Abstract
Background
The QRS-T angle correlates with prognosis in patients with heart failure and coronary artery disease, reflected by an increase in mortality proportional to an increase in the difference between the axes of the QRS complex and T wave in the frontal plane. The value of this correlation in patients with Chagas heart disease is currently unknown.
Objective
Determine the correlation of the QRS-T angle and the risk of induction of ventricular tachycardia / ventricular fibrillation (VT / VF) during electrophysiological study (EPS) in patients with Chagas disease.
Methods
Case-control study at a tertiary center. Patients without induction of VT / VF on EPS were used as controls. The QRS-T angle was categorized as normal (0-105º), borderline (105-135º) or abnormal (135-180º). Differences between groups for continuous variables were analyzed with the t test or Mann-Whitney test, and for categorical variables with Fisher's exact test. P values < 0.05 were considered significant.
Results
Of 116 patients undergoing EPS, 37.9% were excluded due to incomplete information / inactive records or due to the impossibility to correctly calculate the QRS-T angle (presence of left bundle branch block and atrial fibrillation). Of 72 patients included in the study, 31 induced VT / VF on EPS. Of these, the QRS-T angle was normal in 41.9%, borderline in 12.9% and abnormal in 45.2%. Among patients without induction of VT / VF on EPS, the QRS-T angle was normal in 63.4%, borderline in 14.6% and abnormal in 17.1% (p = 0.04). When compared with patients with normal QRS-T angle, those with abnormal angle had a fourfold higher risk of inducing ventricular tachycardia / ventricular fibrillation on EPS [odds ratio (OR) 4; confidence interval (CI) 1.298-12.325; p = 0.028]. After adjustment for other variables such as age, ejection fraction (EF) and QRS size, there was a trend for the abnormal QRS-T angle to identify patients with increased risk of inducing VT / VF during EPS (OR 3.95; CI 0.99-15.82; p = 0.052). The EF also emerged as a predictor of induction of VT / VF: for each point increase in EF, there was a 4% reduction in the rate of sustained ventricular arrhythmia on EPS.
Conclusions
Changes in the QRS-T angle and decreases in EF were associated with an increased risk of induction of VT / VF on EPS.
Keywords: Tachycardia, Ventricular; Arrhythmias, Cardiac; Chagas Disease; Electrocardiography; Case-Control Studies
Introduction
Chagas disease is a prevalent public health problem in Brazil and Latin America. The disease has been gaining importance in developing countries due to intense migration of individuals from places historically considered to be reservoirs of the disease1. It is caused by the parasite Trypanosoma cruzi transmitted vectorially through the bite of triatomine insects, from mother to fetus, orally or through transfusion of contaminated blood2.
The physiopathology of the disease involves inflammation, tissue destruction and fibrosis of cardiac cells leading to dysautonomia, microcirculatory changes and damage to the muscle heart and to the intramural nervous system1. The disease occurs in indeterminate, non-cardiac or cardiac forms. The cardiac form is further subdivided into with or without ventricular dysfunction. Even with normal ejection fraction, patients with Chagas heart disease may progress with several cardiac conduction disorders and severe ventricular arrhythmias which emerge as important prognostic predictors.
Tachyarrhythmias (ventricular tachycardia and ventricular fibrillation) and heart failure are the most common cardiovascular causes of mortality in patients with Chagas disease1,3,4. Tachyarrhythmias may be preceded by typical symptoms or even progress to sudden death without premonitory signs, which may also affect individuals with structurally normal hearts. Considering the prevalence of Chagas disease and the increase in life expectancy, risk stratification for sudden death and tachyarrhythmias is of extreme importance in public health.
The QRS-T angle is an electrocardiographic variable that determines the directions of depolarization and repolarization of the heart in the frontal plane. In normal conditions, these processes have the same spatial orientation but in opposite directions. Differences between both indicate electrical cardiac abnormalities that signal structural myocardial changes affecting depolarization or regional changes in repolarization sequence. Studies show that a simple tool - the electrocardiogram - offers information for risk stratification based on analysis of the QRS-T angle. However, no studies have evaluated the importance of this variable and its association with induction of malignant ventricular arrhythmias during programmed ventricular stimulation in patients with Chagas heart disease.
The aim of this study was to determine whether the QRS-T angle obtained in the frontal plane during a 12-lead resting electrocardiogram is associated with increased risk of induction of ventricular arrhythmia during electrophysiologic study (EPS) in patients with Chagas disease.
Methods
Study planning
This is a retrospective study that included patients with Chagas disease who underwent EPS at Instituto Dante Pazzanese de Cardiologia within the past three years. Patients were divided into two groups according to induction or not of malignant ventricular arrhythmias (sustained ventricular tachycardia, ventricular fibrillation or ventricular flutter) in response to the protocol of ventricular stimulation during the EPS. Collected information included demographic data (age, gender, history of systemic arterial hypertension, diabetes mellitus, dyslipidemia, coronary artery disease, stroke, syncope, use of concomitant medications), electrocardiographic data (rhythm, presence of atrioventricular and intraventricular block, QRS interval and QRS-T angle); echocardiographic data (ejection fraction, right ventricular dysfunction, presence of thrombi or aneurysms) and results of 24-hour Holter monitoring (quantification of ventricular extrasystoles, nonsustained and sustained ventricular tachycardias). These data were obtained from medical records, registered in forms specifically designed for the study and then correlated with EPS findings. Patients were not followed up and the data were collected from records, tests and chart notes.
Cohort of patients
The study included all patients with at least two positive serological tests for Chagas disease who underwent EPS over the previous three years. Information collected about the cohort included medical history and use of medications. Patients with blood pressure ≥ 140 / 90 mmHg5 or using antihypertensive drugs were labeled hypertensive. Serum fasting glucose levels above 126 mg/dL on two occasions or use of oral hypoglycemic agents or insulin was determined as diabetes mellitus. The analysis excluded individuals with cardiomyopathy of other etiologies (coronary artery disease, hypertension, or others), atrial fibrillation, left bundle branch block and those with rhythm determined by a pacemaker. The diagnosis of coronary artery disease was determined by coronary angiography showing at least 70% of stenosis on the affected artery.
Definition of events
Sustained ventricular tachycardia was defined as the occurrence of tachycardia arising from the ventricle with a heart rate above 100 bpm and duration above 30 seconds or associated with clinical or hemodynamic instability. A rapid, disordered, and ineffective ventricular activity characterized the diagnosis of ventricular fibrillation.
Electrocardiogram
The QRS complex and T wave axes on the frontal plane were calculated based on an analysis of the (12-lead) resting electrocardiogram recorded at 25 mm / sec and with amplitude of 10 mm / mV. In both situations, the axis was located on the lead with highest QRS complex and T wave amplitudes. The difference between the angles of the QRS complex and T wave was calculated as the absolute difference between the angles, with values between 0º and 180º. These measurements were determined by two independent reviewers. In case of disagreement, a third reviewer was prompted. The QRS-T angle was categorized in three groups: normal (0-105º), borderline (105-135º) and abnormal (135-180º).
Holter monitoring
24-hour Holter monitoring offered information about the occurrence of ventricular extrasystole and ventricular tachycardia. Ventricular extrasystole was defined as the occurrence of an isolated or coupled beat arising in the ventricle. The occurrence of at least three consecutive ventricular beats with a rate above 100 bpm was defined as nonsustained ventricular tachycardia and, when lasting more than 30 seconds, as sustained ventricular tachycardia.
EPS
All patients underwent EPS according to the standard routine protocol adopted at the institution. The protocol consists of programmed ventricular stimulation with two basic cycles (600 and 500 ms), with up to three extrastimuli at the apex and outflow tract of the right ventricle, in addition to rapid stimulation (up to 250 ms) of the same sites. The first extrastimulus, coupled with the last QRS of the burst pacing and 50 ms faster than the ventricular refractory period, is applied during late diastole. The coupling interval is shortened every 10 ms until the refractory period is reached. The second and third extrastimuli, which are similar to the first, are then introduced in sequence. In the event of ventricular tachycardia, cardioversion to sinus rhythm was performed with rapid ventricular stimulation or, in case of hemodynamic collapse, electrical cardioversion.
Echocardiogram
Echocardiographic assessments included measurement of left atrial diameter, left ventricular systolic and diastolic diameters, left ventricular ejection fraction and, when present, determination of diastolic dysfunction, right ventricular dysfunction, and left ventricular thrombus or aneurysm.
Statistical Analysis
Continuous variables were described as mean and standard deviation, and as interquartile range when appropriate. Categorical variables were presented as relative and absolute frequencies. Differences between groups regarding the induction or not of ventricular arrhythmias were analyzed with the t test or Mann-Whitney test for continuous variables, and with Fisher's exact test for categorical variables. Logistic regression models were applied to identify potential factors influencing the groups in combination. Backward stepwise regression was applied to select the variables, with an alpha-to-remove of 5%. P values below 0.05 were considered statistically significant. Retrieved data were analyzed with the softwares Microsoft Excel and R for Windows.
Results
Between January and July 2013, a total of 116 charts of patients with Chagas disease who underwent EPS were selected. Of these, 44 (37.9%) were excluded due to the following reasons: 18 (15.5%) for incomplete data, 6 (5.2%) for inactive records and 19 (16.4%) in which the calculation of the QRS-T angle was impractical. Of the reasons that precluded the calculation of the QRS-T angle were the occurrence of left bundle branch block in 16 (13.8%) and atrial fibrillation in 3 (2.6%). The final analysis, therefore, included 72 patients.
Mean age was 59.3 ± 10.6 years and 35 patients (48.6%) were males. Mean ejection fraction was 49.8 ± 16.1% and more than half of the cohort had functional class I. Right bundle branch block and left anterior superior divisional block were observed in 41 (56.9%) and 47 (65.3%) patients, respectively. Almost 80% of the patients used angiotensin-converting enzyme inhibitors / angiotensin II receptor blockers, 54.2% used amiodarone and 47.2% used beta-blockers. The QRS-T angle was normal in 39 patients (54.2%), abnormal in 21 (29.2%) and borderline in 10 (13.9%).
Clinical, electrocardiographic, echocardiographic and Holter findings of the 72 patients included in the analysis are described in Table 1.
Table 1.
Clinical, electrocardiographic, echocardiographic and Holter findings of 72 patients with Chagas disease
| Characteristics | N (%) |
|---|---|
| Clinical characteristics | |
| Age in years (mean ± standard deviation) | 59.3 ± 10.6 |
| Male gender | 35 (48.6) |
| Dyslipidemia | 27 (37.5) |
| Syncope | 43 (59.7) |
| Smoking | 5 (6.9) |
| Stroke or TIA | 7 (9.7) |
| Systemic arterial hypertension | 55 (76.4) |
| Diabetes mellitus | 10 (13.9) |
| Implantable cardioverter | 2 (2.8) |
| Pacemaker | 2 (2.8) |
| Functional class | |
| I | 37 (51.4) |
| II | 30 (41.7) |
| III | 5 (6.9) |
| IV | 0 (0.0) |
| Concomitant medications | |
| Beta-blockers | 34 (47.2) |
| Amiodarone | 39 (54.2) |
| ACE inhibitors/ABRs | 57 (79.2) |
| Furosemide | 18 (25.0) |
| Statins | 21 (29.2) |
| Aspirin | 30 (41.7) |
| Oral anticoagulant | 2 (2.8) |
| Spironolactone | 19 (26.4) |
| Electrocardiographic features | |
| First degree ABV | 22 (30.6) |
| Right bundle branch block | 41 (56.9) |
| Left anterior superior hemiblock | 47 (65.3) |
| QRS < 120 ms | 24 (33.3) |
| QRS > 120 ms | 48 (66.7) |
| Normal QRS-T angle | 39 (54.2) |
| Abnormal QRS-T angle | 21 (29.2) |
| Borderline QRS-T angle | 10 (13.9) |
| Echocardiographic characteristics | |
| Ejection fraction (mean) | 49.8 ± 16.1% |
| Diastolic dysfunction | 42 (58.3) |
| Systolic dysfunction | 3 (4.2) |
| Intracardiac thrombus | 1 (1.4) |
| Left ventricular aneurysm | 3 (4.2) |
| Holter findings | |
| 0-10 ventricular extrasystoles / hour | 12 (16.7) |
| 11-30 ventricular extrasystoles / hour | 10 (13.9) |
| > 31 ventricular extrasystoles / hour | 43 (59.7) |
| Nonsustained ventricular tachycardia | 37 (51.4) |
TIA: transitory ischemic attack; ACE: angiotensin-converting enzyme; ABRs: angiotensin II receptor blockers; ABV: atrioventricular block.
There were no differences in baseline characteristics between groups, except for age. These findings are shown in Table 2.
Table 2.
Comparison of clinical characteristics between groups
| Clinical characteristics | Ventricular tachycardia / ventricular fibrillation induction | ||
|---|---|---|---|
| No 41 (56.4%) | Yes 31 (43.1%) | p value | |
| Age (years) | 61.98 | 55.77 | 0.01 |
| Male gender | 16 (39) | 19 (61.3) | 0.09 |
| Dyslipidemia | 16 (39) | 11 (35.5) | 0.81 |
| Syncope | 24 (58.5) | 19 (61.3) | 1.00 |
| Smoking | 3 (7.3) | 2 (6.5) | 1.00 |
| Previous stroke / TIA | 5 (12.2) | 2 (6.5) | 0.69 |
| Systemic arterial hypertension | 30 (73.2) | 25 (80.6) | 0.58 |
| Diabetes mellitus | 6 (14.6) | 4 (12.9) | 1.00 |
TIA: transitory ischemic attack.
Statins and aspirin were the most commonly prescribed medications in the group without induction of malignant ventricular arrhythmias. Even though beta-blockers and spironolactone were used more often in the group with induction of arrhythmias, this difference did not reach statistical significance (Table 3).
Table 3.
Comparison between groups regarding use of concomitant medications
| Concomitant medications | Induction of ventricular tachycardia / ventricular fibrillation | ||
|---|---|---|---|
| No 41 (56.4%) | Yes 31 (43.1%) | P value | |
| Beta-blocker | 15 (36.6) | 19 (61.3) | 0.06 |
| Amiodarone | 22 (53.7) | 17 (54.8) | 1.00 |
| ACE inhibitors/ABRs | 33 (80.5) | 24 (77.4) | 0.78 |
| Furosemide | 10 (24.4) | 8 (25.8) | 1.00 |
| Statins | 16 (39.0) | 5 (16.1) | 0.04 |
| Aspirin | 22 (53.7) | 8 (25.8) | 0.03 |
| OA | 2(4.9) | 0 (0.0) | 0.50 |
| Spironolactone | 8 (19.5) | 11 (35.5) | 0.18 |
ACE: angiotensin-converting enzyme: ABRs: angiotensin II receptor blockers: OA: oral anticoagulant.
A QRS complex duration greater than 120 ms was observed more frequently in patients without induction of sustained ventricular arrhythmias. Among patients with induction of ventricular arrhythmias on EPS, the QRS-T angle was normal in 13 (41.9%), borderline in 4 (12.9%) and abnormal in 14 (45.2%). In the group of patients without induction of ventricular arrhythmias, the QRS-T angle was normal in 26 (63.4%), borderline in 6 (14.6%) and abnormal in 7 (17.1%, p = 0.04). The frequency of ventricular extrasystoles on 24-hour Holter was higher in individuals without induction of ventricular arrhythmias on EPS (70.3% versus 60.7%), however, this finding showed no statistical significance (p = 0.71).
Mean left ventricular ejection fraction in the group with induction of ventricular arrhythmia was 42.6%, compared with 55.1% in the group without induction of ventricular arrhythmias (p = 003, Tables 4 and 5).
Table 4.
Comparison of electrocardiographic findings between groups
| Electrocardiographic findings | Induction of ventricular tachycardia / ventricular fibrillation | |||
|---|---|---|---|---|
| No 41 (56.4%) | Yes 31 (43.1%) | P value | ||
| First degree AVB | 12 (29.3) | 10 (32.3) | 0.80 | |
| Right bundle branch block | 25 (61.0) | 16 (51.6) | 0.48 | |
| Left anterior superior hemiblock | 29 (70.7) | 18 (58.1) | 0.32 | |
| QRS < 120 ms | 16 (39.0) | 8 (25.8) | ||
| QRS < 120 ms | 25 (61.0) | 23 (74.2) | 0.88 | |
| QRS-T angle | ||||
| Normal | 26 (63.4) | 13 (41.9) | 0.04 | |
| Borderline | 6 (14.6) | 4 (12.9) | ||
| Abnormal | 7 (17.1) | 14 (45.2) | ||
ABV: atrioventricular block.
Table 5.
Comparison of echocardiographic and Holter findings between groups
| Findings of echocardiogram and Holter | Induction of ventricular tachycardia / ventricular fibrillation | ||
|---|---|---|---|
| No 41 (56.4%) | Yes 31 (43.1%) | p value | |
| Left ventricular diastolic dysfunction | 26 (63.4) | 16 (51.6) | 0.47 |
| Right ventricular dysfunction | 1 (2.4) | 2 (6.5) | 0.57 |
| Left ventricular thrombus | 0(0.0) | 1 (3.2) | 0.42 |
| Mean ejection fraction | 55.12 | 42.57 | 0.03 |
| 0-10 ventricular extrasystoles / hour | 6 (14.6) | 6 (19.4) | 0.71 |
| 11-30 ventricular extrasystoles / hour | 5 (12.2) | 5 (16.1) | |
| > 31 ventricular extrasystoles / hour | 26 (63.4) | 17 (54.8) | |
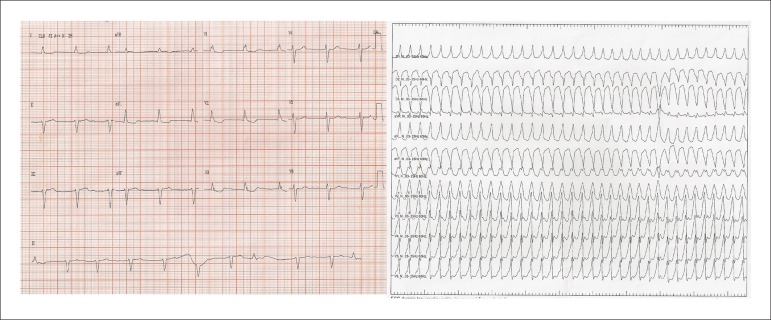
Figure 1 shows findings from a patient with abnormal QRS-T angle who induced sustained ventricular tachycardia on EPS.
Figure 1.
Left, electrocardiogram showing abnormal QRS-T angle (SÂQRS= -70º; SÂT = +100º; QRS-T 170º angle). Right, sustained monomorphic ventricular tachycardia induced during electrophysiological study of the same patient.
On logistic regression analysis, ejection fraction emerged as a strong predictor of induction of ventricular tachycardia / ventricular fibrillation in this cohort. For each point increase in the ejection fraction there was a reduction of approximately 4% on the induction rate of ventricular tachycardia / ventricular fibrillation on EPS. Compared with patients with normal QRS-T angle, those with abnormal angle had a fourfold increased risk of inducing ventricular tachycardia / ventricular fibrillation during EPS [odds ratio (OR) 4; confidence interval (CI) 1.298-12.325; p=0.028]. After adjustment for other variables such as age, ejection fraction and QRS size, there was a trend in the abnormal QRS-T angle to identify patients with increased risk of induction of VT / VF during EPS (OR 3.95; CI 0.99-15.82; p = 0.052, Table 6).
Table 6.
Multivariate analysis in patients who induced ventricular tachyarrhythmia during EPS
| Induction of ventricular tachycardia / ventricular fibrillation Ventricular | ||||
|---|---|---|---|---|
| OR | p value | CI | ||
| Age > 65 years | 0.25 | 0.04 | 0.06 - 0.97 | |
| Ejection fraction < 35% | 4.84 | 0.02 | 1.23 - 19.09 | |
| Beta-blocker use | 1.30 | 0.64 | 0.39 - 4.33 | |
| QRS < 120 ms | 1.35 | 0.65 | 0.37 - 4.90 | |
| QRS-T angle | ||||
| Normal | ||||
| Borderline | 1.23 | 0 80 | 0.24 - 6.14 | |
| Abnormal | 3.95 | 0.052 | 0.99 - 15.82 | |
Discussion
The results of this study show that patients with Chagas heart disease with abnormal QRS-T angle in the frontal plane tend to have a higher risk of inducing ventricular tachycardia / ventricular fibrillation during programmed ventricular stimulation on the EPS. This finding shows that an electrocardiographic variable may help clinicians establish a prognosis for future arrhythmic events in this population.
Abnormalities in ventricular repolarization are associated with increased susceptibility to complex arrhythmias6. Rassi et al7 demonstrated that an abnormal ECG associated with symptoms of heart failure - functional class III or IV - determine a high mortality risk in patients with Chagas disease. This finding allows guidance of specific therapies directed to this subgroup of patients. In addition to that, the analysis of the amplitude and duration, as well as the spatial and frontal axes of the QRS-T angle have also been described in several clinical studies as strong and independent predictors of mortality in elderly patients8,9, HIV patients receiving antiretroviral drugs10, patients with coronary artery disease11 and conditions such as acute coronary syndrome12, post-acute myocardial infarction13, heart failure14 and nonischemic cardiomyopathy15.
Previous studies have highlighted the importance of the QRS-T angle as an independent predictor of mortality in patients with Chagas disease16-18. However, until now, there had been no reports of the association between the value of the QRS-T angle on the induction of malignant arrhythmias in this population, which would reflect an increased possibility of high risk arrhythmic events in this population. In this study, the direct comparison between abnormal and normal QRS-T angles showed that the first was associated with a fourfold increased risk of induction of ventricular arrhythmia during EPS, highlighting the importance of this simple electrocardiographic variable in risk stratification of a population with such severe cardiopathy.
The ideal method of calculating the QRS-T angle is a matter of discussion. The angle may be determined by spatial calculation or by a simple difference between the angles of the QRS complex and the T wave in the frontal plane. However, the spatial calculation requires the Frank leads (X, Y, Z), which are not always available in conventional electrocardiographs, making this calculation less practical. In contrast, the determination of the difference between the angles in the frontal plane (the technique adopted in this study) is more practical, and of easy reach and interpretation in clinical practice. Zhang et al. demonstrated that the determination of the QRS-T angle in the frontal plane shows good correlation with the findings obtained on spatial determination11. However, Brown and Schlegel19 , when comparing the mean spatial QRS-T angle with frontal plane QRS-T angles determined by conventional electrocardiogram and vectorcardiogram of 370 patients with cardiac disease confirmed by imaging tests (coronary artery disease, hypertrophic cardiomyopathy, or ventricular systolic dysfunction) and 210 apparently normal individuals, identified a statistically significant difference favoring a stronger prognostic power for the spatial method. The authors interpreted this result as decisive to suggest that the frontal plane QRS-T angle should not be used to replace the spatial QRS-T angle. In contrast, a recent study by Aro et al20 assessing the QRS-T angle in the frontal plane demonstrated that 2% of a population of 10,957 individuals had a difference > 100 degrees and a higher rate of sudden death from arrhythmic causes and total mortality when compared with those with normal QRS-T angle. These along with Zhang's data support the adoption of the simple difference between the axes of the QRS complex and T wave in the frontal plane as equally useful in determining the risk of induction of ventricular tachycardia / ventricular fibrillation in patients with Chagas disease undergoing EPS.
The presence of fibrotic areas or tissues with low capacity to conduct electricity may modify the process of cardiac depolarization and repolarization, representing therefore an area with a reentrant circuit. Abnormalities in activation and recovery of electrical activity, obtained by differences between the angles of the QRS complex and the T wave in the frontal plane may suggest the presence of this circuit and were, therefore, probably associated with a an increased probability of induction of ventricular tachycardia in this population of patients with Chagas disease.
Lastly, it should be emphasized that a left ventricular systolic dysfunction was associated with increased induction of malignant ventricular arrhythmias in the studied population. These results corroborate evidence published recently by our group and reflect the prognostic value of arrhythmogenic circuits secondary to fibrotic areas intermixed with normal conduction tissue21.
Limitations
The limitations of this study include its observational retrospective nature, the small sample size and the collection of data from charts. The protocol of ventricular stimulation was similar for all patients, since it follows a methodology proposed by the group which has been routinely adopted for several years.
Conclusions
Changes in the QRS-T angle and ventricular dysfunction were associated with induction of severe ventricular arrhythmias - ventricular tachycardia and fibrillation - during EPS in the cohort. The presence of ventricular extrasystoles or nonsustained ventricular tachycardia during 24-hour Holter monitoring, as well as clinical factors such as male gender and history of syncope, did not emerge as predictive factors for induction of such outcome.
Footnotes
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author contributions
Conception and design of the research: Zampa HB, Moreira DAR, Armaganijan LV; Acquisition of data and Writing of the manuscript: Zampa HB, Ferreira Filho CAB, Souza CR, Menezes CC, Hirata HS; Analysis and interpretation of the data: Zampa HB; Critical revision of the manuscript for intellectual content: Moreira DAR, Armaganijan LV.
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Andrade JP, Marin-Neto JA, Paola AA, Vilas-Boas F, Oliveira GM, Bacal F, et al. I Latin American guidelines for the diagnosis and treatment of Chagas cardiomyopathy. Arq Bras Cardiol. 2011;97(2) Suppl 3:1–48. [PubMed] [Google Scholar]
- 2.Proceedings of the International Colloquium on Congenital Trypanosoma Cruzi Infection, Cochabamba, Bolivia, 6-8 November 2002. Rev Soc Bras Med Trop. 2005;38(Suppl 2):1–124. [PubMed] [Google Scholar]
- 3.Santo AH. [Chagas disease-related mortality trends, state of Sao Paulo, Brazil, 1985 to 2006: a study using multiple causes of death]. Rev Panam Salud Publica. 2009;26(4):299–309. doi: 10.1590/s1020-49892009001000003. [DOI] [PubMed] [Google Scholar]
- 4.Rassi A, Jr, Rassi SG, Rassi A. Sudden death in Chagas' disease. Arq Bras Cardiol. 2001;76(1):75–96. doi: 10.1590/s0066-782x2001000100008. [DOI] [PubMed] [Google Scholar]
- 5.Sociedade Brasileira de Cardiologia. Sociedade Brasileira de Hipertensão. Sociedade Brasileira de Nefrologia VI Diretrizes brasileiras de hipertensão. Arq Bras Cardiol. 2010;95(1) supl.1:1–51. [PubMed] [Google Scholar]
- 6.Lux RL, Hilbel T, Brockmeier K. Electrocardiographic measures of repolarization revisited: why? what? how? . J Electrocardiol. 2001;34(Suppl):259–264. doi: 10.1054/jelc.2001.28909. [DOI] [PubMed] [Google Scholar]
- 7.Rassi A Jr, Rassi A, Rassi SG. Predictors of mortality in chronic Chagas disease: a systematic review of observational studies. Circulation. 2007;115(9):1101–1108. doi: 10.1161/CIRCULATIONAHA.106.627265. [DOI] [PubMed] [Google Scholar]
- 8.Kors JA, de Bruyne MC, Hoes AW, van Herpen G, Hofman A, van Bemmel JH, et al. T axis as an indicator of risk of cardiac events in elderly people. Lancet. 1998;352(9128):601–605. doi: 10.1016/S0140-6736(97)10190-8. [DOI] [PubMed] [Google Scholar]
- 9.Kardys I, Kors JA, van der Meer IM, Hofman A, van der Kuip DA, Witteman JC. Spatial QRS-T angle predicts cardiac death in a general population. Eur Heart J. 2003;24(14):1357–1364. doi: 10.1016/s0195-668x(03)00203-3. [DOI] [PubMed] [Google Scholar]
- 10.Dawood FZ, Khan F, Roediger MP, Zhang ZM, Swaminathan S, Klinker H, et al. Electrocardiographic spatial QRS-T angle and incident cardiovascular disease in HIV-infected patients (from the Strategies for the Management of Antiretroviral Therapy [SMART] study) Am J Cardiol. 2013;111(1):118–124. doi: 10.1016/j.amjcard.2012.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang ZM, Prineas RJ, Case D, Soliman EZ, Rautaharju PM, Group AR. Comparison of the prognostic significance of the electrocardiographic QRS/T angles in predicting incident coronary heart disease and total mortality (from the atherosclerosis risk in communities study) Am J Cardiol. 2007;100(5):844–849. doi: 10.1016/j.amjcard.2007.03.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lown MT, Munyombwe T, Harrison W, West RM, Hall CA, Morrel C, et al. Association of frontal QRS-T angle--age risk score on admission electrocardiogram with mortality in patients admitted with an acute coronary syndrome. Am J Cardiol. 2012;109(3):307–313. doi: 10.1016/j.amjcard.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 13.Li YH, Ren XJ, Han ZH, Wang YL, Wang Y, Zhang JR, et al. Value of the frontal planar QRS-T angle on cardiac dysfunction in patients with old myocardial infarction. Int J Clin Exp Med. 2013;6(8):688–692. [PMC free article] [PubMed] [Google Scholar]
- 14.Gotsman I, Keren A, Hellman Y, Banker J, Lotan C, Zwas DR. Usefulness of electrocardiographic frontal QRS-T angle to predict increased morbidity and mortality in patients with chronic heart failure. Am J Cardiol. 2013;111(10):1452–1459. doi: 10.1016/j.amjcard.2013.01.294. [DOI] [PubMed] [Google Scholar]
- 15.Pavri BB, Hillis MB, Subacius H, Brumberg GE, Schaechter A, Levine JH, et al. Prognostic value and temporal behavior of the planar QRS-T angle in patients with nonischemic cardiomyopathy. Circulation. 2008;117(25):3181–3186. doi: 10.1161/CIRCULATIONAHA.107.733451. [DOI] [PubMed] [Google Scholar]
- 16.Salles G, Xavier S, Sousa A, Hasslocher-Moreno A, Cardoso C. Prognostic value of QT interval parameters for mortality risk stratification in Chagas' disease: results of a long-term follow-up study. Circulation. 2003;108(3):305–312. doi: 10.1161/01.CIR.0000079174.13444.9C. [DOI] [PubMed] [Google Scholar]
- 17.Rautaharju PM, Nelson JC, Kronmal RA, Zhang AM, Robbins J, Gottdiener JC, et al. Usefulness of T-axis deviation as an independent risk indicator for incident cardiac events in older men and women free from coronary heart disease (the Cardiovascular Health Study) Am J Cardiol. 2001;88(2):118–123. doi: 10.1016/s0002-9149(01)01604-6. [DOI] [PubMed] [Google Scholar]
- 18.Salles GF, Xavier SS, Sousa AS, Hasslocher-Moreno A, Cardoso CR. T-wave axis deviation as an independent predictor of mortality in chronic Chagas' disease. Am J Cardiol. 2004;93(9):1136–1140. doi: 10.1016/j.amjcard.2004.01.040. [DOI] [PubMed] [Google Scholar]
- 19.Brown RA, Schlegel TT. Diagnostic utility of the spatial versus individual planar QRS-T angles in cardiac disease detection. J Electrocardiol. 2011;44(4):404–409. doi: 10.1016/j.jelectrocard.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Aro AL, Huikuri HV, Tikkanen JT, Junttilla MJ, Rissanen HA, Reunanen A, et al. QRS-T angle as a predictor of sudden cardiac death in a middle-aged general population. Europace. 2012;14(6):872–876. doi: 10.1093/europace/eur393. [DOI] [PubMed] [Google Scholar]
- 21.Armaganijan L, Moreira DA, Nolasco De Araújo RR, Puzzi MA, Munhoz FP, Carvalho MJ, et al. The usefulness of T-wave peak to T-wave end interval in identifying malignant arrhythmias in patients with Chagas disease. Hellenic J Cardiol. 2013;54(6):429–434. [PubMed] [Google Scholar]