Summary
Background
Patient portal adoption has rapidly increased over the last decade. Most patient portal research has been done in primary care or medical specialties, and few studies have examined their use in surgical patients or for recruiting research subjects. No known studies have compared portal messaging with other approaches of recruitment.
Objectives
This case report describes our experience with patient portal versus telephone recruitment for a study involving long-term follow up of surgical patients.
Methods
Participants were recruited for a study of recurrence after ventral hernia repair through telephone calls and patient portal messaging based on registration status with the portal. Potential subjects who did not have a portal account or whose portal messages were returned after 5 days were called. The proportion of participants enrolled with each method was determined and demographics of eligible patients, portal users, and participants were compared.
Results
1359 patients were eligible for the hernia study, and enrollment was 35% (n=465). Most participants were recruited by telephone (84%, n=391); 16% (n=74) were recruited through portal messaging. Forty-four percent of eligible participants had a registered portal account, and 14% of users responded to the recruitment message. Portal users were younger than non-users (55 vs. 58 years, p<0.001); participants recruited through the portal versus telephone were also younger (54 vs. 59 years, p=0.001). Differences in the sex and racial distributions between users and non-users and between portal and telephone recruits were not significant.
Conclusions
Portal versus telephone recruitment for a surgical research study demonstrated modest portal recruitment rates and similar demographics between recruitment methods. Published studies of portal-only recruitment in primary care or medical-specialty patient populations have demonstrated higher enrollment rates, but this case study demonstrates that portal recruitment for research studies in the surgical population is feasible, and it offers convenience to patients and researchers.
Keywords: Patient portal, clinical research, subject recruiting, disparities, health information technologies
Background
Patient portals are online applications that allow patients and their families to interact with a healthcare system [1]. Patient portal adoption has rapidly increased over the last two decades, and use of patient portals has been shown to enhance patient satisfaction [2] and self-efficacy [3], increase adherence to preventative screening recommendations and treatment regimens [4–6], and improve clinical outcomes in chronic diseases such as hypertension [7], diabetes [8, 9], and depression [10].
Most research about patient portals has been done in primary care or medical specialty settings where providers have ongoing relationships with their patients [11]. The few studies that have described the use of a patient portal for research study recruitment have been done in primary care settings, in patients with scheduled appointments, and with a single communication modality (i.e., portal) for recruitment. Simon reported use of a patient portal to recruit 48% of eligible registered portal users from primary care practices for a study of online depression management [10]. Grant and colleagues recruited active patient portal users with diabetes and a visit with a primary care physician within the past year for a study investigating the use of a personal health record in preparing for an upcoming appointment; 37% of eligible participants were enrolled [12]. Leveille and colleagues used a patient portal to recruit patients scheduled for primary care appointments to a study screening for untreated depression, chronic pain, and mobility problems, and 24.7% of eligible patients were recruited [13].
All of these studies recruited only through the patient portal in a population of patients with recent or scheduled interactions with their providers. Little is known about the use of patient portals to facilitate research, especially in acute care specialties such as surgery, which may only interact with patients episodically. Several studies have suggested that users of patient portals are demo-graphically distinct from non-users [14–21], so their use for research recruitment has the potential to introduce biases in the enrolled population.
Objectives
This case report compares the use of patient portal messaging and telephone calls to recruit research participants and to assess long-term surgical outcomes in a study of ventral hernia recurrence. We report study enrollment rates by patient portal and telephone, and we compare the demographics of eligible portal users and non-users and of the groups recruited by portal messaging and by telephone.
Methods
Patient portal usage for surgical research recruitment and follow up was examined in the context of a prospective clinical trial to determine whether a brief patient survey is accurate for the diagnosis of recurrence after ventral hernia repair (VHR), a common procedure performed by surgeons [22]. English-speaking adult patients who underwent elective VHR at Vanderbilt University Medical Center (VUMC), at least 1 year and up to 5 years prior to enrollment, were eligible to participate in the hernia follow-up study. Initial enrollment involved completion of a survey, and patients were recruited by either telephone call or a secure message sent through Vanderbilt’s patient portal, My Health at Vanderbilt (MHAV).
MHAV is a patient portal, established in 2004, with over 274,000 registered users and 2.4 million logins per year. Portal messaging takes place in a closed-loop system integrated with Vanderbilt’s electronic health record and the provider inter-departmental messaging system. MHAV has a bounce-back feature that returns unanswered messages to the sender after 5 days [23]. Several features of MHAV support the security of its communications. MHAV is a Java application which stores data in an Oracle database and has a web-based user interface accessible only through the Hypertext Transfer Protocol Secure (HTTPS) communications protocol. The web component is available outside the institutional firewall, while the web servers and database exist within the firewall and interact only with applications from institutional servers. MHAV may be accessed from computer or smartphone based web-browsers. MHAV users receive email notifications when MHAV messages arrive, but they must log into the secure MHAV application to view the content of the messages.
Patients eligible for the study and registered with MHAV received a MHAV message containing a brief description of the study and a link directing them to an online survey. The message contained information about the study, including the purpose of the study, and contact information allowing patients the opportunity to respond through the portal or telephone with any questions about participation or study procedures. Patients received a telephone call if they did not have a MHAV account or if they did not open the MHAV message after 5 days. During the telephone call, patients received the same information regarding the purpose of the study, study procedures, and contact information. The survey was completed during the telephone call, and the telephone script contained the same text as the online survey. The survey contained only 3 brief questions, in addition to the participant’s name and birthdate. For patients recruited by telephone, up to 3 attempts were made to contact the patient.
We compared the proportions and demographics (i.e., sex, age, and race) of patients recruited through patient portal and by telephone calls, as well as the demographics of eligible MHAV users versus non-users. Comparisons of proportions and means were performed using the chi-squared test or t-test, as appropriate.
Results
There were 1359 patients who underwent VHR within 1 to 5 years of enrollment, and the population was 50% male (n=682). The mean age was 57 ± 13 (SD) years, and the mean time from VHR was 4 ± 1 years. Of these eligible VHR patients, 89% (n=1210) were white, 8% (n=111) black, and 3% (n=38) other or unknown.
Overall, 34% (n=465) of eligible patients completed the survey, with 16% (n=74) recruited through MHAV and 84% (n=391) recruited by telephone. Recruitment by telephone required 2 to 5 minutes per call, depending upon whether the patient agreed to participate and their response to the survey questions. Most eligible participants received an average of 1 to 2 phone calls. MHAV recruitment involved verifying the account and sending the message and took less than 1 minute per patient. Data from surveys conducted by telephone were manually entered into the research database by study personnel whereas data from surveys done online were automatically entered.
▶Figure 1 shows a flow diagram depicting recruitment. The research team called 130 patients before they received institutional approval to recruit via patient portal messaging. Of the remaining 1229 patients, 44% (n=539) had a MHAV account and were sent a message. The mean time since VHR was 47 months for those without a MHAV compared to 45 months for those with a MHAV account (p=0.035). Seven patients responded to the MHAV message directly and stated that they did not wish to participate in the study, and 14% (n=74) completed the survey after receiving the message. Patients who did not open the MHAV message after 5 days received a subsequent telephone call.
Fig. 1.
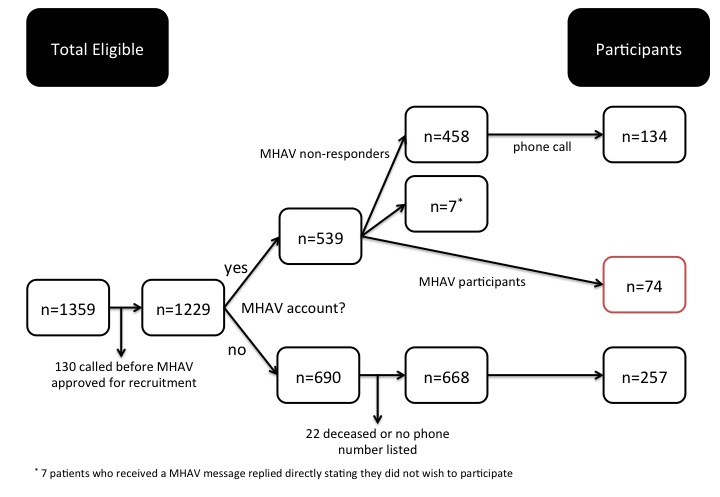
Of the 1359 patients eligible, a total of 465 agreed to participate. There were 74 participants (16%) recruited through the patient portal, and 257 participants (55%) recruited by telephone who did not have access to the patient portal. The remaining 134 participants (29%) were recruited by telephone after not responding to the MHAV message.
In total, 1256 patients (92% of eligible population) received a telephone call, including patients who were called prior to receiving a MHAV message (n=130), patients who did not have a MHAV account (n=690), and those who did not open the MHAV message (n=458). Of the 458 patients who did not open the MHAV message, 29% (n=134) were subsequently recruited by telephone. There were 22 patients from the eligible population who did not receive a telephone call because they were either deceased or had no phone number listed.
The patients with a MHAV account were, on average, 3 years younger than those without an account (58 years vs. 55 years, p<0.001). Of those with a MHAV account, 50% (n=268) were male, and of those without an account, 51% (n=350) were male (p=0.73). The race distributions for the eligible population and for those with and without MHAV accounts are shown in ▶Figure 2. Of patients registered for MHAV, 90% (n=487) were white, 7% (n=39) black, and 2% (n=13) other or unknown. This distribution is similar to those without a MHAV account, with 87% white, 10% black (p=0.13).
Fig. 2.
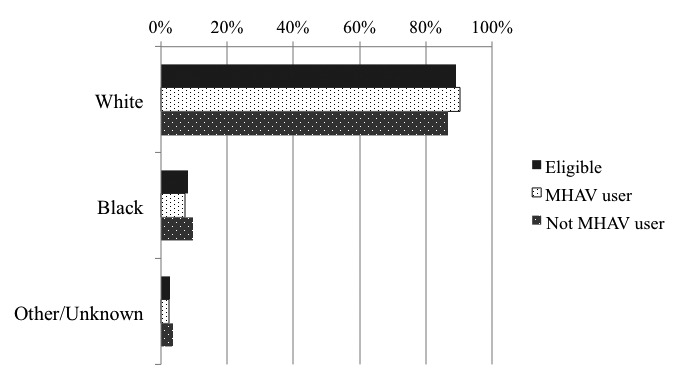
Distribution of Race in Elegible Population by Patient Portal User Status
A summary of patient characteristics for those recruited via telephone compared to those recruited via MHAV can be found in ▶Table 1. Of 465 participants, the percentage of men recruited through MHAV was not significantly different than the percentage of men recruited via telephone, and the difference in race distributions between groups was not significant (▶Figure 3). Patients recruited through the portal were significantly younger than those who were recruited by telephone (54 years vs. 59 years, p=0.001). Finally, patients recruited through telephone calls were further removed from their operation compared to those recruited via MHAV (48 months vs. 43 months, p=0.003).
Table 1.
Demographics of Study Participants. The patients recruited by telephone were slightly older and were further removed from their operations than those recruited through the patient portal. There was no significant difference in race or gender between the two groups.
| Demographics of Participants | Recruited via Telephone (n=391) | Recruited via Patient Portal (n=74) | p-value |
|---|---|---|---|
| Age, mean (SD), yrs | 59.1 (13) | 53.3 (12) | <0.001a |
| – Gender, n (%) | |||
| Male | 204 (52%) | 33 (45%) | 0.232b |
| Female | 187 (48%) | 41 (55%) | |
| Race, n (%) | |||
| White | 357 (91%) | 68 (92%) | 0.426b |
| Black | 26 (7%) | 6 (8%) | |
| Other/Unknown | 8 (2%) | 0 (0%) | |
| Months since VHR, mean (SD) | 48 (12) | 43 (10) | 0.003a |
a t-test;
b chi2; Ventral hernia repair, VHR; Standard deviation (SD)
Fig. 3.
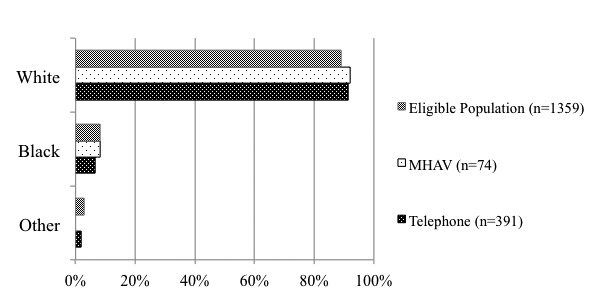
Demographics of Participants by Recruitment Method
Discussion
This case study is one of the first reports to compare research subject recruitment through a patient portal and telephone and to examine portal usage in surgical patients. Research recruitment rates were modest – 16% of all patients recruited and 5% of eligible participants – but some important lessons were learned. The convenience that portal recruitment offers to patients and researchers cannot be discounted, and given that prior reports of recruitment through a portal have not provided a comparison group of patients recruited through alternate methods, this case report offers important, novel information for researchers considering recruitment through a patient portal.
Several studies have reported concerning disparities in age-[14–18], gender-[14–16, 19], and racial-based [14, 15, 17, 19–21] usage of patient portals. In this population of surgery patients who had a history of VHR, we did not observe significant disparities between those with and without portal accounts or those recruited by the portal or telephone. Portal users and participants were slightly younger, but the difference may not be clinically significant. There we no statistically significant differences in race or sex between users and non-users or those patients recruited by the portal versus the telephone. The mean time since VHR was 5 months shorter for the group recruited via MHAV. Additionally, in the eligible patient population, those with a MHAV account were not as far removed from their operation. The reason for this is not known, although it is likely due to increasing patient and provider adoption of the patient portal over time and a more recent interaction with the healthcare system.
Enrollment through the portal was lower in this study than in previous studies reported in the literature [10, 12, 13]. There are several reasons for this difference. First, the pool of recruited patients was expanded by recruitment through alternative communication modalities, unlike nearly all prior studies examining research study enrollment through patient portals, which recruited only through the portal. Second, many of these studies were performed in the primary care population and in patients with already-scheduled appointments. Registered users and patients actively engaged with a healthcare system through upcoming appointments would understandably be more likely to respond to messages through a patient portal. The surgical patient population involved in this study may have only interacted with our healthcare system during an acute episode of care, and thus, been less likely to have registered for or used our patient portal than the primary care or medical populations who may have long-term relationships with their providers. Finally, the bounce-back feature of our portal, which results in an automated, returned message after five days, may have also limited recruitment through the portal. While a five-day limit may be appropriate for urgent clinical issues, a longer time for response may have allowed more patients to be recruited through the portal.
VUMC is in the process of streamlining registration procedures for MHAV; all adult patients providing an email address and proof of identity during check in for clinical care will be emailed a MHAV registration invitation. With an easier registration process and expanded MHAV use base, future research recruitment efforts may prove more effective. One important lesson learned from patients who were later called after not participating through MHAV was that the hyperlink to the survey was not functional in the portal message, meaning that patients needed to manually copy and paste the link into a web browser. This process was not easy or intuitive for some patients. Future recruitment attempts that include instructions or an active link may increase recruitment through MHAV.
Though modest, the 16% enrollment through the portal may still represent a significant gain in the recruitment process. It is unknown whether these same patients would have been successfully recruited by telephone, but we suspect that some participants were gained due to convenience. Of the 74 MHAV participants, 37% completed the survey after 5 pm and before 8 am, when study personnel are typically not able to make telephone calls. There are several additional advantages to using a patient portal for recruitment. For study personnel, the time spent sending a MHAV message was less than the time spent conducting a telephone survey and manually entering the data, particularly if a voicemail was left or phone calls had to be returned. In addition, patients who were not interested in participating could respond directly in an asynchronous fashion and avoid receiving a telephone call.
This attempt to recruit surgical patients for a research study using a patient portal offers several important lessons. First, portal policies and functions developed for clinical care, such as a prompt messaging bounce-back feature, may need to be modified as portal adoption increases and portals are used for purposes such as research. Second, healthcare providers may want to broaden their thinking in encouraging acute-care patients to register for patient portals, as the portals can offer a convenient way to conduct online follow up and to assess long-term outcomes. Such forward-thinking behavior could be discouraged in acute-care and specialty providers if Meaningful Use requirements mandate frequent interaction with registered portal users. Finally, physicians using patient portals for research recruitment should be aware of how the demographic distribution of portal users may bias a study. While only minor disparities in age were observed in our experience, our eligible population was predominately middle-aged and White. The generalizability to the population as a whole is unknown since we were unable to evaluate recruitment in minority populations, and the potential for bias in other studies may be significant. Additionally, consideration will also need to be given to the study procedures involved during recruitment. In this case, recruitment involved a 3-question survey. The online survey was brief, and this could easily be read in a telephone script. Given the influence that survey administration can have upon results, this factor must be taken into account during study designs utilizing patient portals for recruitment.
Conclusions
Patient portals offer a novel and efficient method to recruit patients for research studies. Rates of recruitment in surgical or acute-care patients may not be as high as those seen in medical specialties due to a lack of registered portal users. Potential demographic biases in the study should be considered carefully. Portal operational policies may need to be revised as portals are adopted for functions other than clinical care.
Footnotes
Clinical Relevance Statement
Patient portals offer an efficient method to recruit patients for research studies in the surgical or acute-care population. Researchers should be aware of the demographics of their specific population of portal users in order to avoid bias in recruitment. Patient registration for portal use, even in acute-care settings, should be encouraged as they offer a convenient method to assess long-term outcomes.
Conflicts of interests
Dr. Poulose has received funding for unrelated research from Bard-Davol and Gore. Part of Dr. Jackson’s salary is supported by funding provided to Vanderbilt University by West Health for a research collaboration involving West Heath, West Corporation, and Vanderbilt University. The remaining authors report no conflicts of interest.
Human Subjects Protections
The Vanderbilt University Institutional Review Board approved this study. The study was performed in compliance with the World Medical Association Declaration of Helinski on Ethical Principles for Medical Research Involving Human Subjects. Each patient recruited by telephone gave verbal consent prior to completion of the survey, and those recruited through the patient portal were directed to a screen which explained the purpose of the study, risks and benefits of participation, and contact information for the investigators, prior to entering the survey.
References
- 1.Patient portal [Website]. Wikepedia Foundation, Inc.; [updated May 25, 2014; cited 2014 June 4, 2014]. Available from: http://en.wikipedia.org/wiki/Patient_portal. [Google Scholar]
- 2.Lin C-T, Wittevrongel L, Moore L, Beaty LB, Ross ES.An Internet-Based Patient-Provider Communication System: Randomized Controlled Trial. J Med Internet Res 2005; 7(4): e47 doi: 10.2196/jmir.7.4.e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCarrier KP, Ralston JD, Hirsch IB, Lewis G, Martin DP, Zimmerman FJ, Goldberg HI.Web-based collaborative care for type 1 diabetes: a pilot randomized trial. Diabetes technology & therapeutics. 2009; 11(4):211–217 doi: 10.1089/dia.2008.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krist AH, Woolf SH, Rothemich SF, Johnson RE, Peele JE, Cunningham TD, Longo DR, Bello GA, Matzke GR.Interactive preventive health record to enhance delivery of recommended care: a randomized trial. Annals of family medicine 2012; 10(4):312–319 doi: 10.1370/afm.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT.Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res 2004; 6(2): e12 doi: 10.2196/jmir.6.2.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright A, Poon EG, Wald J, Feblowitz J, Pang JE, Schnipper JL, Grant RW, Gandhi TK, Volk LA, Bloom A, Williams DH, Gardner K, Epstein M, Nelson L, Businger A, Li Q, Bates DW, Middleton B.Randomized controlled trial of health maintenance reminders provided directly to patients through an electronic PHR. J Gen Intern Med 2012; 27(1):85–92 doi: 10.1007/s11606–011–1859–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, Carrell D, Tyll L, Larson EB, Thompson RS.Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. Jama 2008; 299(24):2857–2867 doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI.Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes care 2009; 32(2):234–239 doi: 10.2337/dc08–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang PC, Overhage JM, Chan AS, Brown NL, Aghighi B, Entwistle MP, Hui SL, Hyde SM, Klieman LH, Mitchell CJ, Perkins AJ, Qureshi LS, Waltimyer TA, Winters LJ, Young CY.Online disease management of diabetes: engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. J Am Med Inform Assoc 2013; 20(3):526–534 doi: 10.1136/amiajnl-2012–001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simon GE, Ralston JD, Savarino J, Pabiniak C, Wentzel C, Operskalski BH.Randomized trial of depression follow-up care by online messaging. J Gen Intern Med 2011; 26(7):698–704 doi: 10.1007/s11606–011–1679–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldzweig CL, Orshansky G, Paige NM, Towfigh AA, Haggstrom DA, Miake-Lye I, Beroes JM, Shekelle PG.Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Annals of internal medicine 2013; 159(10):677–687 doi: 10.7326/0003–4819–159–10–201311190–00006. [DOI] [PubMed] [Google Scholar]
- 12.Grant RW, Wald JS, Schnipper JL, Gandhi TK, Poon EG, Orav EJ, Williams DH, Volk LA, Middleton B.Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Archives of internal medicine 2008; 168(16):1776–1782 doi: 10.1001/archinte.168.16.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leveille S, Huang A, Tsai S, Weingart S, Iezzoni L.Screening for Chronic Conditions Using a Patient Internet Portal: Recruitment for an Internet-based Primary Care Intervention. J Gen Intern Med 2008; 23(4):472–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ancker JS, Barron Y, Rockoff ML, Hauser D, Pichardo M, Szerencsy A, Calman N.Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med 2011; 26(10):1117–1123 doi: 10.1007/s11606–011–1749-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW.Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 2011; 26(10):1112–1116 doi: 10.1007/s11606–011–1728–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ralston JD, Rutter CM, Carrell D, Hecht J, Rubanowice D, Simon GE.Patient use of secure electronic messaging within a shared medical record: a cross-sectional study. J Gen Intern Med 2009; 24(3):349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A, Schillinger D.Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011; 18(3):318–321 doi: jamia.2010.006015 [pii] 10.1136/jamia.2010.006015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weingart SN, Rind D, Tofias Z, Sands DZ.Who uses the patient internet portal? The PatientSite experience. J Am Med Inform Assoc 2006; 13(1):91–95 doi: M1833 [pii] 10.1197/jamia.M1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roblin DW, Houston TK, 2nd, Allison JJ, Joski PJ, Becker ER.Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc 2009; 16(5):683–689 doi: M3169 [pii] 10.1197/jamia.M3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kahn JS, Hilton JF, Van Nunnery T, Leasure S, Bryant KM, Hare CB, Thom DH.Personal health records in a public hospital: experience at the HIV/AIDS clinic at San Francisco General Hospital. J Am Med Inform Assoc 2010; 17(2):224–228 doi: 17/2/224 [pii] 10.1136/jamia.2009.000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller H, Vandenbosch B, Ivanov D, Black P.Determinants of personal health record use: a large population study at Cleveland Clinic. J Healthc Inf Manag 2007; 21(3):44–48. [PubMed] [Google Scholar]
- 22.Poulose BK, Shelton J, Phillips S, Moore D, Nealon W, Penson D, Beck W, Holzman MD.Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 2012; 16(2):179–183 doi: 10.1007/s10029–011–0879–9. [DOI] [PubMed] [Google Scholar]
- 23.Osborn CY, Rosenbloom ST, Stenner SP, Anders S, Muse S, Johnson KB, Jirjis J, Jackson GP.MyHealthAt-Vanderbilt: policies and procedures governing patient portal functionality. J Am Med Inform Assoc 2011; 18 (Suppl 1): i18–i23 doi: 10.1136/amiajnl-2011–000184. [DOI] [PMC free article] [PubMed] [Google Scholar]


