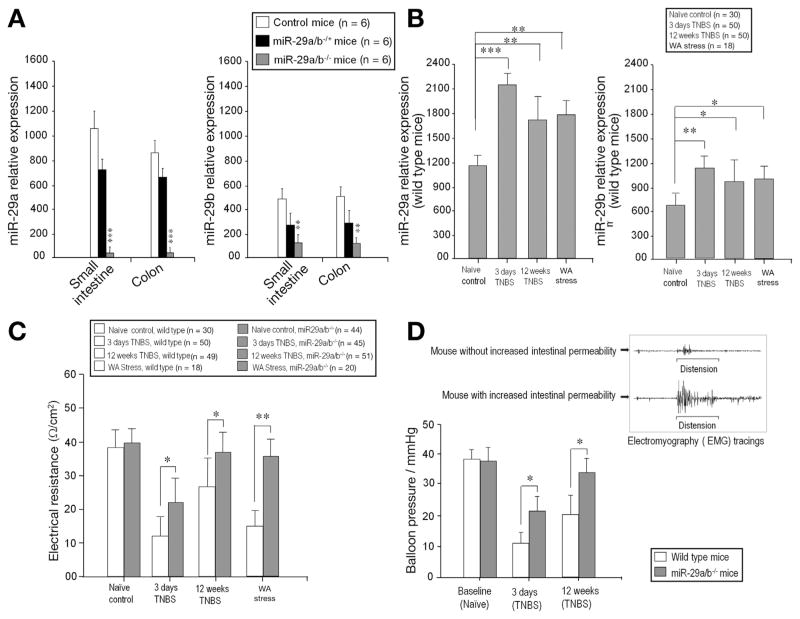
Figure 2.
In vivo deletion of miR-29 prevents intestinal hyperpermeability. Real-time PCR generated from 6 WT, 6 miR-29a/b−/+ (heterozygous) mice, and 6 miR-29a/b−/− (homozygous) mice. (A) There was significantly diminished miR-29a expression (left panel) in the small intestine and colon of miR-29a/b−/− mice compared with control and miR-29a/b−/+ mice (***P < .0001). There was significantly diminished miR-29b expression (right panel) in miR-29a/b−/− mice compared with control and miR-29a/b−/+ mice (**P < .001). (B) TNBS colitis (3 days, 12 weeks) and WAS resulted in up-regulation of miR-29a and miR-29b expression in WT mouse colon tissue. (C) There was increased intestinal permeability (decreased intestinal electrical resistance) after TNBS colitis or WAS. (D) Left: Depicts decreased visceral hypersensitivity in miR-29a/b−/− mice compared with WT after TNBS. Right: Electromyographic (EMG) tracing of mouse abdominal wall muscles shows increased in EMG activity after colonic distension in mice with increased intestinal permeability (lower tracing) compared with mice with normal intestinal permeability (upper tracing) after TNBS.