Figure 2.
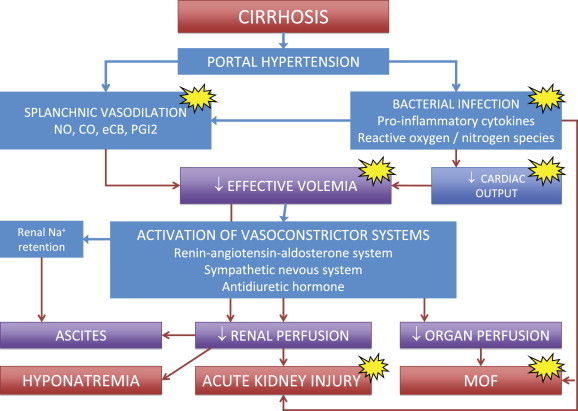
Schematic representation of the main pathophysiological events leading to renal sodium and water retention, ascites, hyponatremia, hepatorenal syndrome and multiorgan failure (MOF) in cirrhosis. Patients with cirrhosis are characterized by peripheral, mainly splanchnic, vasodilation, due to portal hypertension and a low-grade but sustained inflammatory state secondary to the intestinal translocation of bacteria and bacterial products. The ensuing reduction in effective volemia evokes the activation of vasoconstrictor and sodium and water retaining systems aimed at compensation through renal fluid retention and increased cardiac output. However, compensation is only partial and these changes lead to adverse effects, such as ascites formation and reduced renal perfusion that represents the background for dilutional hyponatremia and acute kidney injury. In this setting, the storm of pro-inflammatory cytokines and reactive oxygen and nitrogen species provoked by bacterial infections further enhances vasodilation, depresses cardiac function and endanger microcirculation potentially leading to multiorgan failure. The clinical use of albumin should aim not only at enhancing effective hypovolemia, but also at exploiting its antioxidant, scavenging and immunomodulating activities (yellow spots).
