Abstract
Objective:
Although autologous chondrocyte implantation (ACI) has become an established surgical treatment for cartilage defects of the knee, little is known about what patients expect about this surgery.
Design:
A total of 150 patients who underwent ACI for cartilage defects at the knee were assigned to the present study and asked about their expectations and estimation concerning the ACI procedure. Patients were asked to answer 4 questions of a web-based questionnaire concerning their expectations on clinical outcome and on factors they considered relevant for clinical outcome.
Results:
A total of 118 (79%) returned questionnaires. Mean patient age was 32.6 years and mean defects size was 4.1 cm2. A proportion of 70% (n = 83) of patients expected pain-free sports participation as a result of the ACI surgery, including 24 patients who expected to return to high-impact sports without any restrictions. Only 12.7% expected a reduction but persistence of pain during everyday activities. Concerning factors that influence outcome, the majority of the patients (55.1%) considered defect characteristics (i.e., size and location) most important for clinical outcome, whereas only a small proportion of patients considered rehabilitation (7.6%), cell quality (10.2%), or prior surgeries (4.2%) more relevant for final outcome.
Conclusion:
The present study illustrates that expectations of ACI patients are demanding and quite high. The ACI technique seems generally considered to be able to restore pain-free sports participation. Patients do not seem to be aware of all factors of possible importance concerning clinical outcome.
Keywords: autologous chondrocyte implantation, cartilage defect, cartilage repair, expectations, cell transplantation
Introduction
Since the introduction in 1994 by the group of Lars Peterson, autologous chondrocyte implantation (ACI) has become an established therapeutic option for treatment of full-thickness cartilage defects of the knee.1,2 In the meantime, high-quality studies3-7 as well as long-term results8-12 are available that prove the safety, efficiency, and durability of this tissue engineering approach.
Although various factors including technical modifications13 and factors that influence outcome and prognostic parameters have been described in detail,14 little is known about the expectations of patients treated with ACI for cartilage defects.
This issue is becoming considerably relevant because the view and opinion of an individual patient on a treatment method generally is not based on the scientific literature that is available on this topic but is mostly influenced by other media, such as television, nonscientific magazines, the Internet, or even from the experience or the opinion of peers. Against this background, the opinion of a patient on a treatment method is likely to differ from the scientific view, and it is very difficult for the surgeon to estimate before surgery. With regard to this, previous studies on other surgical techniques show some surprising and partially controversial results, concerning what patients expect about their surgery.15,16
From a clinical perspective, the patient’s expectancy range before surgery is of great importance, because unrealistically high expectations of a surgery’s benefit can lead to unsatisfied patients in the clinical course following. For different pathologies, it has been demonstrated that fulfilled expectations are linked to a better compliance with postoperative recommendations,17 and patient’s initial expectations and postoperative outcome as well as patient’s satisfaction following surgery has been shown to be correlated by several studies, especially in the field of total joint replacement.18,19 Therefore, appropriate information on what is expectable of ACI can be important, and it might be detrimental to offer patients a treatment based on unrealistic expectations concerning the clinical outcome. In order to better inform patients, it seems important for the surgeon to know a patient’s expectance and to correct it if necessary. Such attempts have also been reported and proven to be efficient in high-quality interventional studies in the field of total joint replacement.20
In general, these findings are independent of the type of surgery performed. There is no current literature available describing patient’s expectations and information with regard to ACI. The aim of the present study was to evaluate the expectations and knowledge of patients who undergo ACI for full-thickness cartilage defects.
Patients and Methods
A total of 150 patients who underwent ACI for isolated cartilage defects across the knee joint at our institution were assigned to the present study. At the time of initial presentation patients were informed about ACI being a cell-based treatment option for cartilage defects that requires an arthroscopic surgery for final decision making and cell harvesting following by a second open surgery during which chondrocytes are transplanted into the defect. All patients were informed about the principles of ACI, including the need of rehabilitation and aftercare. In order not to severely influence the results of question 4, a detailed comment on the period of time that is needed before the regeneration process is completed was not given.
At the time of data evaluation, all patients were asked a total of 4 questions concerning their expectations about ACI before surgery. All patients were contacted via e-mail after surgery; a web-based interface was used in order to collect data. Of the 150 patients initially contacted, 180 contributed to this study (follow-up rate 78.7%). Mean patient age was 32.6 years (SD = 8.3), and all patients suffered from isolated cartilage defects of the knee joint graded III and IV according to ICRS classification21 with a mean defect size of 4.9 cm2 (SD = 1.7). Defect location was medial femoral condyle in 51.9% (n = 61) of cases, lateral femoral condyle and trochlea groove in 9.3% (n = 11), and patella in 29.7% of cases (n = 35).
The questionnaire (in German; translated to English for the purpose of publication) used for the present evaluation contained 4 items.
Item 1: What do you expect as a minimum concerning the benefit from your surgery?
Ability to perform pain-free high-impact sports (such as basketball, soccer, handball, etc.)
Ability to perform pain-free medium-impact sports (such as tennis, jogging, etc.)
Ability to perform pain-free low-impact sports (such as cycling, swimming, etc.)
Pain-free activities of daily living
Reduction of pain during activities of daily living
Delay of total joint replacement
Item 2: The success of the ACI procedure mostly depends on:
individual defect characteristics such as defect size and defect location
personal risk factors and individual parameters such as smoking, body mass index, postoperative compliance
quality of transplanted chondrocytes
quality of the surgery
previous surgeries and treatment prior to the ACI
postoperative rehabilitation
Item 3: Please give the percentage of how important you consider different factors on clinical outcome following ACI in percentage:
individual defect characteristics such as defect size and defect location
personal risk factors and individual parameters such as smoking, body mass index, postoperative compliance
quality of transplanted chondrocytes
quality of the surgery
previous surgeries and treatment prior to the ACI
postoperative rehabilitation
Item 4: Please estimate the amount of time from transplantation of the chondrocytes (date of surgery) to the end of the developing and maturation process of the transplanted cartilage (in months)?
Data Evaluation
The completed questionnaires were examined and then processed anonymously for further analysis. IBM SPSS Statistics 18 (Chicago, Illinois) was used for statistical analysis designed to work up the data collected; this software was also used for preparation of the figures and illustrations.
Results
Response to the Questionnaire
Data for 118 of 150 patients were available for evaluation (follow-up rate 79%).
Item 1
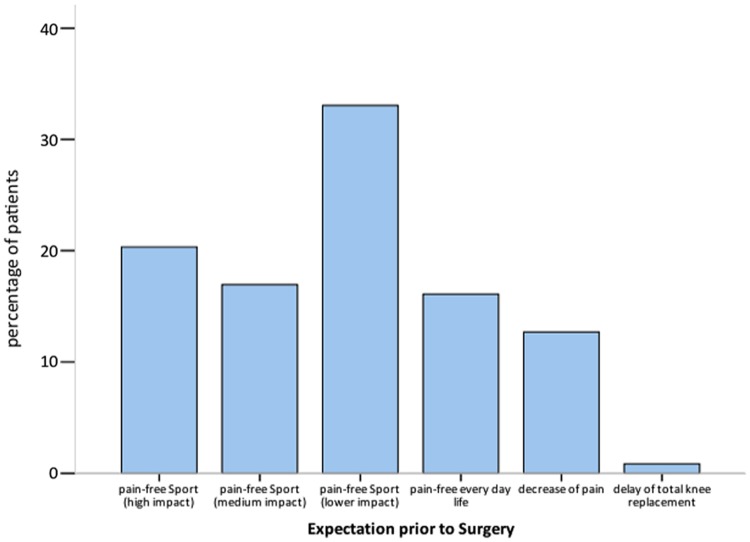
1 of 150 expected a delay of the need for total joint replacement from the ACI procedure (0.8%); a decrease of pain was expected by 15 patients (12.7%) whereas pain-free everyday life as a minimum concerning postoperative activity was expected by 19 patients (16.1%). Pain-free sports at a low impact level was expected by 39 patients (33.1%), at a medium level by further 20 patients (16.9%), and at a high impact level by further 24 patients (20.3%). Therefore, overall, 70.3% patients expected pain-free participation in sports at different levels (Figure 1).
Figure 1.
Minimal expectations of patients following ACI for isolated cartilage defects of the knee (n = 118)
Item 2
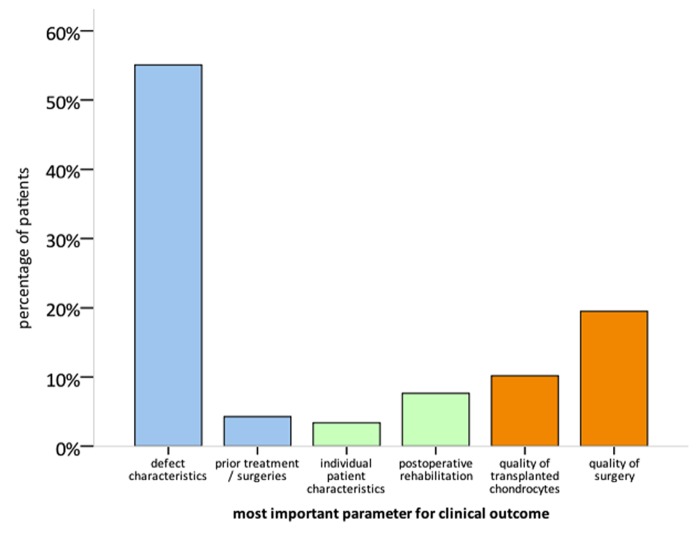
The majority of patients considered defect characteristics most important for clinical outcome (n = 65, 55.1%). Quality of the surgery was considered most important by 23 patients (19.5%), whereas the remaining patients considered quality of the transplanted chondrocytes (n = 12, 10.2%), prior surgical treatment (n = 5, 4.2%), and postoperative rehabilitation (n = 9, 7.6%) most relevant for clinical outcome following ACI (Figure 2).
Figure 2.
Most important factors concerning clinical outcome following ACI according to the estimation of ACI patients (n = 118; blue columns: cannot be influenced by the patient; green columns: can be influenced by the patient; orange columns: issue related to the ACI technique and to the surgeon)
Item 3
Defect characteristics were considered most important (M = 29.2%, SD = 19.4), whereas quality of surgery was considered second most relevant (M = 23.8%, SD = 17.6). Cell quality was considered to influence clinical outcome at an estimate of 16.9% (SD = 14.0), whereas the amount of individual predisposition was considered to influence clinical outcome by 9.8% (SD = 10.1), prior surgeries 5.4% (SD = 8.3), and rehabilitation by 14.1% (SD = 13.1), respectively.
Item 4
Patients estimated the time from cell transplantation to final maturation of the transplanted tissue to be 13.25 months (SD = 8.01; range = 2–36 months).
Discussion
Postoperative satisfaction has been correlated with the fulfillment of patient’s expectations in several studies,22 and preoperative expectations directly seem to influence the postoperative outcome.19 High and even unrealistic preoperative expectations are common, which seem to be more frequent in male, young patients and those with lower body mass index,16,23 which may be related to a higher activity level and overall demand. Therefore, patients’ expectations need to be considered carefully in all patients in whom a surgery is recommended. Because expectations are specific for every kind of pathology and intervention, this has to be addressed separately for every surgical treatment option. Until now, no data are available at all dealing with expectations of patients who undergo ACI for isolated cartilage defects of the knee.
The aim of the present study was to evaluate the expectations of patients eligible for ACI prior to surgery. Because only few standardized scoring systems or scores to evaluate patients’ expectations are available and because those do not seem to be appropriate for the assessment of patients’ expectations in a very selected group of patients, such as patients with cartilage defects before ACI,24 analogous to other studies dealing with various pathologies an individual questionnaire was used in order to evaluate the most important parameters that represent what an individual patient expects from ACI.25,26
A total of 118 of 150 patients were participating in the present study (follow-up rate 79%). This moderate follow-up rate could be explained by the fact that a web-based interface was used for this study. Direct contact in terms of personal communication was avoided so as not to influence the patient by any interviewer suggestions. Nevertheless, dissatisfaction with the treatment or advice given, general incompliance, and disinterest or indifference of the patient seem further possible reasons. The possible impact of a limited follow-up rate of approximately 80% remains unclear and it remains hypothetical how this could have influenced the outcome of the present study. The population of the present study was characterized by patients with large isolated full-thickness cartilage defects of the knee who were eligible for ACI. Both average age at time of surgery (32.6 years) and defect size (4.9 cm2) are well comparable to other ACI studies, and therefore seem representative.
Patients expectations concerning postoperative clinical outcome have been evaluated in the first item of the questionnaire. Those expectations seem to be quite demanding and high. Only 1 patient of the entire study population expected a delay of a total joint replacement by the ACI procedure. This low percentage of patients demonstrates that ACI is not considered a salvage procedure in osteoarthritis. Even the percentage of patients who expected a persistence of pain and only reduction of pain after ACI was very low (12.7%), which underlines this estimation. The vast majority of patients expected a minimum of pain-free everyday life as a result of the ACI surgery (86%) with or without additional sporting activity. More than 70% of patients expected pain-free sports participation as clinical outcome following ACI. Among those patients, almost one third of patients (n = 24), representing approximately 20% of the entire study population, expected pain-free sports participation at high-impact level, such as basketball, soccer, and handball, as a result of the ACI. These expectations differ dramatically from what has been reported in patients who undergo total knee replacement for osteoarthritis.25,26 Although the present study was not designed to evaluate the surgeon’s expectation separately, the high expectations reported by the patients are probably higher than what surgeons expect from ACI. This interesting observation has also been reported for other treatments such as total knee and hip replacement.15
With regard to earlier published ACI studies, success rates are generally described either by an improvement in clinical function (in general evaluated by standardized scoring systems) or by the proportion of good and excellent results also defined by a standardized score. According to these definitions, the success rates of most relevant ACI studies vary between 80% and 95%. These success rates also have to be considered with regard to the observation that the patient population in most high-quality studies does not represent the reality to full extend.27 In addition, in order to achieve a good or excellent result in standard scoring systems, pain-free sports activity is generally not mandatory. Participation in sports activity has also been addressed in various studies, but success rate in terms of return to sports rates or return to preinjury level is not as high as the percentage of good and excellent score reported in literature. Previously, Mithoefer and coworkers evaluated all data available on ACI and postoperative sports activity for different cartilage repair techniques.28 They found a 71% rate of return to preinjury level of these patients by evaluating studies including 362 ACI patients. Although continued sports activity as a parameter of durability (96%) and mean Tegner score was highest in the group of ACI, these data demonstrate that highly competitive sports and high-impact sports following ACI seems realistic but the ability to perform high-impact sports is not achieved in every patient. Against this background, patient expectations need to be analyzed.
The second question, which was under investigation in the present study, was to evaluate the opinion of the patients about what is most important for clinical outcome. This question seems important against the background that some issues related to the ACI procedure, for example, rehabilitation, are directly influenced by patient’s compliance and probably directly related to the motivation of the individual patient. There are no reliable scientific data available that quantify the patient’s estimation concerning the relevance of the individual parameters such as defect size and location, patient compliance, individual risk factors (i.e., smoking or an increased BMI), cell quality as well as quality of the surgical treatment and postoperative rehabilitation. Interestingly, the initial individual pathology (defect size and defect location) is considered most relevant in the majority of patients (55.1% of all patients). Because defect size and location are described as relevant factors that influence clinical outcome, this estimation seems realistic and correct. Individual patient-specific parameters are obviously considered the most important factors for clinical outcome. According to the estimation of the patients involved in the present study, those characteristics contribute approximately 29.2% (SD = 19.2) to the clinical outcome following ACI. The second most relevant parameter concerning success of the ACI was the quality of the surgery itself. This is considered the most important parameter by 19.5% of the patients and contributes to the final results to more than 20%. The parameter cell quality has been addressed because some recent studies demonstrated that quality of the transplanted cells seems to influence clinical outcome.3,4,29 This parameter has been considered most relevant by only 10.2% of the patients. The significance of cell quality concerning the estimation of the patients on clinical outcome following ACI is approximately in the same range as the estimation of the importance of rehabilitation; this has only been indicated by 7.6% of the patients. Without being able to proof this by scientific data, according the estimation of the authors, the importance of postoperative rehabilitation clearly seems to be underestimated. This observation is also considerable against the background of an increasing number of publications on the topic of rehabilitation following ACI. This illustrates that various experts in the field of cartilage repair have increased their focus on the issue of postoperative rehabilitation.30-32
Results of the present study also illustrate that some recent studies on ACI are not well known by the patients, even if the knowledge of patients about their surgeries probably has increased because more and more information is available from the world wide web. Although various studies underline the influence of prior surgeries on the clinical outcome of ACI, only 4% of the patients involved in the present study consider this parameter most important for clinical outcome and by all patients this parameter was estimated to influence overall outcome by an amount of approximately 5%. Again, this parameter seems to be underestimated by patients before ACI.
As last item of the present study, patients were asked about the estimated time from surgery until final maturation and differentiation of the transplanted tissue. Scientific studies demonstrate that this process takes up to 24 months31,33 following the ACI procedure. Patients included in the present study estimated a period of 13.25 months (SD = 8.00) until the final regenerative cartilage tissue is differentiated, which is a clear underestimation because this is about half of the period of time as demonstrated in experimental studies.
Together with the fact that quality of the surgery is considered most important for clinical outcome contributes to the impression that there is a tendency to overestimate the surgery itself and to underestimate rehabilitation and time after surgery that is needed to return to everyday life and sports activity.
As possible limitation of the present study, time of data evaluation needs to be discussed. In contrast to other therapies, such as total joint replacement, ACI is not that popular and well known among patients. As a consequence, not every patient who presents with a cartilage defect is aware of this concept, which takes away the chance to evaluate patients before any contact with the treating surgeon. Data evaluation following the initial presentation is majorly influenced by the information given by the treating surgeon. In addition, it is almost impossible to standardize this information, because it really depends on the background of an individual patient and also the patient’s questions. Therefore, initial information given to the patients at the time of its first presentation in the hospital certainly varies in between individual patients. With regard to this, an optimal time for data evaluation concerning the expectation of patients prior to ACI is not available. For this reason, in the present study, patients were evaluated following the ACI procedure. Because it is well known, and because patients were informed, that the clinical course following ACI is quite long including the need of a long rehabilitation period,31 and that it takes up to 2 to 3 years until a final regenerative tissue is achieved,34 patient expectation should not change significantly within the early clinical course following ACI. This gives the chance to evaluate patient’s expectations. Nevertheless, certainly the surgery itself and early complications might influence the expectations of patients with regard to this time of data evaluation. Therefore, the time of data evaluation needs to be considered when interpreting the results of the present study. Realistically, this possible influence should lead to even lower expectations of patients. Because expectations in the present study seem really demanding and high, a relevant influence of time of data evaluation on the results of the present study seem unlikely. Nevertheless, it could also be of interest to evaluate the patient’s expectation immediately before and after surgery and to compare it with their expectations during the further clinical course following ACI.
In conclusion, the expectations of patients before ACI are demanding and quite high. Obviously the technique is generally considered to restore pain-free sports participation, but it seems that patients are not aware of all factors that are of possible importance concerning clinical outcome. Especially, time required for maturation of the regenerative tissue and rehabilitation seems underestimated. All these factors should be discussed with the patients prior to ACI in order to better inform and create realistic expectations of the postoperative benefit.
Footnotes
The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331(14):889-95. [DOI] [PubMed] [Google Scholar]
- 2. Cole BJ, Pascual-Garrido C, Grumet RC. Surgical management of articular cartilage defects in the knee. J Bone Joint Surg Am. 2009;91(7):1778-90. [PubMed] [Google Scholar]
- 3. Saris DB, Vanlauwe J, Victor J, Almqvist KF, Verdonk R, Bellemans J, et al. Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med. 2009;37(Suppl 1):10S-9S. [DOI] [PubMed] [Google Scholar]
- 4. Saris DB, Vanlauwe J, Victor J, Haspl M, Bohnsack M, Fortems Y, et al. Characterized chondrocyte implantation results in better structural repair when treating symptomatic cartilage defects of the knee in a randomized controlled trial versus microfracture. Am J Sports Med. 2008;36(2):235-46. [DOI] [PubMed] [Google Scholar]
- 5. Basad E, Ishaque B, Bachmann G, Sturz H, Steinmeyer J. Matrix-induced autologous chondrocyte implantation versus microfracture in the treatment of cartilage defects of the knee: a 2-year randomised study. Knee Surg Sports Traumatol Arthrosc. 2010;18(4):519-27. [DOI] [PubMed] [Google Scholar]
- 6. Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Isaksen V, Ludvigsen TC, et al. A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am. 2007;89(10):2105-12. [DOI] [PubMed] [Google Scholar]
- 7. Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grontvedt T, Solheim E, et al. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am. 2004;86-A(3):455-64. [DOI] [PubMed] [Google Scholar]
- 8. Peterson L, Vasiliadis HS, Brittberg M, Lindahl A. Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med. 2010;38(6):1117-24. [DOI] [PubMed] [Google Scholar]
- 9. Moseley JB, Jr, Anderson AF, Browne JE, Mandelbaum BR, Micheli LJ, Fu F, et al. Long-term durability of autologous chondrocyte implantation: a multicenter, observational study in US patients. Am J Sports Med. 2010;38(2):238-46. [DOI] [PubMed] [Google Scholar]
- 10. Vasiliadis HS, Danielson B, Ljungberg M, McKeon B, Lindahl A, Peterson L. Autologous chondrocyte implantation in cartilage lesions of the knee: long-term evaluation with magnetic resonance imaging and delayed gadolinium-enhanced magnetic resonance imaging technique. Am J Sports Med. 2010;38(5):943-49. [DOI] [PubMed] [Google Scholar]
- 11. Bhosale AM, Kuiper JH, Johnson WE, Harrison PE, Richardson JB. Midterm to long-term longitudinal outcome of autologous chondrocyte implantation in the knee joint: a multilevel analysis. Am J Sports Med. 2009;37(Suppl 1):131S-8S. [DOI] [PubMed] [Google Scholar]
- 12. Brittberg M. Autologous chondrocyte implantation—technique and long-term follow-up. Injury. 2008;39(Suppl 1):S40-9. [DOI] [PubMed] [Google Scholar]
- 13. Marlovits S, Zeller P, Singer P, Resinger C, Vecsei V. Cartilage repair: generations of autologous chondrocyte transplantation. Eur J Radiol. 2006;57(1):24-31. [DOI] [PubMed] [Google Scholar]
- 14. Krishnan SP, Skinner JA, Bartlett W, Carrington RW, Flanagan AM, Briggs TW, et al. Who is the ideal candidate for autologous chondrocyte implantation? J Bone Joint Surg Br. 2006;88(1):61-4. [DOI] [PubMed] [Google Scholar]
- 15. Moran M, Khan A, Sochart DH, Andrew G. Expect the best, prepare for the worst: surgeon and patient expectation of the outcome of primary total hip and knee replacement. Ann R Coll Surg Engl. 2003;85(3):204-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. J Arthroplasty. 2009;24(5):716-21. [DOI] [PubMed] [Google Scholar]
- 17. Iversen MD, Daltroy LH, Fossel AH, Katz JN. The prognostic importance of patient pre-operative expectations of surgery for lumbar spinal stenosis. Patient Educ Couns. 1998;34(2):169-78. [DOI] [PubMed] [Google Scholar]
- 18. Gonzalez Saenz de Tejada M, Escobar A, Herrera C, Garcia L, Aizpuru F, Sarasqueta C. Patient expectations and health-related quality of life outcomes following total joint replacement. Value Health. 2010;13(4):447-54. [DOI] [PubMed] [Google Scholar]
- 19. Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29(6):1273-9. [PubMed] [Google Scholar]
- 20. Mancuso CA, Graziano S, Briskie LM, Peterson MG, Pellicci PM, Salvati EA, et al. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties. Clin Orthop Relat Res. 2008;466(2):424-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(Suppl 2):58-69. [DOI] [PubMed] [Google Scholar]
- 22. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35-43. [DOI] [PubMed] [Google Scholar]
- 23. Hepinstall MS, Rutledge JR, Bornstein LJ, Mazumdar M, Westrich GH. Factors that impact expectations before total knee arthroplasty. J Arthroplasty. 2011;26(6):870-6. [DOI] [PubMed] [Google Scholar]
- 24. van den Akker-Scheek I, van Raay JJ, Reininga IH, Bulstra SK, Zijlstra W, Stevens M. Reliability and concurrent validity of the Dutch hip and knee replacement expectations surveys. BMC Musculoskelet Disord. 2010;11:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Suda AJ, Seeger JB, Bitsch RG, Krueger M, Clarius M. Are patients’ expectations of hip and knee arthroplasty fulfilled? A prospective study of 130 patients. Orthopedics. 2010;33(2):76-80. [DOI] [PubMed] [Google Scholar]
- 26. Nilsdotter AK, Toksvig-Larsen S, Roos EM. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop. 2009;80(1):55-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Engen CN, Engebretsen L, Aroen A. Knee cartilage defect patients enrolled in randomized controlled trials are not representative of patients in orthopedic practice. Cartilage. 2010;1(4):312-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mithoefer K, Hambly K, Della Villa S, Silvers H, Mandelbaum BR. Return to sports participation after articular cartilage repair in the knee: scientific evidence. Am J Sports Med. 2009;37(Suppl 1):167S-76S. [DOI] [PubMed] [Google Scholar]
- 29. Pietschmann MF, Horng A, Niethammer T, Pagenstert I, Sievers B, Jansson V, et al. Cell quality affects clinical outcome after MACI procedure for cartilage injury of the knee. Knee Surg Sports Traumatol Arthrosc. 2009;17(11):1305-11. [DOI] [PubMed] [Google Scholar]
- 30. Assche DV, Caspel DV, Staes F, Saris DB, Bellemans J, Vanlauwe J, et al. Implementing one standardized rehabilitation protocol following autologous chondrocyte implantation or microfracture in the knee results in comparable physical therapy management. Physiother Theory Pract. 2011;27(2):125-36. [DOI] [PubMed] [Google Scholar]
- 31. Hambly K, Bobic V, Wondrasch B, Van Assche D, Marlovits S. Autologous chondrocyte implantation postoperative care and rehabilitation: science and practice. Am J Sports Med. 2006;34(6):1020-38. [DOI] [PubMed] [Google Scholar]
- 32. Wondrasch B, Zak L, Welsch GH, Marlovits S. Effect of accelerated weightbearing after matrix-associated autologous chondrocyte implantation on the femoral condyle on radiographic and clinical outcome after 2 years: a prospective, randomized controlled pilot study. Am J Sports Med. 2009;37(Suppl 1):88S-96S. [DOI] [PubMed] [Google Scholar]
- 33. Brittberg M. Cell carriers as the next generation of cell therapy for cartilage repair: a review of the matrix-induced autologous chondrocyte implantation procedure. Am J Sports Med. 2010;38(6):1259-71. [DOI] [PubMed] [Google Scholar]
- 34. Breinan HA, Minas T, Hsu HP, Nehrer S, Sledge CB, Spector M. Effect of cultured autologous chondrocytes on repair of chondral defects in a canine model. J Bone Joint Surg Am. 1997;79(10):1439-51. [DOI] [PubMed] [Google Scholar]