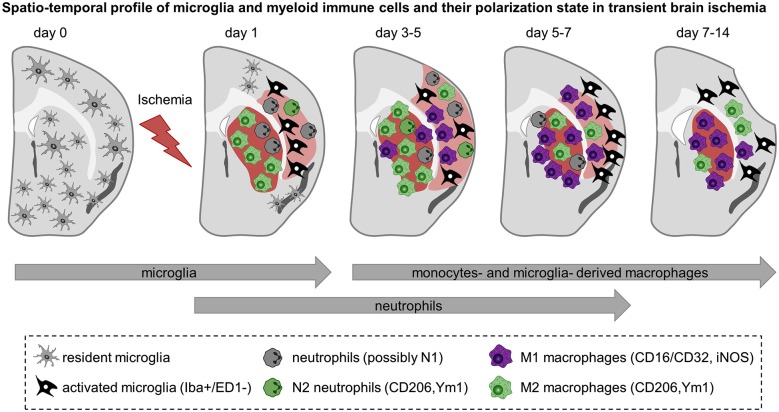
Figure 2.
Spatiotemporal profile of myeloid immune cell activation in acute cerebral ischemia. Schematic representation of rodent brain coronal sections through the anterior commissure (bregma = 0) after transient MCA occlusion in C57BL/6 mice. The core of the infarct is represented in red and the peri-infarct area is shown in light red. The evolution of the infarct is based on observations of ours and others and depicted as follow: infarct size becomes detectable 1 day after transient MCA occlusion, is maximal at 3–5 days after ischemia onset and decreases afterwards together with shrinkage of the injured hemisphere and enlargement of the ventricles. Before injury, resident microglia display ramified thin processes and are highly motile. They scan their microenvironment to detect any disturbances. Cerebral ischemia triggers microglia to become activated and to display distinct shapes and expression patterns upon the course of reperfusion. Based on findings depicted here, microglia become activated at the onset of cerebral ischemia—as early as 1 day after injury—and further develop into macrophages. In the core of the infarct, microglia are round-shaped, expressed ED-1 and display a M2 phenotype aimed at phagocytize the cellular debris and clear the damaged tissue. In the peri-infarct region microglia have ramified processes but are negative for the phagocytic marker ED-1. They are present early after injury, peak between 5–7 days and decrease thereafter. Neutrophils are the first myeloid immune cells to invade the brain and might display a N1 or N2 phenotypes. They can be detected in the ischemic region from 1 to 5–7 days after injury. Monocytes infiltrate the ischemic parenchyma after microglia activation and transform into macrophages. Between 3–5 days M2 macrophages are more abundant in the striatum—the core of the infarct—and decline by 2 weeks. In contrast, pro-inflammatory M1 cells are first observed in the peri-infarct of the lesion and increase in number in the core over time and outnumber the M2 macrophages later on. From 3–5 days onwards it is not clear yet whether the so called M1 and M2 macrophages found in the ischemic region are derived preferentially from microglia or infiltrated monocytes and if they have similar functions. Preliminary data suggest that microglia-derived macrophages can proliferate and have greater phagocytic properties than monocytes-derived macrophages.