Abstract
Objective
The aim of this prospective study was to determine whether the additional use of the single photon emission computed tomography/CT (SPECT/CT) technique improves the diagnostic value of planar lymphoscintigraphy in patients presenting with primary lymph edema of the lower limb.
Materials and Methods
For a defined period of three years (April 2011-April 2014) a total of 34 consecutive patients (28 females; age range, 27-83 years) presenting with swelling of the leg(s) suspicious of (uni- or bilateral, proximal or distal) primary lymphedema were prospectively examined by planar lymphoscintigraphy (lower limbs, n = 67) and the tomographic SPECT/CT technique (anatomical sides, n = 65).
Results
In comparison to pathological planar scintigraphic findings, the addition of SPECT/CT provided relevant additional information regarding the presence of dermal backflow (86%), the anatomical extent of lymphatic disorders (64%), the presence or absence of lymph nodes (46%), and the visualization of lymph vessels (4%).
Conclusion
As an adjunct to planar lymphoscintigraphy, SPECT/CT specifies the anatomical correlation of lymphatic disorders and thus improves assessment of the extent of pathology due to the particular advantages of tomographic separation of overlapping sources. The interpretation of scintigraphic data benefits not only in baseline diagnosis, but also in physiotherapeutical and microsurgical treatments of primary lymphedema.
Keywords: Lymphoscintigraphy, SPECT/CT, Hybrid imaging, Lymphedema, Dermal backflow
INTRODUCTION
Peripheral lymphedema is caused by an insufficiency of lymph circulation. The diagnosis is based on clinical findings, but imaging studies permit objective confirmation (1), especially in the clinically less apparent early stages of lymphatic disease. Due to its high specificity for the lymphatic vessel system (2), lymphoscintigraphy performed with subcutaneously injected technetium-99m-labeled nanocolloids reliably provides information about lymph transport, filtration, and reticuloendothelial function. However, lymphoscintigraphy inherently suffers from limitations arising from low spatial resolution, such that the anatomical localization of diseased lymphatic vessels can be unsatisfactory (3). Secondary morphological disorders, such as fibrotic tissues are best detected by computed tomography (CT), which provides additional useful anatomic information about the impaired lymphatic system.When there is an insufficiency of the peripheral lymphatic system, the phenomenon of "dermal backflow" can occur, resulting in diffuse lymph transport by superficial lymphatic vessels.
Single photon emission computed tomography/CT (SPECT/CT), a hybrid imaging modality that merges functional and anatomic information and redefines the radiotracer principle in the context of morphological imaging, is expected to create a more powerful diagnostic tool than the separate component modalities. To the best of our knowledge, the following is the most extensive published study of lymphoscintigraphic investigations of primary lymphedema of the lower limb, as it retrospectively describes 17 patients, suggesting SPECT/CT is a promising addition to planar imaging in lymphedema (4).
We intended to prospectively compare conventional planar scintigraphy and CT-based tomographic acquisition in the assessment of a series of patients with clinically suspected lymphatic disease, hypothesizing that the additional use of the SPECT/CT technique will improve the diagnostic value of planar lymphoscintigraphy in patients presenting with primary lower limb lymph edema.
MATERIALS AND METHODS
Patients
For a defined period of three years (April 2011-April 2014) a total of 34 consecutive patients (28 females; mean age 47 years, range 27-83) presenting with swelling of the leg(s) suspicious of (unilateral or bilateral, proximal or distal) primary lymphedema were prospectively examined by planar lymphoscintigraphy (lower limbs, n = 67) and additional tomographic SPECT/CT technique (anatomical sides, n = 65). In accordance with the German law, pre-approval by an Institutional Review Board was not required for this study, which complied with the Declaration of Helsinki. Lymphoscintigraphy is a well-established and routine diagnostic procedure at our clinic; all patients gave written informed consent prior to undergoing the procedure. The datasets of six patients (lower limbs, n = 11) had to be excluded since these patients declined to give consent to participate in the additional SPECT/CT procedure. Exclusion criteria were typical contraindications to scintigraphy, such as pregnancy and breastfeeding.
A previous clinical diagnosis of lymphedema was established according to the criteria of the International Society of Lymphology Classification of 2013 (5). The scintigraphic and SPECT/CT imaging tests were performed in all patients following the removal of any compressive bandages. We observed no negative side effects or adverse reactions related to the injection of the radiopharmaceutical.
Lymphoscintigraphy
Technetium-99m-labelled human serum albumin (Nanocoll; GE Healthcare, Munich, Germany) was administered at a mean dose of 102 MBq (median 101; range 62?-135) in a volume of 0.3 mL; the mean left and right leg doses were nearly identical (103 MBq vs. 102 MBq). The radiopharmaceutical was administered by an injection with a 27-gauge needle into the subcutaneous tissue of the first interdigital space of the foot, strictly avoiding intravascular application. Because lymphatic flow at rest is low, patients were asked to stimulate lymphatic drainage by walking for ten minutes after the injection. Beginning at ten minutes after injection, sequential images of the lower limbs were acquired using a low-energy-high-resolution collimator (e.cam; Siemens Healthcare Sector, Erlangen, Germany). The image matrices measured 256 × 1024, and were acquired extending from the feet to the liver at a scanning speed of 5 cm/min. The acquisition was repeated at intervals of about 60 minutes, and ended either by default at five hours after tracer administration, or when inguinal lymph nodes were detected.
As illustrated in Table 1, the additional SPECT/CT was performed either in the pelvic region, the upper or lower leg (including the knees), or the foot. Due to dosimetry limits, the SPECT/CT acquisition was limited to a maximum of two regions: first, in all patients, the segment presenting the maximum of diffuse or focal tracer pattern was selected to tomographically separate overlapping sources of tracer uptake. In addition, for cases of "missing" inguinal lymph nodes in planar scintigraphy, a second SPECT/CT acquisition of the pelvic region was performed in order to morphologically detect any reduction of lymph nodes.
Single photon emission computed tomography/CT-parameters were as follows: 360°, image matrices 128 × 128, 3°, 5 mm, 0.8 sec/step, 130 kV, 20 mAs (Symbia; Siemens Healthcare Sector, Erlangen, Germany). The reconstructions were performed using the HERMES-System (hybrid-recon, OSEM 1 iteration, 4 subsets).
Image Analysis
The data sets of lymphoscintigraphic tests were analyzed in two stages by two experienced nuclear medicine physicians. Initially, planar findings were assessed by a physician blinded to the findings of the other physician and thereafter the results of the tomographic acquisition (transversal, sagittal, and coronal views) were evaluated in a second step.
The presence or absence of lymphatic disorders, such as lymphoceles or "dermal backflow", not caused by the tracer applications, was recorded for each examined limb, and a well-established transport-index (TI) was used to assess the extension of the pathology (6, 7). In order to quantify the visual scintigraphic findings, a numeric index of transport kinetics combining a visual assessment of five criteria was applied as previously described by Kleinhans et al. (6).To that end, five visually assessed criteria were evaluated: temporal and flat transport kinetics (K), radiopharmaceutical distribution pattern (D), time to appearance of inguinal lymph nodes (T), graded visualization of lymph nodes (N), and of lymph vessels (V). For assessment, scores ranging from 0 to 9 were used, as described in Table 2. According to these parameters, lymphatic flow was normal if no substantial delay of transport kinetics was observed, the distribution pattern was not diffuse, the time of appearance of the inguinal lymph nodes was less than 25 minutes after injection, and lymph nodes and vessels were clearly visible. The TI was calculated by the formula: TI = K + D + 0.04T + N + V. Normalization of time (T, minute) was performed with the factor 0.04; absence of evident lymph node appearance was scored as TI = 9. Thus, the resulting TI values ranged from 0 (normal) to 45 (most pathological), where any TI less than ten was considered normal (6).
Table 2.
Calculation of Transport-Index
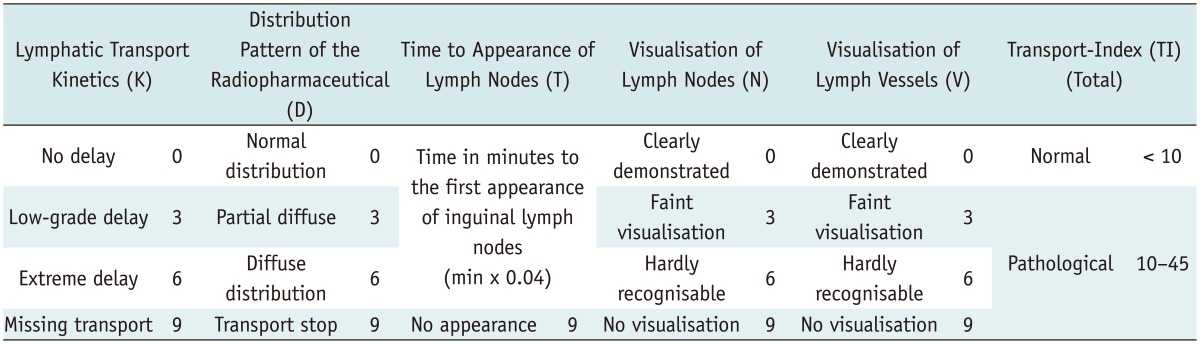
Note.- Calculation of transport-index (TI); resulting TI values range from 0 (normal) to 45 (most pathological), where any TI less than ten is considered normal.
Regarding additional relevant diagnostic information by SPECT/CT visual interpretation of scintigraphic findings were scanned due to the following criteria by comparison to planar acquisition:
- exact anatomic allocation of lymphatic disease based on anatomical margins,
- three-dimensional extent of lymphatic transport disorder,
- presence of "dermal backflow" with reference to spatial anatomic margins,
- morphological visualization of lymph vessels,
- increasing number of the number of morphologically depicted lymph nodes, as distinct from those with "missing" function.
RESULTS
All patients (n = 34) underwent planar scintigraphy in 67 lower limbs, giving a total of 65 anatomic sites investigated by SPECT/CT.
Regarding the lymph kinetics, planar scintigraphy showed in 62.7% (42/67) of cases without delay, 23.9% (16/67) with low-grade delay, 9.0% (6/67) with extreme delay, and 4.5% (3/67) with missing transport. The distribution of the radiopharmaceutical was normal in 59.7% (40/67) of lower limbs, partially diffuse in 25.4% (17/67), diffuse in 13.4% (9/67) and one patient 1.5% (1/67) showed a transport stop. In 53.7% (36/67) of cases, the time to appearance of inguinal lymph nodes was < 25 minutes, in 28/67 (41.8%) cases the time to appearance was > 25 minutes, and in 3/67 (4.5%) limbs, there was no scintigraphical visualization of inguinal lymph nodes in the default time interval of five hours after tracer administration. The visualization of lymph nodes could be clearly depicted in 74.6% (50/67)of lower limbs, showed faint visualization in 13.4% (9/67)of limbs, was hardly recognizable in 4.5% (3/67) of limbs, and showed no visualization in 7.5% (5/67) of limbs. The visualization of lymph vessels could be clearly depicted in 62.7% (42/67) lower limbs, showed faint visualization in 19.4% (13/67) of limbs, was hardly recognizable in 8/67 limbs, and showed no visualization in 5.9% (4/67) of limbs.
In total, planar lymphoscintigraphy including the calculation of TI (TI ≥ 10) (Table 2) detected a total of 28 limbs presenting as lymphatic disorders; in comparison to pathological planar scintigraphic findings, SPECT/CT provided relevant additional information in 27/28 (96.4%) of the lower extremities. In 64% (18/28) of the lower limbs presenting with pathological planar scintigraphic findings, we obtained additional information using SPECT/CT regarding the exact anatomic allocation of lymphatic disorders, based on anatomic margins. In 86% (24/28) of the lower limbs, SPECT/CT was informative about the presence of diffuse distribution of the radiopharmaceutical due to dermal backflow; this additional value was derived from the three-dimensional depiction and superior spatial resolution of SPECT/CT. In 4% (1/28) of the lower limbs, there was a faint visualization of lymph vessels by SPECT/CT. Thirteen of 28 (46%) lower limbs showed an increasing or reduced number of inguinal lymph nodes; while planar scintigraphy could only functionally demonstrate the inguinal lymph nodes, the CT-component of SPECT/CT served to verify the morphology and the presence or absence of lymph nodes in the corresponding area. Table 1 presents the number of tomographically investigated anatomic sites, as well as the improvements of diagnostic value due to the additional use of SPECT/CT. Representative examples are depicted in Figures 1,2,3.
Table 1.
Additional Diagnostic Information from SPECT/CT
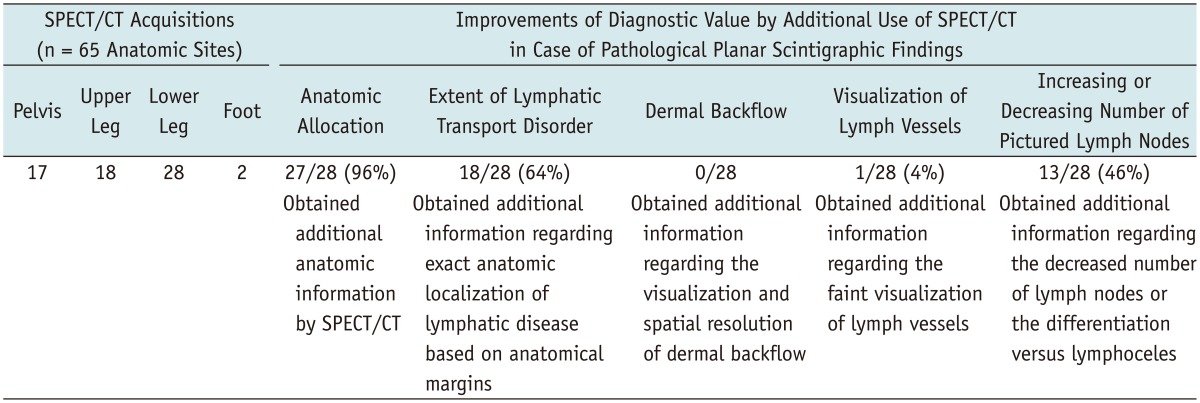
Note.- Number of tomographically investigated anatomic sites, as well as improvements of diagnostic value by additional use of SPECT/CT compared to planar scintigraphy. SPECT/CT = single photon emission computed tomography/CT
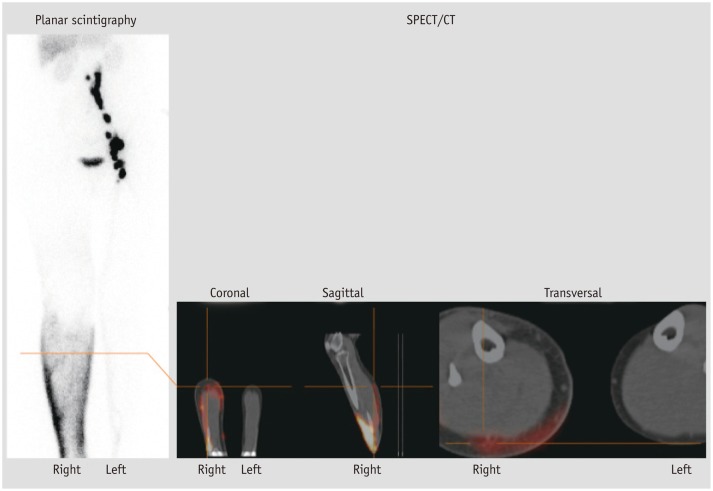
Fig. 1.
60-year-old female patient with clinically swelling of lower right leg suspicious for primary lymphedema. Lymphatic transport disorders (diffuse distribution of radiopharmaceutical at right lower leg, delayed/missing inguinal lymph nodes of right leg, transport-index 39) were properly detected in planar lymphoscintigraphy (4.5 hours after injection), but only tomographic acquisition by means of single photon emission computed tomography/CT (SPECT/CT) confirmed "dermal backflow" at posterior right lower leg (red colored); additional value of SPECT/CT in terms of dermal backflow consists of three-dimensional spatial resolution and definable location of anatomical margins. Physiological lymph transport and distinct visualization of inguinal and iliacal lymph nodes of left leg.
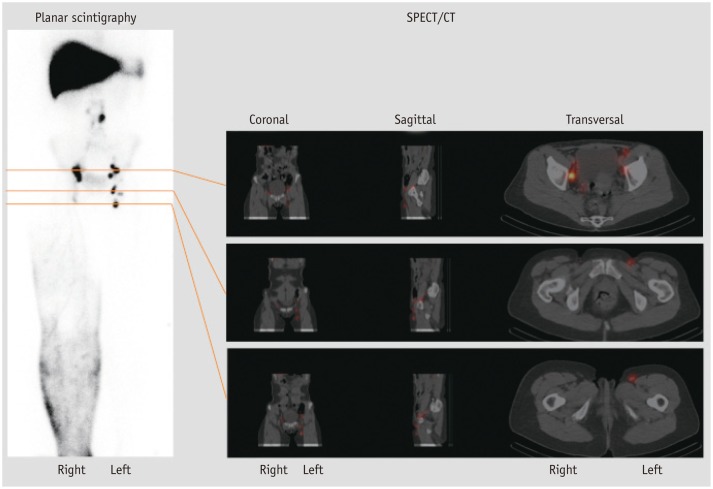
Fig. 2.
46-year-old female patient with clinically swelling of right leg suspicious for primary lymphedema. Planar lymphoscintigraphy clearly depicted diffuse distribution of radiopharmaceutical at right lower leg and upper leg. In comparison to contralateral side, likely decreased number of inguinal lymph nodes could be suspected, which was reliably confirmed with three-dimensional anatomical correlation by means of single photon emission computed tomography/CT (SPECT/CT). While planar scintigraphy is limited to functionally demonstrate (inguinal) lymph nodes, CT-component of SPECT/CT serves to verify morphological presence of lymph nodes in this area. Physiological lymph transport and distinct visualization of inguinal lymph nodes of left leg.
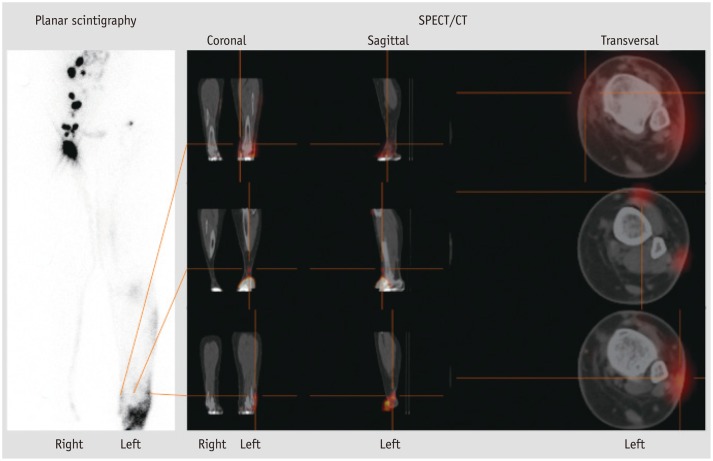
Fig. 3.
65-year-old female patient with clinically swelling of lower left leg suspicious for primary lymphedema. Lymphatic transport disorders (e.g., diffuse distribution of radiopharmaceutical at left lower leg, delayed/missing inguinal lymph nodes of left leg, transport-index 11) were properly detected in planar lymphoscintigraphy (4 hours after injection); due to its three-dimensional imaging options, additionally performed single photon emission computed tomography/CT (SPECT/CT) enables differentiation of anterior versus posterior lymph transport, thus providing accurate anatomic correlation and functional assessment of extent of edema (red colored). Planar lymphoscintigraphy cannot provide these special kinds of morphological information. Physiological lymph transport and distinct visualization of inguinal and iliacal lymph nodes of right leg.
DISCUSSION
In our study, we analyzed the additional diagnostic value of the SPECT/CT technique in patients presenting with primary lymphedema in lower extremities. From the inception of this project, the standardized scintigraphic tests have been maintained; in particular, we have adhered to a standard for the injected radiopharmaceutical dose and volume (8). Lymphoscintigraphy provides information about lymph transport, filtration, and reticuloendothelial function. The lymphoscintigraphic transport kinetics of technetium-99m-bound agents substantially depends on their particle size; for reliable transport from the interstitium to initial lymph vessels, and for adequate lymph node tracer-uptake, an optimal particle size of about 80-100 nm has been suggested (2).
Among the most important parameters for the diagnosis of lymphedema are the dermal backflow of lymph and the asymmetry of inguinal lymph nodes. Visual interpretation of scintigraphic findings is particularly helpful in determining the characteristics of lymphedema and in addition a semi-quantitative index of lymphatic transport reliably depicts abnormalities of the lymphatic circulation.
However, in chronic lymphedema not only the lymphatic vessels, but also the surrounding and functionally associated connective tissue, are disturbed. Despite the scintigraphically demonstrated function of dynamic flow within the lymphatic collectors, the secondary changes (e.g., fibrosis as an excess of connective tissue, sclerosis as a hardening of tissue, and an increase of adipose tissue) may not be depicted; in planar lymphoscintigraphy, the inherent lack of detailed spatial and anatomical information can lead to a misinterpretation of focal tracer accumulation, such as a misattribution of uptake in the popliteal lymph nodes.
In chronic lymphedema, there is a disturbance not only the lymphatic vessels, but also in the surrounding and functionally associated connective tissue. While scintigraphy serves admirably to demonstrate dynamic flow within the lymphatic system, the secondary changes are best demonstrated by morphological imaging, such as the CT-component of the SPECT/CT acquisition (9). While SPECT/CT improved the anatomical correlation of lymphatic transport disorders by reducing image-degrading effects of partial volume, planar lymphoscintigraphy cannot provide this particular information.
Another factor in the decision to use additional tomographic acquisitions with fusions of the anatomic images (SPECT/CT) is related to the purpose of the scintigraphic test. In our hospital, autologous lymph vessel transplantation is one of the major therapeutic options in patients presenting with peripheral lymph edema. Transplantation of autologous lymph collectors is a microsurgical procedure (10), whereby autologous vessel grafts measuring about 25 cm are removed from the superficial medial bundle of the unaffected upper leg. Successful grafting restores lymphatic transport capacity. The graft anastomoses are usually made end-to-end using a tension-free microsurgical technique. Therefore, the high spatial resolution and anatomical information provided by SPECT/CT has proven beneficial for planning these microsurgical therapies.
In general, both planar and tomographic acquisition methods reliably and readily detected lymphatic disorders in our series of patients. Furthermore, our results support the expectation that additional use of the SPECT/CT technique improves the diagnostic value of planar lymphoscintigraphy in primary lymphedema of the lower extremities. SPECT/CT yields improved anatomical correlation of lymphatic transport disorders, and thus a better assessment of the extent of pathology; in addition, tomographic acquisition reduces the image degrading effects of partial volume, thus enabling differentiation of tracer uptake in lymph nodes versus lymphoceles. Scintigraphic interpretation is, similar to other methods, based on lymph node appearances. However, in situations such as agenesis of lymph nodes, the lymphatic system morphology takes on a greater importance as a clinical endpoint to explain functional deficiencies (11). Due to its three-dimensional imaging options, this enables a differentiation of the epifascial versus subfasciallymphatics, thus providing an accurate functional assessment of type and stage of the edema.
In our study, we noted only a faint visualization of lymph vessel by SPECT/CT. Despite the imaging limitations of the low-dose CT compared with a state-of-art CT scanner, the transmission maps allowed for the precise anatomical localizations of the emission images; therefore scintigraphic functional findings become more accurate and meaningful when supported by corresponding morphological details (12) and contributed to the assessment of tissue changes related to the lymph stasis (1). Furthermore, the exact anatomic correlation of lymphatic disorders has proven to be most supportive for physiotherapeutic compression-techniques, planning surgical lipo lympho suctions, and particularly helpful in finding connection capabilities for microsurgical lymph vessel transplantations (3, 13). Planar lymphoscintigraphy cannot provide this morphological information. Our results emphasize that SPECT/CT is best used as a supportive method to augment planar lymphoscintigraphy, delivering additional relevant information to this sensitive method in 96% of the examined, pathological assessed lymph drainage regions due to its tomographic acquisition and the spatial resolution provided by the CT component. Despite these properties, SPECT/CT has yet to become a routine diagnostic tool in the assessment of peripheral lymphedema, in part due to the technical requirements for acquisition.
Regarding the depiction of the general pattern of lymphatic drainage or lymphatic transport delay, there have been some retrospective preliminary reports of tomographic acquisition techniques, such as SPECT/CT, for the diagnosis of lymphedema. Baulieu et al. (4) described the interpretation of delayed planar conventional imaging in 17 patients as questionable due to the superimposition of soft tissues, while Weiss et al. (14) noticed in 11 patients that SPECT/CT-imaging provided relevant additional information before treatment compared to the planar technique. These findings could be confirmed in our enlarged collective.
To our knowledge, this study provides the largest series of patients presenting with primary lymphedema of the lower limb undergoing lymphoscintigraphy in planar and SPECT/CT technique. Our preliminary results show that SPECT/CT combines the superior functional imaging capabilities of SPECT with the anatomical overlay of CT. We note that tomographic imaging has an even better diagnostic value than planar lymphoscintigraphy, and anticipate that SPECT/CT will find traction in assessing lymphatic function. Due to the particular advantages of the improved anatomic localization of lymphatic transport disorders, and tomographic separation of overlapping sources, interpretation of scintigraphic data benefits not only at baseline diagnosis but also during physiotherapeutical and microsurgical treatments of primary lymphedema.
Acknowledgments
All the authors have made substantial contributions to the study, and have approved the final manuscript.
References
- 1.Pecking AP, Albérini JL, Wartski M, Edeline V, Cluzan RV. Relationship between lymphoscintigraphy and clinical findings in lower limb lymphedema (LO): toward a comprehensive staging. Lymphology. 2008;41:1–10. [PubMed] [Google Scholar]
- 2.Weiss M, Gildehaus FJ, Brinkbäumer K, Makowski M, Hahn K. [Lymph kinetics with technetium-99m labeled radiopharmaceuticals. Animal studies] Nuklearmedizin. 2005;44:156–116. doi: 10.1267/nukl05040156. [DOI] [PubMed] [Google Scholar]
- 3.Weiss M, Baumeister RG, Hahn K. Dynamic lymph flow imaging in patients with oedema of the lower limb for evaluation of the functional outcome after autologous lymph vessel transplantation: an 8-year follow-up study. Eur J Nucl Med Mol Imaging. 2003;30:202–206. doi: 10.1007/s00259-002-1020-1. [DOI] [PubMed] [Google Scholar]
- 4.Baulieu F, Bourgeois P, Maruani A, Belgrado JP, Tauveron V, Lorette G, et al. Contributions of SPECT/CT imaging to the lymphoscintigraphic investigations of the lower limb lymphedema. Lymphology. 2013;46:106–119. [PubMed] [Google Scholar]
- 5.International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology. Lymphology. 2013;46:1–11. [PubMed] [Google Scholar]
- 6.Kleinhans E, Baumeister RG, Hahn D, Siuda S, Büll U, Moser E. Evaluation of transport kinetics in lymphoscintigraphy: follow-up study in patients with transplanted lymphatic vessels. Eur J Nucl Med. 1985;10:349–352. doi: 10.1007/BF00251310. [DOI] [PubMed] [Google Scholar]
- 7.Weiss M, Baumeister RG, Tatsch K, Hahn K. [Lymphoscintigraphy for non-invasive long term follow-up of functional outcome in patients with autologous lymph vessel transplantation] Nuklearmedizin. 1996;35:236–242. [PubMed] [Google Scholar]
- 8.Bourgeois P. Scintigraphic investigations of the lymphatic system: the influence of injected volume and quantity of labeled colloidal tracer. J Nucl Med. 2007;48:693–695. doi: 10.2967/jnumed.107.039594. [DOI] [PubMed] [Google Scholar]
- 9.Monnin-Delhom ED, Gallix BP, Achard C, Bruel JM, Janbon C. High resolution unenhanced computed tomography in patients with swollen legs. Lymphology. 2002;35:121–128. [PubMed] [Google Scholar]
- 10.Baumeister RG, Seifert J, Hahn D. Autotransplantation of lymphatic vessels. Lancet. 1981;1:147. doi: 10.1016/s0140-6736(81)90723-6. [DOI] [PubMed] [Google Scholar]
- 11.O'Mahony S, Rose SL, Chilvers AJ, Ballinger JR, Solanki CK, Barber RW, et al. Finding an optimal method for imaging lymphatic vessels of the upper limb. Eur J Nucl Med Mol Imaging. 2004;31:555–563. doi: 10.1007/s00259-003-1399-3. [DOI] [PubMed] [Google Scholar]
- 12.Bocher M, Balan A, Krausz Y, Shrem Y, Lonn A, Wilk M, et al. Gamma camera-mounted anatomical X-ray tomography: technology, system characteristics and first images. Eur J Nucl Med. 2000;27:619–627. doi: 10.1007/s002590050555. [DOI] [PubMed] [Google Scholar]
- 13.Wallmichrath J, Baumeister R, Giunta RE, Notohamiprodjo M, Frick A. [Update on special surgical approaches in the therapy for lymphedemas] Handchir Mikrochir Plast Chir. 2012;44:334–342. doi: 10.1055/s-0032-1323840. [DOI] [PubMed] [Google Scholar]
- 14.Weiss M, Landrock S, Wallmichrath J, Baumeister RG, Bartenstein P, Frick A. [The clinical yield of SPECT/CT for the assessment of lymphatic transport disorders. First experiences] Nuklearmedizin. 2013;52:235–224. doi: 10.3413/Nukmed-0587-13-05. [DOI] [PubMed] [Google Scholar]