutional Review Board of Virginia Commonwealth University.
Table 1.
Demographic characteristics of patients with cancer (N = 1,306)
| Variable | % |
|---|---|
| Female | 54.8 |
| Race/ethnicity | |
| African American | 37.7 |
| White | 61.7 |
| Other | 0.6 |
| Education | |
| Less than high school | 12.9 |
| GED | 2.8 |
| High school diploma | 14.7 |
| Some collage | 19.8 |
| Associate/technical degree | 11.0 |
| Bachelor’s degree | 23.1 |
| Less than bachelor’s | 15.5 |
| Refused | 0.1 |
| Marital status | |
| Married/partnership | 52.4 |
| Never married | 17.1 |
| Widowed | 7.4 |
| Divorced/separated | 23.1 |
| Colon/rectal/anal | 6.2 |
| Diagnosis (cancer type) | |
| Colon/rectal/anal | 6.2 |
| Gastrointestinal | 4.2 |
| Breast | 16.3 |
| Hematologic | 8.1 |
| Head and neck | 26.2 |
| Skin | 11.7 |
| Endocrine | 3.0 |
| Genitourinary | 10.3 |
| Gynecologic | 9.4 |
| Other | 2.2 |
| Unknown | 0.7 |
| Health insurance | |
| Private | 46.6 |
| Public | 50.2 |
| Uninsured | 2.8 |
| Other | 0.3 |
| Recurrence | 7.0 |
| Remission | 28.6 |
| Undergoing chemotherapy | 19.1 |
| Undergoing radiation therapy | 4.0 |
Study Design
The Cancer Health Literacy Study was conducted between April 2011 and April 2013 in the Virginia Commonwealth University Massey Cancer Center and surrounding oncology clinics. A mixed method design was used. The study started with a qualitative phase to identify the boundaries of cancer health literacy and what it entails to ensure a comprehensive content coverage by bringing in perspectives from health literacy scholars, clinicians, and cancer patients. A list of cancer health literacy items, the outcome of the qualitative phase, was administered to 1,306 cancer patients. The data were then used in the quantitative phase to create the final instruments and provide validity and reliability evidence.
The qualitative phase first used a Delphi Panel to discuss domains of health literacy and evaluate various definitions of health literacy as it relates to these domains. The Delphi Panel involved online discussions between geographically dispersed physicians, nurses, medical librarians, and prominent health literacy researchers (n = 11). The panelists were anonymous to encourage candid discussion and debate and transcripts of these discussions were used in the analysis. In addition to our panel of experts, we conducted and recorded six focus group sessions, each with six to eight patients with cancer (n = 39), to elicit their understanding of cancer health literacy. Overall, 54% of the focus group participants were female and 46% male, with 59% Black, 39% White, and 2% Native American. Each group included participants from both gender and race/ethnicity groups. To understand how education influences topics related to health literacy, groups were separated by level of completed education. Three groups included participants who completed more than a high school education and three groups consisted of participants with a high school degree or less. The composition and results of the focus groups are discussed in detail elsewhere (Cartwright, Dumenci, Siminoff, & Matsuyama, 2014).
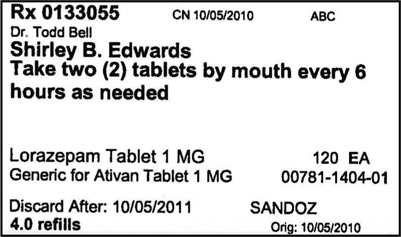
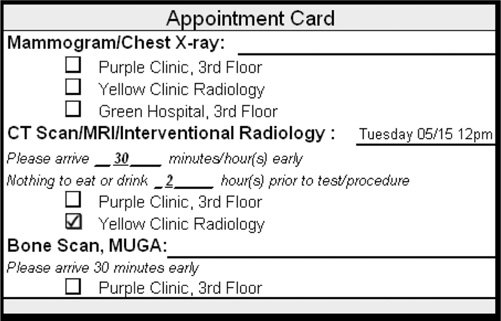
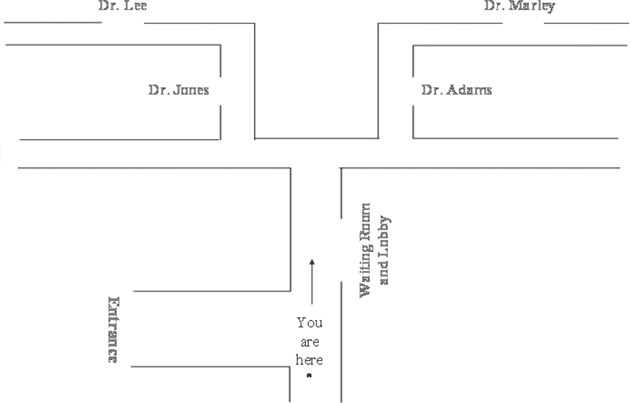
For both the Delphi Panel and focus groups, qualitative content analysis (Ritchie, 2003) was used to analyze the transcripts. Transcripts from the Delphi Panels and focus groups were supplemented with recent research reports on health literacy, health education booklets and pamphlets from oncology clinics, actual medication labels, clinical appointment cards, health insurance forms, and patient education information from the National Cancer Institute and American Cancer Society websites. The research team, consisting of six Cancer Health Literacy Study members, examined the materials and each independently wrote 25 test items with correct/incorrect responses representative of the cancer health literacy construct to ensure a broad content coverage. The research team met five times to review and revise the list of potential test items. The initial list of 112 items was pilot tested using cognitive interviews with 25 patients diagnosed with cancer. The usability testing of touch-screen devices was also a part of the pilot administration with 25 patients.
Items identified in the cognitive interviews as redundant, unclear or marginally related to cancer health literacy were eliminated, resulting in a list of 76 items for the full administration of the test. Medical records and fliers posted in oncology clinics were used to recruit participants. Following physician permission to contact the patient and preliminary eligibility determination, a recruitment letter was mailed explaining the study with an opt-out toll-free phone number. Of 2,199 contact attempts by surface mail, the research team was unable reach 226 patients, 656 stated no interest in participating, and 1,313 consented to the study. Touchscreen devices were used to administer the test items. The device also read each question aloud to ensure that the measurement of cancer health literacy is not limited to written materials. Data from seven participants were excluded from the analysis due to computer malfunction or patient ineligibility. Participants were compensated $25 for their time and effort. In addition, 98 consenting participants took a 2-week retest (M = 13 days; range = 7–17) and another 60 participants took a 6-month retest (M = 180 days; range = 161–190).
Statistical Analysis
The quantitative phase of the study involved two steps. In Step 1, interim analyses were conducted to assess scale dimensionality and reduce the test length by eliminating poorly performing items. Responses to 76 items were obtained from 1,306 participants. Interim analyses included exploratory factor analysis (Mulaik, 2009) with one- to eight-factor solutions examined, percentage of correct item responses, item-corrected total correlations, gender and race/ethnicity differences in item responses, and content coverage analysis (Lord & Novick, 1968). The resultant 30 items (CHLT-30) were subsequently used once the data collection was completed.
In Step 2 of the quantitative phase, a one-factor model was used to represent the dimensional measurement structure of the CHLT-30. Diagonally weighted least squares estimator was used to take into account binary item responses. Model fit was evaluated with the chi-square test, root mean square error of approximations (RMSEA), comparative fit index (CFI), and Tucker-Lewis index (TLI) using Hu and Bentler’s criteria (Hu & Bentler, 1999). Gender- and race/ethnicity-specific models were also tested. A two-parameter logistic (2-PL) item response theory model (Embretson & Reise, 2000) was used to estimate the item difficulty and discrimination parameters. From the 2-PL, item information curves were obtained to identify a small set of items that contain the largest amount of information on cancer health literacy. Coefficient alpha (Cronbach, 1951), omega (McDonald, 1999), and 2- and 6-month test–retest correlations were used to estimate various forms of scale reliability. Multigroup confirmatory factor analysis was used to test measurement invariance (or item/test bias) between gender and race/ethnic groups followed by group difference tests in latent means (Joreskog, 1971; Millsap, 2011) using chisquare difference test and differences in RMSEA, CFI, and TLI. Structural equation modeling (Bollen, 1989) was used to predict self-confidence about engaging in health decisions from the CHLT-30 scores.
As a subset of the CHLT-30 items, the six most informative items from the 2-PL model were used in a latent class model to identify individuals with limited cancer health literacy. Pearson chi-square test, likelihood ratio chi-square test, entropy, and average latent class probabilities for the most likely latent class membership by latent classes were used to evaluate the quality of latent class solution (Collins & Lanza, 2010; Rupp, Templin, & Henson, 2010). Unconditional latent class probabilities were used to estimate the prevalence of limited cancer health literacy. The three-step procedure (Asparouhov & Muthén, 2014) was used to predict latent class membership from a set of covariates simultaneously by taking into account classification error in the external validation of the CHLT-6. Last, multigroup latent class analysis (Kankaras, Moors, & Vermunt, 2011) was used to test measurement invariance of the CHLT-6 between gender and race/ethnic groups to assess test bias. Mplus 7 (Muthén & Muthén, 1998–2012) was used for factor analysis, 2-PL, latent class analysis, measurement invariance tests, structural equation modeling, and latent mean difference tests. All other analyses were performed using IBM SPSS 19 (Norusis, 2012).
Results
CHLT-30
A one-factor model provided a good fit to the CHLT-30 data (χ2[405] = 542.57, p < .001; RMSEA = .016; CFI = .990; TLI = .989) supporting the unidimensional representation of cancer health literacy as a latent variable. As listed in Table 2, gender and race/ethnicity specific model fit indices also supported a unidimensional measurement model for the CHLT-30. Test items are provided in the Appendix. Parameter estimates from unidimensional latent variable models and abbreviated item descriptions appear in Table 3. Standardized factor loadings were all significant (p < .001) and large (range = .44 to .81; M = .63; median = .62) indicating a strong relationship between the item responses and continuous cancer health literacy latent variable and high scale precision. These results were corroborated with significant (p < .001) and large discrimination parameters from the 2-PL model (M = .84; median = .79; range = .49 to 1.36), as well as moderate to high item-corrected total correlations (M = .42; median = .42; range = .31 to .54). The percent correct item responses were high (M = .81; median = .84; range = .56 to .93) and the item difficulty parameter estimates from the 2-PL model were all negative (p < .001; M = −1.43; median = −1.53; range = −2.13 to −0.36) indicating that the items are relatively easy to answer. Easy items capture nuanced differences toward the low ends of cancer health literacy continuum where the test scores matter most during clinical encounters.
Table 2.
Model fit for the CHLT-30, by gender and race/ethnicity groups
| Sample | n | χ2 | df | p | RMSEA | 90% CI | CFI | TLI |
|---|---|---|---|---|---|---|---|---|
| Male | 590 | 446.68 | 405 | .075 | .013 | 0 to .020. | 993 | .993 |
| Female | 716 | 487.11 | 405 | .005 | .017 | .010 to .022 | .986 | .985 |
| Black | 492 | 505.59 | 405 | <.001 | .022 | .015 to .029 | .968 | .966 |
| White | 806 | 441.73 | 405 | .101 | .011 | 0 to .017 | .981 | .980 |
Note. CHLT-30 = 30-item Cancer Health Literacy Test; RMSEA = root mean square error of approximation; CFI = comparative fit index; TLI = Tucker-Lewis index.
Table 3.
Item parameters for the CHLT-30
| Item | Correct (%) |
Item-correlated total r |
Factor loading |
Difficulty | Discrimination | |
|---|---|---|---|---|---|---|
| 1. | High calorie | 56 | 0.31 | 0.44 | –0.36 | 0.49 |
| 2. | Next pill | 90 | 0.45 | 0.72 | –1.81 | 1.03 |
| 3. | Chemotherapy | 88 | 0.36 | 0.56 | –2.05 | 0.68 |
| 4. | Hemoglobin range | 91 | 0.43 | 0.71 | –1.87 | 1.00 |
| 5. | Oral cancer | 71 | 0.41 | 0.57 | –0.97 | 0.70 |
| 6. | Side effects | 84 | 0.35 | 0.54 | –1.86 | 0.64 |
| 7. | Risk of complications | 84 | 0.41 | 0.60 | –1.65 | 0.75 |
| 8. | Palliative care | 70 | 0.34 | 0.48 | –1.08 | 0.54 |
| 9. | Biopsy | 93 | 0.46 | 0.77 | –1.92 | 1.20 |
| 10. | Appointment location | 92 | 0.39 | 0.65 | –2.13 | 0.85 |
| 11. | Body temperature | 71 | 0.44 | 0.61 | –0.90 | 0.78 |
| 12. | Stage 1 cancer | 89 | 0.52 | 0.77 | –1.57 | 1.21 |
| 13. | Direction | 65 | 0.40 | 0.56 | –0.68 | 0.67 |
| 14. | Efficacy | 85 | 0.46 | 0.68 | –1.53 | 0.92 |
| 15. | Tumor spread | 75 | 0.44 | 0.61 | –1.10 | 0.76 |
| 16. | Generic drugs | 83 | 0.42 | 0.61 | –1.54 | 0.76 |
| 17. | Survival rate | 76 | 0.36 | 0.52 | –1.39 | 0.61 |
| 18. | Fasting | 73 | 0.51 | 0.70 | –0.86 | 0.99 |
| 19. | Smoking risk | 76 | 0.46 | 0.64 | –1.09 | 0.84 |
| 20. | Physical therapist | 89 | 0.54 | 0.81 | –1.51 | 1.36 |
| 21. | Inoperable tumor | 88 | 0.49 | 0.74 | –1.56 | 1.09 |
| 22. | High fiber food | 91 | 0.39 | 0.63 | –2.08 | 0.81 |
| 23. | Metastasized | 72 | 0.37 | 0.52 | –1.10 | 0.61 |
| 24. | Benign tumor | 82 | 0.47 | 0.67 | –1.38 | 0.90 |
| 25. | Radiation treatment | 93 | 0.45 | 0.78 | –1.94 | 1.23 |
| 26. | Complication rate | 63 | 0.50 | 0.69 | –0.47 | 0.94 |
| 27. | Double dose | 89 | 0.39 | 0.62 | –2.01 | 0.79 |
| 28. | Book chapter | 87 | 0.40 | 0.62 | –1.80 | 0.79 |
| 29. | Dose time | 62 | 0.36 | 0.51 | –0.59 | 0.59 |
| 30. | Map reading | 90 | 0.37 | 0.61 | –2.10 | 0.76 |
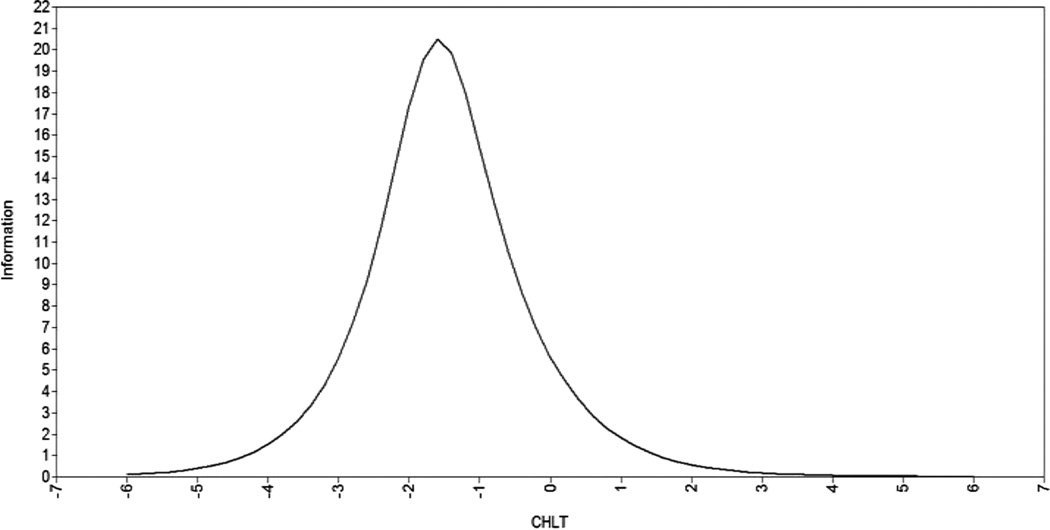
The CHLT-30 has Cronbach’s alpha internal consistency reliability of .88, McDonald’s omega reliability of .89, 2-week test–retest reliability of .90, and 6-month test–retest reliability of .92, all of which are indicative of a highly consistent measure of cancer health literacy. Along the latent cancer health literacy continuum, the precision of measurement is at its peak at approximately 1.5 SD below the mean score, as determined by the test information curve estimated from the 2-PL model (see Figure 1). This is the region of highest measurement fidelity and also is likely the most helpful in clinical settings when interacting with patients with limited cancer health literacy. The measurement invariance tests were supported between males and females and between Blacks and Whites indicating no gender or racial/ethnic bias in CHLT-30 scores (see Table 4). Results indicated no significant mean difference between men and women (p = .247), but the Black patients’ mean cancer health literacy score was significantly lower than Whites (p < .0001). The mean raw CHLT-30 scores were 23.97 (SD = 5.61), 24.26 (SD = 5.19), 20.04 (SD = 5.58), and 26.61 (SD = 3.38) for men, women, non-Hispanic Blacks, and non-Hispanic Whites, respectively.
Figure 1.
CHLT-30: test information curve from the two-parameter logistic model. CHLT-30 = 30-item Cancer Health Literacy Test.
Table 4.
Measurement invariance tests for the CHLT-30 between gender and race=ethnicity groups
| Group | Invariance test | |||
|---|---|---|---|---|
| Fit index | Configural | Scalar | Difference test | |
| Male versus female | χ2(df) | 933.96 (810) | 1004.05 (838) | 62.52 (28) |
| p | <.005 | <.0001 | <.005 | |
| RMSEA | .017 | .017 | .002 | |
| 90% CI | .010 to .020 | .013 to .021 | ||
| CFI | .990 | .987 | .003 | |
| TLI | .989 | .986 | .003 | |
| White versus Black | χ2(df) | 938.81 (810) | 966.37 (838) | 38.21 (28) |
| p | <.005 | <.005 | <.095 | |
| RMSEA | .016 | .015 | .001 | |
| 90% CI | .010 to .020 | .010 to .020 | ||
| CFI | .973 | .973 | 0 | |
| TLI | .971 | .972 | .001 | |
Note. CHLT-30=30-item Cancer Health Literacy Test.
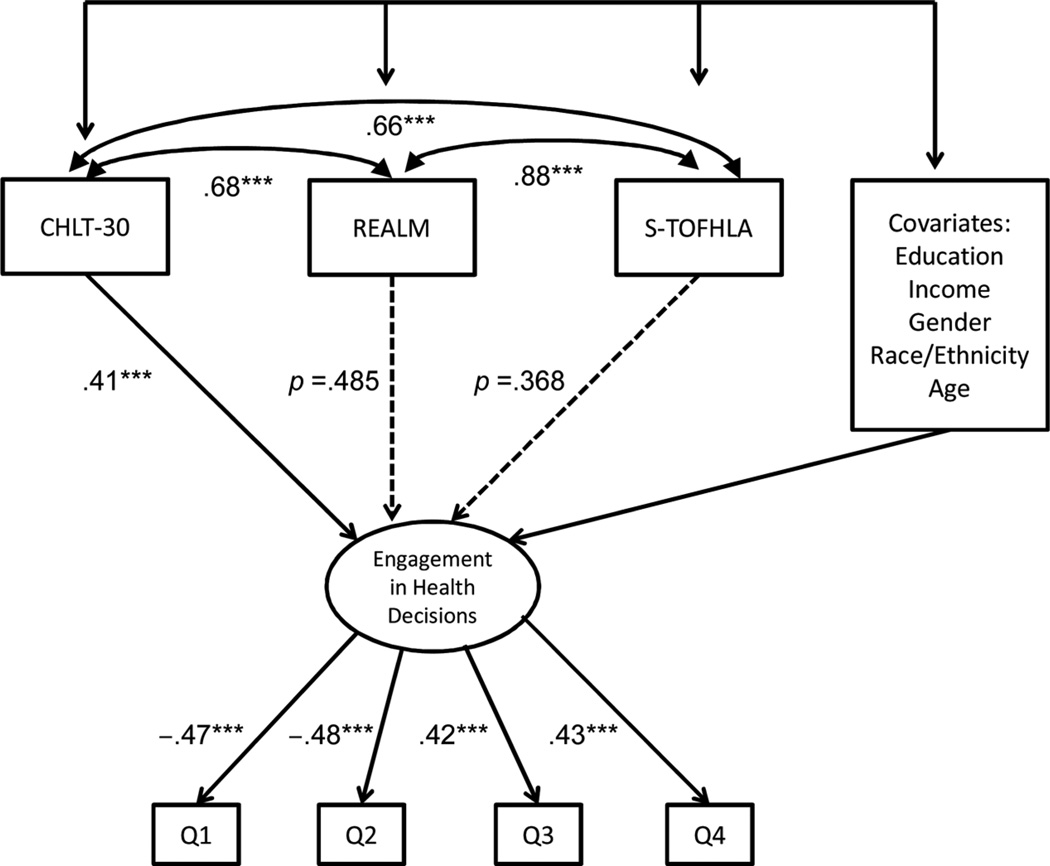
We used structural equation modeling to externally validate the CHLT-30 scores by determining the extent to which scores predicted self-confidence about engaging in health decisions after adjustment for covariates including demographic information (gender, race/ethnicity, income, education, and age) and two measures of health literacy (REALM and S-TOFHLA). In structural equation modeling, the self-confidence about engaging in health decisions was specified as a latent variable measured by two positively and two negatively worded items on a 4-point response format (see Table 5 for item descriptions). This measure was developed as a part of the Cancer Health Literacy Study. As depicted in Figure 2, the CHLT-30 was a significant predictor of the outcome (p < .001). The standardized path coefficient was moderately high (β = .41) linking the new instrument to health decisions as envisioned by the Institute of Medicine’s definition of health literacy. Neither the REALM nor S-TOFHLA was a significant predictor of self-confidence about engaging in health decisions in this model. Correlations between health literacy measures and covariates estimated from the structural equation modeling are presented in Table 6.
Table 5.
Self-confidence about engaging in health decisions
| Test item | |
|---|---|
| 1. | I would offend my doctor if I were to make my own decision(s). |
| 2. | I don’t know enough to make my own medical decisions. |
| 3. | I’d rather be given many choices about what’s best for my health than have the doctor make the decision for me. |
| 4. | Sometimes, there are good reasons not to follow the advice of a doctor. |
Note. Responses were reported on a 4-point scale ranging from 1 (strongly disagree) to 4 (strongly agree).
Figure 2.
CHLT-30: External validation with Self-Confidence about Engaging in Health Decisions as outcome. ***p < .001; for nonsignificant path coefficients, the actual p values are shown; standardized coefficients are shown; Itemdescriptions of Self-Confidence about Engaging in Health Decision construct are listed in Table 5; correlations between health literacy scores and covariates estimated from the structural equation modeling are given in Table 6. CHLT-30 = 30-item Cancer Health Literacy Test; REALM = Rapid Estimate of Adult Literacy in Medicine; S-TOFHLA = short form of the Test of Functional Health Literacy in Adults.
Table 6.
Correlations between health literacy scores and covariates estimated from structural equation modeling
| Covariate | Health Literacy Scale | ||
|---|---|---|---|
| CHLT-30 | REALM | S-TOFHLA | |
| Education | .64 | .52 | .46 |
| Income | .40 | .28 | .24 |
| Gender (0=male; 1=female) | .02* | .09 | .09 |
| Race=ethnicity (0=White; 1=Black) | −.60 | −.43 | −.35 |
| Age | −.02* | −.03* | −.06* |
Note. All correlation coefficients are significant (p<.01), unless marked with an asterisk.
CHLT-30= 30-item Cancer Health Literacy Test; REALM=Rapid Estimate of Adult Literacy in Medicine; S-TOFHLA=short form of the Test of Functional Health Literacy in Adults.
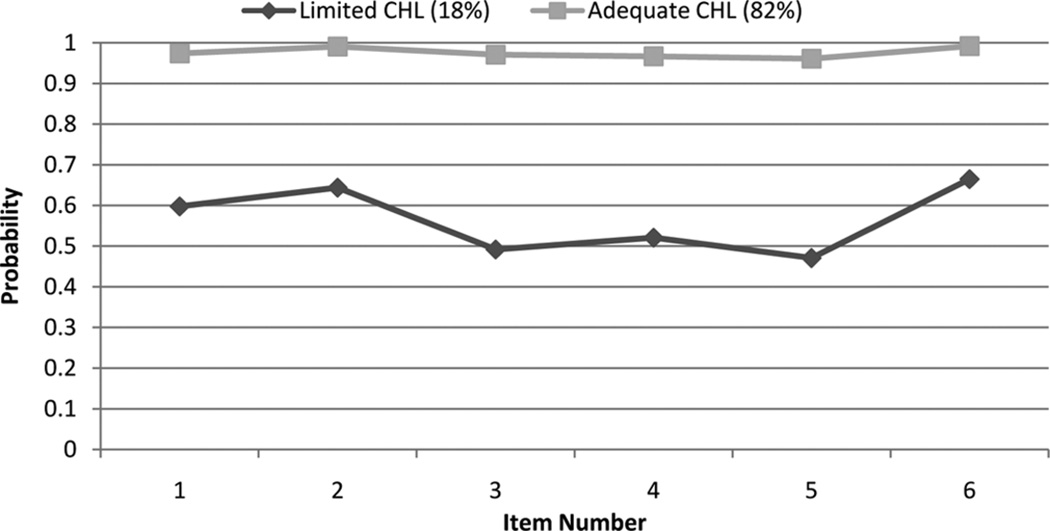
CHLT-6
A two-class solution from the latent class analysis provided the most adequate representation of the CHLT-6 data (Pearson χ2[50] = 84.76; p = .002; likelihood ratio χ2[50] = 82.22; p = .003) supporting the two-group classification of patients in terms of their cancer health literacy (see Table 7 for gender- and race/ethnicity-specific model fit indices). Results from the two-class solution are depicted in Figure 3. In the first class, the probability of correct responses was very high (range = .96 to .99) for all six items. This subgroup of patients was labeled adequate cancer health literacy comprising 82% of cancer patients in this study. In the second class, the probabilities for correct item responses were close to chance levels (range = . 49 to .67). Consequently, this group was labeled limited cancer health literacy comprising 18% of the patients. Large differences in the probability of correct responses to the 6 items between adequate and limited cancer health literacy classes, coupled with a high entropy index score of .827, indicated that the CHLT-6 separates patients with limited cancer health literacy from those with adequate cancer health literacy with a high degree of precision. The CHLT-6 items are provided in Table 8.
Table 7.
Model fit statistic for the CHLT-6, by gender and race/ethnicity groups
| Sample | Pearson’s χ2 | df | p | LRT χ2 | df | p | Entropy |
|---|---|---|---|---|---|---|---|
| Male | 37.11 | 50 | .912 | 43.28 | 50 | .738 | .824 |
| Female | 85.86 | 50 | .001 | 79.84 | 50 | .005 | .836 |
| White | 65.32 | 50 | .072 | 50.57 | 50 | .451 | .874 |
| Black | 79.71 | 50 | .005 | 76.17 | 50 | .010 | .691 |
Note. CHLT-6 = six-item Cancer Health Literacy Test; LRT = likelihood ratio test.
Figure 3.
CHLT-6: Parameter estimates from the two-class solution. CHLT-6 = six-item Cancer Health Literacy Test.
Table 8.
CHLT-6 test items
| Item | Response format |
|---|---|
| 1. The normal range for hemoglobin for a male is 13.3–17.2 g/dl. Joe’s hemoglobin is 9.7 g/dl. Is Joe within the normal range? |
|
| 2. A biopsy of a tumor is done to … |
|
| 3. If a patient has stage 1 cancer, it means the cancer is … |
|
| 4. The role of a physical therapist is to talk to a patient about emotional needs. |
|
| 5. A tumor is considered “inoperable” when it cannot be treated with … |
|
| 6. Sally will get radiation therapy once a day, Monday through Friday. If Sally has therapy for 4 weeks, how many times will she get radiation therapy? |
|
Note. Correct responses appear in boldface. CHLT-6 = six-item Cancer Health Literacy Test.
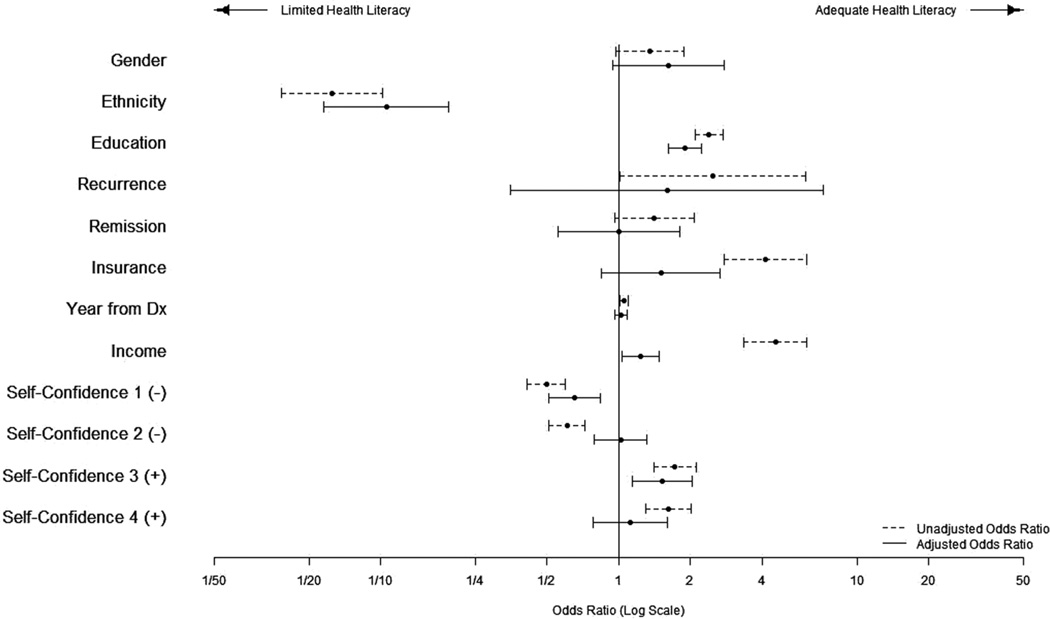
Data from 1,306 cancer patients showed that the average probability of belonging to the limited cancer health literacy class is .95 and that the average probability of belonging to the adequate cancer health literacy class is .96. Relative to the probability of 1.0, as one expects from a hypothetical gold standard, the accuracy of CHLT-6 is extremely high. In testing gender and race/ethnic bias in CHLT-6 scores, multigroup latent class analysis was used by comparing models with and without between-group equality constraints on conditional probabilities. Results supported the measurement invariance in both gender and race/ethnic groups providing evidence that the prevalence estimates are free from gender and racial/ethnic bias. Measurement invariance test statistics are provided in Table 9. Using the three-step procedure (Asparouhov & Muthen, 2013) to account for classification error, the latent class variable was regressed on a set of predictors one at a time and simultaneously resulting in unadjusted and adjusted odds ratios, respectively (see Figure 4). In this external validity analysis, unadjusted odds ratios indicated that, relative to individuals with adequate cancer health literacy, individuals with limited cancer health literacy are likely to be Black, undereducated, low income, insured by state/federal government (compared with private insurance), and tend not to engage in health decisions. When all covariate effects were estimated simultaneously, race/ethnicity, education, income and two out of four health decision variables remained significant predictors of the binary latent class variable.
Table 9.
Measurement invariance test for the CHLT-6
| Sample | Pearson’s χ2 | df | p | LRT χ2 | df | p | Entropy |
|---|---|---|---|---|---|---|---|
| Male versus female | 122.97 | 100 | .059 | 123.11 | 100 | .058 | .915 |
| White versus Black | 145.03 | 100 | .002 | 126.75 | 100 | .037 | .902 |
Note. CHLT-6 = six-item Cancer Health Literacy Test; LRT = likelihood ratio test.
Figure 4.
CHLT-6: External validation. CHLT-6 = six-item Cancer Health Literacy Test.
Discussion
As emphasized in the Affordable Care Act of 2010, patients are expected to successfully engage in their health care (Koh, Brach, Harris, & Parchman, 2013). For example, they should be able to adhere to their medication regimens, distinguish scientifically credible medical evidence from misconceptions and myths, and effectively communicate with their providers on issues such as success rate of chemotherapy and 5-year survival rates following a surgery. Patients with limited cancer health literacy commonly struggle with these and other issues related to health care. The expectation of patients’ engagement in health care decisions by their health care providers likely increases the burden that cancer patients are already experiencing following a life-changing diagnosis.
In this study, we found, for example, that 23% of Black and 3% of White cancer patients believe that rather than taking a pill twice a day as prescribed, taking it three times a day will help them get better faster; 19% of Blacks and 5% of Whites cannot follow a map to find their way around on a hospital floor; 44% of Blacks and 14% of Whites believe that exposing a tumor to air during surgery causes the tumor to spread; and 61% of Blacks and 23% of Whites have difficulty answering the following arithmetic question: ‘‘Of 100 people receiving treatment, half are expected to respond to the treatment. Of those who respond, half are expected to have complications. How many people who respond to treatment are expected to have complications?’’ Patients with limited cancer health literacy, a group of individuals comprising 18% of cancer patients in our study, show striking similarities to patients with heart failure in terms of the limited health literacy rate of 18% and low educational attainment as reported in a recent study by Peterson and colleagues (2011). Among patients with heart failure, the researchers also linked individuals with limited health literacy to an increased rate of all-cause mortality. With the availability of cancer specific health literacy instruments reported in the Cancer Health Literacy Study, the links between health literacy and mortality need to be examined for cancer patients in future studies.
The CHLT-30 is designed to measure cancer health literacy along a continuum. Accurate measurements of theoretical constructs such as cancer health literacy allow researchers to estimate treatment effect in intervention studies, assess change over time, and establish relationships with theoretically relevant factors and clinically important outcomes (e.g., morbidity, mortality). The instrument has a broad content coverage, very high reliability, and is strongly linked to self-confidence about engaging in health decisions. The CHLT-30 is easy to administer and takes approximately 10–15 minutes. The test score is obtained by the total number of correct responses and ranges from 0 to 30.
The CHLT-6 is designed to quickly identify individuals with limited cancer health literacy. It has invariant measurement properties between gender and race/ethnic groups, and is externally validated. These features make the CHLT-6 attractive for adoption in a variety of settings in which patients with cancer are treated and particularly in oncology clinics and pharmacies. The CHLT-6 takes less than 2 minutes to administer and score. The computerized test scoring yields two probabilities: (a) the probability of belonging to the limited cancer health literacy class and (b) the probability of belonging to the adequate cancer health literacy class. Two probabilities sum up to unity, by definition.
Is health literacy an ability, a skill, or is it knowledge? In developing the CHLT-30 and CHLT-6, we adopted an ability definition of health literacy. Consequently, our test items include knowledge and skills, as well as items that require synthesizing knowledge and skills. A strong support for the unidimensional representation of cancer health literacy that we report in this study indicates that knowledge, skill, and their synthesis are highly correlated.
Our study has some limitations. The sample was large and covered cancer patients with various demographic characteristics, but it included only non-Hispanic Black and White cancer patients and may not generalize to other racial/ethnic groups. Evidence suggests, for example, that Hispanics have the highest rates of limited health literacy (Sentell, 2012). Translation of the CHLT-30 and CHLT-6 into Spanish followed by measurement invariance studies are needed to justify using these instruments in Hispanic populations. Also, we used self-confidence about engaging in health decisions in external validation studies. Actual health decisions made by patients should be used in future studies to externally validate health literacy measures. Last, four items in our health decision measure were balanced as positive and negative wordings to avoid response bias. However, negatively worded items could be problematic to participants. We note that we conducted extensive item testing and both negatively worded and positively worded items were supported in this testing.
In conclusion, both the CHLT-30 and CHLT-6 have very strong psychometric properties and are free of gender and racial/ethnic bias in the context of this study. Given the financial constraints in the health care system and competing demands for physicians’ time and attention, the new instruments can be used efficiently and effectively to identify subpopulations of cancer patients at risk for poor outcomes and for targeted interventions to improve cancer health literacy.
Appendix: 30-item Cancer Health Literacy Test (CHLT-30)
-
1)Doctors often recommend high calorie and high protein foods for cancer patients in treatment. Which is the highest in calories and protein?
- French fries
- Cheeseburger
- Hard-boiled egg
-
2)
Shirley took two Lorazepam at 2 p.m. What time can she take the next dose?
- 6 p.m.
- 7 p.m.
- 8 p.m.
-
3)
Adjuvant therapy is cancer treatment generally given after a tumor is removed. Neo-adjuvant therapy is cancer treatment generally given to shrink a tumor before surgery.
Mr. Davis has had his tumor surgically removed. After his surgery, he will get chemotherapy. The chemotherapy is:- Neo-adjuvant
- Adjuvant
-
4)The normal range for hemoglobin for a male is 13.3–17.2 g/dl. Joe’s hemoglobin is 9.7 g/dl. Is Joe within the normal range?
- Yes
- No
-
5)In people who develop oral cancers, 25% of these cases occur in the tongue. Oral cancer occurs in the tongue:
- 1 out of every 25 cases
- 25 out of every 100 cases
- 25 out of every 1000 cases
-
6)
Possible side effects of Tamoxifen:
More than 30% of patients experience- Hot flashes
- Swelling
- Vaginal discharge
- Loss of libido
10% to 29% of patients experience- Nausea
- Menstrual irregularities
- Mood changes
- Weight loss
Which side effect is more common for patients taking Tamoxifen?- Swelling
- Weight Loss
-
7)Chemotherapy treatment A has a 92% success rate and a long-term complication rate of 15.5%. Treatment B has a 95.9% success rate and a long-term complication rate of 3.8%. Which treatment has a lower risk of long-term complications?
- Treatment A
- Treatment B
-
8)The purpose of palliative care is to cure cancer.
- True
- False
-
9)A biopsy of a tumor is done to:
- Remove it
- Diagnose it
- Treat it
-
10)
Above is Maria’s appointment card. Where should Maria go for her appointment?
- Purple Clinic
- Yellow Clinic
- Green Hospital
-
11)Fever classifications:
- None to mild: temperature is 98.6°F to 100.4°F
- Moderate: temperature is 100.5°F to 104°F**
- Severe: temperature is greater than 104°F**
(**Call your doctor right away if you experience this.)
Pete has a temperature of 100.3°F. According to the chart, should he call his doctor?- Yes
- No
-
12)If a patient has stage 1 cancer, it means the cancer is:
- Localized
- In nearby organs
- In distant sites
-
13)
Ms. Rivera needs directions to get to her first appointment. The receptionist tells her to walk to the end of the hall and take a right turn, the first left turn, and then go to the first door on the left. If Ms. Rivera follows these directions, where will she end up?
- Dr. Lee’s Office
- Dr. Marley’s Office
- Dr. Adams’ Office
-
14)The degree to which a drug can have a beneficial effect is called:
- Impotency
- Efficacy
- Dexterity
-
15)Exposing a tumor to air during surgery causes the tumor to spread.
- True
- False
-
16)Brand name drugs have the same active ingredients as generic drugs with a little extra that makes them better.
- True
- False
-
17)The overall five-year survival rate for prostate cancer is 98%. This means that five years after treatment, 98% of prostate cancer patients will be expected to:
- Be alive
- Be cancer-free
- Die
-
18)An appointment card says not to eat or drink anything 9 hours prior to the appointment. Sally has an appointment at 11:15 a.m. on Friday. What time should she stop eating or drinking?
- Thursday at 11:15 p.m.
- Friday at 1:15 a.m.
- Friday at 2:15 a.m.
-
19)Scientists estimate that smoking is responsible for 85% to 90% of lung cancer deaths. This means that 85% to 90% of smokers will get lung cancer.
- True
- False
-
20)The role of a physical therapist is to talk to a patient about emotional needs.
- True
- False
-
21)A tumor is considered “inoperable” when it cannot be treated with:
- Radiation Therapy
- Surgery
- Chemotherapy
-
22)When receiving radiation, patients should eat foods that are high in fiber and avoid eating foods containing lots of spices, caffeine or dairy products. Which of the following foods is best to eat when receiving radiation?
- Curry
- Ice cream
- Bananas
-
24)When a cancer has metastasized it means it has:
- Spread to other parts of the body
- Spread to other parts of the originally affected organ
- Stopped spreading
-
25)A benign tumor is cancerous.
- True
- False
-
26)Sally will get radiation therapy once a day, Monday through Friday. If Sally has therapy for 4 weeks, how many times will she get radiation therapy?
- 5
- 15
- 20
-
27)Of 100 people receiving treatment, half are expected to respond to the treatment. Of those who respond, half are expected to have complications. How many people who respond to treatment are expected to have complications?
- 25
- 35
- 50
-
28)If patients get better by taking Medicine B twice a day, then if they take Medicine B 3 times a day, patients will get better faster.
- True
- False
-
29)
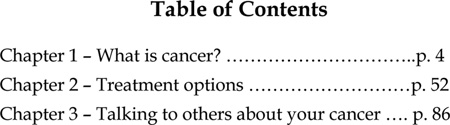
If Ms. Liu wants to learn more about the side effects of radiation, which chapter is most likely to have this information?
Chapter 1
Chapter 2
Chapter 3
-
30)Mrs. Bell takes her first pill at 10:00 a.m. If she takes this medicine every 4 hours, when would she need to take her third pill?
- 2:00pm
- 4:00 p.m.
- 6:00 pm
-
31)
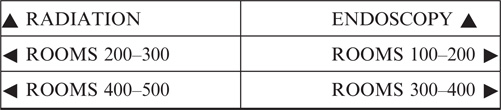 If Mr. Anthon needs to meet his doctor in room202, which direction should he go?
If Mr. Anthon needs to meet his doctor in room202, which direction should he go?- Straight ahead
- Right
- Left
Footnotes
Publisher's Disclaimer: Taylor & Francis makes every effort to ensure the accuracy of all the information (the “Content”) contained in the publications on our platform. However, Taylor & Francis, our agents, and our licensors make no representations or warranties whatsoever as to the accuracy, completeness, or suitability for any purpose of the Content. Any opinions and views expressed in this publication are the opinions and views of the authors, and are not the views of or endorsed by Taylor & Francis. The accuracy of the Content should not be relied upon and should be independently verified with primary sources of information. Taylor and Francis shall not be liable for any losses, actions, claims, proceedings, demands, costs, expenses, damages, and other liabilities whatsoever or howsoever caused arising directly or indirectly in connection with, in relation to or arising out of the use of the Content.
This article may be used for research, teaching, and private study purposes. Any substantial or systematic reproduction, redistribution, reselling, loan, sub-licensing, systematic supply, or distribution in any form to anyone is expressly forbidden. Terms & Conditions of access and use can be found at http://www.tandfonline.com/page/terms-and-conditions
Contributor Information
Levent Dumenci, Department of Social and Behavioral Health, Virginia Commonwealth University, Richmond, Virginia, USA.
Robin Matsuyama, Department of Social and Behavioral Health, Virginia Commonwealth University, Richmond, Virginia, USA.
Daniel L. Riddle, Department of Physical Therapy, Virginia Commonwealth University, Richmond, Virginia, USA
Laura A. Cartwright, Department of Social and Behavioral Health, Virginia Commonwealth University, Richmond, Virginia, USA
Robert A. Perera, Department of Biostatistics, Virginia Commonwealth University, Richmond, Virginia, USA
Harold Chung, Department of Internal Medicine, Virginia Commonwealth University, Richmond, Virginia, USA.
Laura A. Siminoff, College of Health Professions and Social Work, Temple University, Philadelphia, Pennsylvania, USA
References
- Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling. 2014;21:329–341. [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York, NY: Wiley; 1989. [Google Scholar]
- Cartwright LA, Dumenci L, Siminoff LA, Matsuyama RK. Cancer patient’s understanding of prognostic information. Journal of Cancer Education. 2014 doi: 10.1007/s13187-013-0603-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Lanza ST. Latent class and latent transition analysis with applications in the social, behavioral, and health sciences. Hoboken, NJ: Wiley; 2010. [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, Bairnsfather LE. Rapid assessment of literacy levels of adult primary care patients. Family Medicine. 1991;23:433–435. [PubMed] [Google Scholar]
- DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Baker DW. Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumenci L. The Psychometric Latent Agreement Model (PLAM) for discrete latent variables measured by multiple items. Organizational Research Methods. 2011;14:91–115. doi: 10.1177/1094428110374649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumenci L, Matsuyama RK, Kuhn L, Perera RA, Siminoff LA. On the validity of the Rapid Estimate of Adult Literacy in Medicine (REALM) scale as a measure of health literacy. Communication Methods and Measures. 2013;7:134–143. doi: 10.1080/19312458.2013.789839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embretson SA, Reise SP. Item response theory for psychologists. Mahwah, NJ: LEA; 2000. [Google Scholar]
- Goodman LA. Exploratory latent structure analysis using both identifiable and unidentifiable models. Biometrika. 1974;61:215–231. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Joreskog KG. A general approach to confirmatory maximum likelihood factor analysis. Psychometrika. 1969;34:183–201. [Google Scholar]
- Joreskog KG. Simultaneous factor analysis in several populations. Psychometrika. 1971;36:409–426. [Google Scholar]
- Kankaras M, Moors G, Vermunt JK. Testing for measurement invariance with latent class analysis. In: Davidov E, Schmidt P, Billiet J, editors. Cross-cultural analysis: Methods and application. New York, NY: Taylor & Frances; 2011. pp. 359–384. [Google Scholar]
- Katz SJ, Belkora J, Elwyn G. Shared decision making for treatment of cancer: Challenges and opportunities. Journal of Oncology Practice. 2014;10:206–208. doi: 10.1200/JOP.2014.001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh HK, Brach C, Harris LM, Parchman ML. A proposed “health literate care model” would constitute a systems approach to improving patients’ engagement in care. Health Affairs. 2013;32:357–367. doi: 10.1377/hlthaff.2012.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord FM, Novick MR. Statistical theories of mental test scores. Reading, MA: Addison-Wesley; 1968. [Google Scholar]
- McDonald RP. Test theory: A unified treatment. Mahwah, NJ: LEA; 1999. [Google Scholar]
- Millsap RE. Statistical approaches to measurement invariance. New York, NY: Taylor & Francis; 2011. [Google Scholar]
- Mulaik SA. Foundations of factor analysis. 2nd ed. Boca Raton, FL: Chapman & Hall=CRC; 2009. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6th ed. Los Angeles, CA: Author; 1998–2012. [Google Scholar]
- Norusis MJ. IBM SPSS statistics 19 statistical procedure companion. Upper Saddle River, NJ: Prentice Hall; 2012. [Google Scholar]
- Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. American Journal of Health Behavior. 2007;31:S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: A new instrument measuring patients’ literacy skills. Journal of General Internal Medicine. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Masuidi FA. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305:1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pleasant A. Measuring health literacy: A challenge to curriculum design and evaluation. 2009 Retrieved from http://www.centreforliteracy.qc.ca/publications/briefs/measuring/measuring.pdf. [Google Scholar]
- Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan SC, Parker RM, editors. National Library of Medicine current bibliographies in medicine: Health literacy. Bethesda, MD: National Institutes of Health U.S. Department of Health and Human Services; 2000. NLM Pub. No. CBM 2000–1. [Google Scholar]
- Rindskopf D, Rindskopf W. The value of latent class analysis in medical diagnosis. Statistics in Medicine. 1986;5:21–27. doi: 10.1002/sim.4780050105. [DOI] [PubMed] [Google Scholar]
- Ritchie J. Qualitative research practice: A guide for social science students and researchers. London, England: Sage; 2003. [Google Scholar]
- Rupp AA, Templin J, Henson RA. Diagnostic measurement: Theory, method, and application. New York, NY: Guilford Press; 2010. [Google Scholar]
- Sentell T. Implications for reform: Survey of California adults suggests low health literacy predicts likelihood of being uninsured. Health Affairs. 2012;31:1039–1048. doi: 10.1377/hlthaff.2011.0954. [DOI] [PubMed] [Google Scholar]
- Thome S, Oliffe JL, Stajduhar KI. Communicating shared decision-making: Cancer patient perspective. Patient Education and Counseling. 2013;90:291–296. doi: 10.1016/j.pec.2012.02.018. [DOI] [PubMed] [Google Scholar]
- Walter CL, Covinsky KE. Cancer screening in elderly patients: A framework for individualized decision making. JAMA. 2001;285:2750–2756. doi: 10.1001/jama.285.21.2750. [DOI] [PubMed] [Google Scholar]