Abstract
Purpose
The purpose of this study is to assess the extant literature on instruments used to measure self-efficacy in youth with type 1 diabetes (T1DM) and their caregivers and to critically evaluate these measurements.
Methods
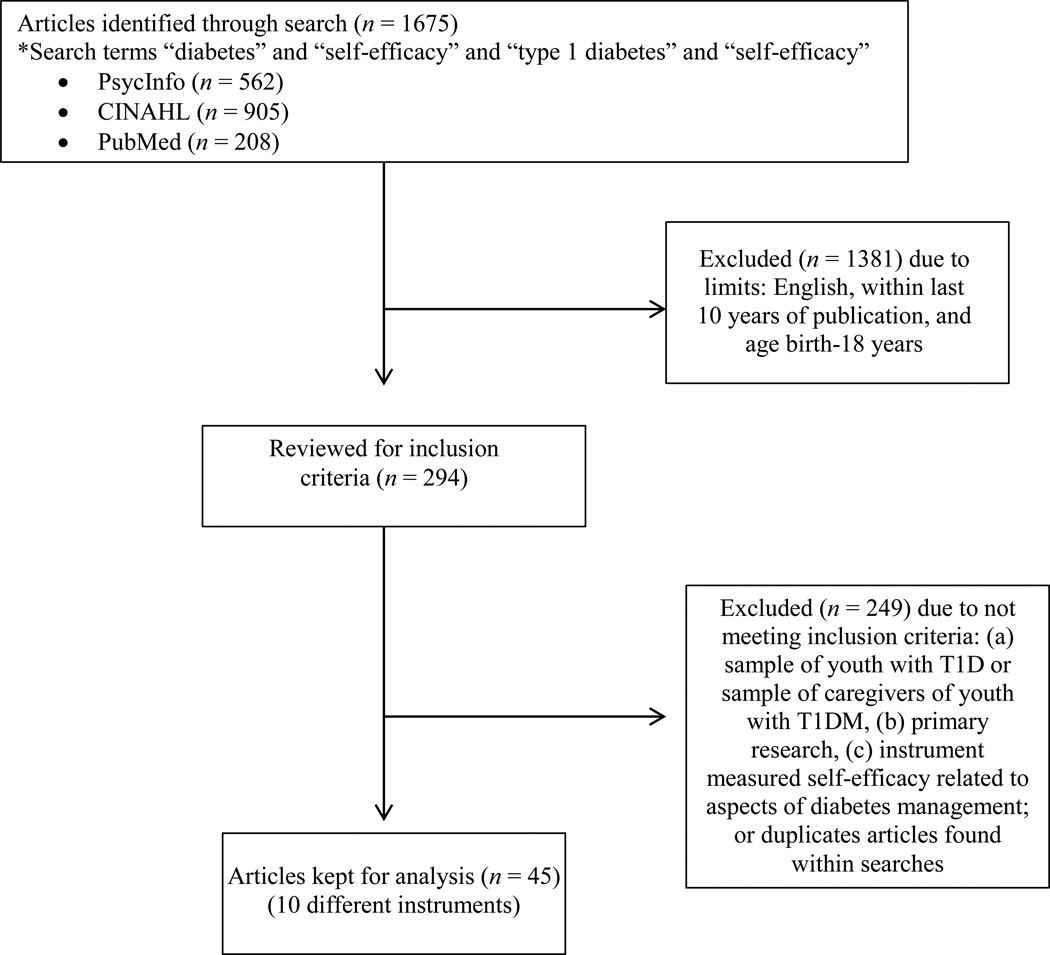
An integrative review (2003–2013) was conducted searching PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and U.S. National Library of Medicine PubMed service (PubMed) databases using key words diabetes, type 1 diabetes, and self-efficacy. The authors reviewed the resulting294 references for inclusion criteria of (a) sample of youth with T1DM or sample of caregivers of youth with T1DM, (b) description of the self-efficacy instrument as primary research, and (c) the instrument measured self-efficacy specifically related to diabetes management. Forty-five articles out of the initial 294 met criteria.
Results
Of the 45 articles, 10 different self-efficacy instruments were identified. The primary theoretical framework used was Bandura’s social cognitive theory and model of self-efficacy. Most participants were white middle class T1DM youth. Evaluations to assess validity often were not reported; however, a majority of studies reported high internal consistency of the instruments.
Conclusions
Sample homogeneity could limit the applicability of results to certain patient populations. Further psychometric analysis, including validity assessments, should be conducted in more diverse samples. Development of valid and reliable instruments for measuring self-efficacy that are sensitive to change across a wider caregiver base over time is necessary. While this review examined reliable and valid instruments used in research, future opportunities include evaluation of measuring self-efficacy in T1DM youth exposed to recent advances in diabetes management technologies.
Adhering to rigorous type 1 diabetes (T1DM) management during the complex stages of normal growth and development in childhood and adolescence is a significant challenge that impacts both youth with diabetes and their parents/guardians. Improved intensive therapy options can add to these challenges, as currently available therapeutic advances require self-management. Despite these improvements and a well-established correlation between adequate glucose control and reduced risk of complications, youth with T1DM often fail to meet the suggested A1C targets necessary to mitigate associated risks.1–4 Enhanced diabetes self-efficacy has been linked to improved diabetes self-care and glycemic control and is an important indicator of health behavior changes in youth.5,6 Self-efficacy, or one’s perceived ability to follow a diabetes treatment program, is important to foster in T1DM youth and their caregivers given the demands of diabetes self-management.7 Therefore, it is important for diabetes educators to understand the concept of self-efficacy and what measures are available to assess self-efficacy in youth with T1DM. The purpose of this integrative review was to identify measurement instruments to assess self-efficacy in youth with T1DM and to evaluate the reported psychometric properties of those instruments.
Theoretical and operational definitions allow for greater understanding and means to measure self-efficacy.8 A theoretical definition of self-efficacy includes the belief that an individual has the ability to create change by personal actions.9 In T1DM, operational definitions are informed by data from self-report surveys that assess one’s level of confidence or self-efficacy to accomplish diabetes management tasks, such as blood glucose monitoring, insulin administration, and attention to diet and exercise, in everyday living and in difficult situations that may occur. Self-efficacy is important to capture in youth with T1DM because higher levels of diabetes specific self-efficacy may result in increased resilience when youth face barriers or challenges associated with diabetes self-management.6 Therefore, ongoing work to measure and optimize self-efficacy in youth with T1DM is necessary to equip youth to manage this disease long-term. This can be particularly important during transition periods across the lifespan of childhood as diabetes management gradually transitions from parents to older children and adolescents and then becomes the sole responsibility of college aged youth or young adults living on their own.
Methods
The literature search focused on (a) identifying instruments used to measure the construct of self-efficacy in youth with T1DMand their parents and (b) evaluating the reported psychometric properties of those instruments. For an appropriate literature search, at least two different search strategies are necessary according to Whittemore and Knafl’s integrative review methodology.10 This literature search used PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and U.S. National Library of Medicine PubMed service (PubMed) to obtain applicable articles. Search engines from nursing, psychology, allied health, and medical literature provided the opportunity to assess the measurement of self-efficacy across disciplines. Because of the unique attributes of T1DM disease management in this particular population, the search focused on studies of youth with T1DM. Additionally, the search included articles across all pediatric age groups and their caregivers involved in the care and management of T1DM. International literature that was translated into English was retained because evaluating the concept across geographies could add a valuable cultural perspective. This search included articles measuring specific areas of self-efficacy within diabetes management (healthy eating, being active, monitoring, taking medication, problem solving, reducing risks, and healthy coping, which are the seven self-care behaviors guiding diabetes education).11 To obtain a contemporary perspective on available instruments, only primary research published between 2003 and 2013 was included.
Figure 1 presents an overview of the literature search and is a CONSORT flow diagram of the search methodology.12 The first database search occurred with PsycINFO. An initial search included the terms “diabetes” and “self-efficacy”, and an additional search included the terms “type 1 diabetes” and “self-efficacy”. The investigators conducted searches with both diabetes and type 1 diabetes to ensure comprehensiveness. Limits of “English, last 10 years of publication, and childhood age (birth-17 years)” were applied. The age limit for the PsycINFO search ended at 17 instead of 18 years because 18 years and older is classified as adulthood in this search engine. The results were evaluated for applicability, availability, and relevance; a total of 28 articles met inclusion criteria. The second database search occurred with CINAHL and included combined searches with “diabetes” and “self-efficacy” as well as “type 1 diabetes” and “self-efficacy”. After applying the limits of “English, last 10 years of publication, and ages birth-18 years”, this search identified 16 articles that met inclusion criteria and were not duplicates from the prior search. A third search occurred in PubMed and included the MeSH terms “diabetes mellitus” and “self-efficacy” and then “type 1 diabetes” and “self-efficacy”. To add precision to the search, the authors specified the MeSH term “self-efficacy” as a major term. Adding the limits of “English, last 10 years of publication, and agesbirth-18 years” yielded one additional article that was not a duplicate from prior searches. The search provided a total of 45 articles that discussed the use of 10 instruments for measuring self-efficacy in youth with T1DM and/or their caregivers.
Figure 1.
Flow diagram of the search process
Tables 1 to 3 contain matrices of relevant articles categorized by type of self-efficacy instrument with particular attention to study sample, instrument characteristics, and instrument psychometrics. The Oxford Centre for Evidence-based Medicine-Levels of Evidence was used to evaluate each study based on study design and analysis.13 Two of the investigators (LR and CJ) evaluated each study to determine the level of evidence and to establish inter-rater reliability. The level of agreement was 100 percent.
Table 1.
Instruments Used to Measure Self-Efficacy in T1DM Youth and Caregivers
| Instrument/ Reference |
Instrument Description/Scoring | Comments |
|---|---|---|
| Self-Efficacy for Diabetes Scale (SED)7,16,24,25,28,29,33–42,53,55,56 | Instrument: 3 subscales: diabetes-specific self-efficacy (24 items), medical situations self-efficacy (5 items), general situations (6 items) questionnaire assessing perceived self-efficacy to manage T1DM28; Likert-like response categories 1–5 with “1 = very sure I cannot” to “5 = very sure I can”34,37,41,42,53,55,56 or “1 = very sure I can” to “5 = very sure I can’t”16 or a 6-point Likert-like scale24,25,33,35 or a 5-point Likert scale with 0–4 “0 = very sure I can” to “4 = very sure I cannot”.40 Some studies report 12-item41 or 33-item25 instrument. Scoring: Scoring differed by study(ies). Total scores represented by mean item score.53 Higher scores reflect greater self-efficacy24,25,37,42,55,56 or more confidence.41 |
Modified to include current aspects of T1DM (pump
therapy).29 SED adapted for parent use with 22-items and youth parent dyads completed the survey.37,42 SED adapted for parent use only with 19-items.7,55,56 SED adapted for camp counselor use.41 |
| Self-Efficacy for Diabetes Self-Management (SEDM)£5,6,21–23,27,47–52 | Instrument: 10 item questionnaire assessing perceived self-efficacy to perform diabetes care behaviors with Likert-like response categories 1–10 with “1 = not at all sure” to “10 = completely sure”. One study used a scale ranging 1–5.52 Scoring: Scoring differed by study(ies) Higher scores indicating higher levels of self-efficacy.5,23,27,51,52 Youth and parent scores combined to measure family self-efficacy.5 |
Instrument adapted for use in youth-parent dyads (either mother, father, or both).5,22,23,50 |
| Diabetes Empowerment Scale (DES)7,26 | Instrument: 28 items composed of 3-subscales rating diabetes specific self-efficacy in managing psychosocial aspects of diabetes, assessing dissatisfaction, and readiness to change and setting and achieving diabetes goals, using 5-point Likert-like scale ranging from 1 = strongly agree to 5 = strongly disagree.26 Scoring: Mean scores provided in each study.7,26 |
One study used the DES in parents of youth with T1DM.7 |
| Diabetes-Specific Self-Efficacy Scale17,18,45,46 | Instrument: 7 items indicating confidence about ability; for each item, numbers converted to A+ = 100 “could not do better” to F = 20 “you are a disaster” using scale 20–100.18 8 item questionnaire assessing perceived related to diet, glucose monitoring, insulin administration, exercise, and hypoglycemia behaviors with grading A+ = 9 could not do better” to F = 1 “you are a disaster”46; Participant graded themselves on tasks with grade ranging from A+ to F with total score ranging 8–72.17,45 Scoring: Scoring differed by study. A+ was equal to a score of 9 and F equal to a score of 1 for each item with the total score being the sum.46 Higher scores indicate higher self-efficacy.17,18 |
Two studies used modified instrument adding item related to hypoglycemia to make total of 8-items.17,45,46 |
| Dietary Self-Efficacy Scale15,43,44 | Instrument: 9 items rating confidence about following dietary plan related to barriers of temptations, negative mood, and uncontrollable situations; 10-point scale ranging from 0 = not confident in following dietary plan to 10 = confident in following dietary plan43; adapted scale to measure confidence in dietary self-care activities with 26 items/common barriers, using 11-point Likert scale of 0 = not at all confident to 10 = totally confident.15,44 Scoring: Higher scores indicate more self-efficacy |
Adapted to use with adolescents and parents.44 |
| Perceived self-efficacy scale related to exercise30 | Instrument: 8 item questionnaire assessing beliefs about personal exercise capability, Likert-like response categories with “1 = not at all true” to “5 = very true”.30 Scoring: Mean of items calculated30 |
Survey assisted in development of exercise program and examined changes post intervention.30 |
| Diabetes self-efficacy scale31 | Instrument: 8 item questionnaire measuring level of self-confidence performing diabetes care-related tasks, 10-point semantic differential scale with “1 = not at all confident” to “10 = totally confident”.31 Scoring: Ratings summed and higher scores indicate greater self-efficacy31 |
|
| Perceived Diabetes Self-Management Scale32 | Instrument: 8 item questionnaire measuring confidence in managing glycemic control well, 5-point Likert-like scale with “1 = strongly disagree” to “5 = strongly agree”.32 Scoring: Four items reverse-scored, scores ranged 8–40 with higher scores indicating greater confidence.32 |
Survey was translated for current study.32 |
| Maternal Self-Efficacy for Diabetes Scale19 | Instrument: 17 item questionnaire to assess maternal self-efficacy in areas of illness, exercise, response to high or lower blood glucose, adjusting insulin doses, and acting as child’s advocate, 5-point Likert scale with “1 = not at all confident” to “5 = very confident without help”.19 Scoring: Not reported19 |
|
| Self-Efficacy in Diabetes Education20 | Instrument: 11 item questionnaire measuring self-efficacy about specific factors related to performing diabetes care and education in school setting, 5-point Likert scale with “1 = not at all confident” to “5 = completely confident”, stem “ I feel confidence with diabetes education when…”20 Scoring: Determined by adding responses of all questions, highest score 55 indicates complete confidence, score 44 high confidence, score 33 moderate confidence, 22 low confidence, lowest score 11 no confidence20 |
NOTE: A table summarizing each study is available from the author.
One study27 used the Diabetes Management Self-Efficacy Scale (DMSES) by Iannotti et al. (2004) from paper presented at the Society of Pediatric Psychology National Conference on Child Health Psychology.
Legend for abbreviations: Type 1 Diabetes (T1DM), Self-Efficacy for Diabetes Scale (SED), Self-Efficacy for Diabetes Self-Management (SEDM), Diabetes Empowerment Scale (DES)
Table 2.
Theoretical Framework and Sample Used in Articles Measuring Self-Efficacy
| Instrument/ Reference |
Theoretical Framework | Sample/Subjects |
|---|---|---|
| Self-Efficacy for Diabetes Scale (SED)7,16,24,25,28,29,33–42,53,55,56 | Self-efficacy theory7; Self-efficacy: Not stated but implied24,25; Stress adaptation model16,28,29; Social ecological model53; Bruhn and Parcel model of health promotion34; Social cognitive theory16; Biopsychosocial model36; Johnson’s biobehavioral model56; Transtheoretical model37; Self-regulation theory41; Not identified33,35,38–40,42,55 | Sample size: n = 147 to 51540 Subjects largely white or white and upper/middle income16,24,25,28,29,33,34,36,37,40–42,53,55,56 Age range across studies: 3.9–21 years old*16,24,25,28,29,33–42,53 Parents of youth with T1DM7,16,28,33,36,37,39,42,55,56 Adolescent camp counselors41 |
| Self-Efficacy for Diabetes Self-Management (SEDM)5,6,21–23,27,47–52 | Self efficacy: Not stated but implied21–23; Bandura’s Social Cognitive Theory6; Dyadic models of coping48; Risk and Resistance model of chronic illness adaptation27; Family organization5; Not identified47,49–52 | Sample size: n = 13749 to 76651 Subjects largely white and/or upper/middle income5,6,21–23,27,47–50,52 Age range across studies: 2–18 years old* Parents of youth with T1DM5,6,21–23,27,47–52 |
| Diabetes Empowerment Scale (DES)7,26 | Extended health belief model26; Self-efficacy theory7 | Sample size: n = 147 to 11826 Age range: 16–25 years old26 Parents of youth with T1DM7 |
| Diabetes-Specific Self-Efficacy Scale17,18,45,46 | Social cognitive perspective-self-efficacy17; Self-efficacy18; Not identified45,46 | Sample size: n = 5618 to 20417 Subjects were largely white or white and upper/middle income17,45,46 Age range across studies: 10–23 years old17,18,45,46 |
| Dietary Self-Efficacy Scale15,43,44 | Self-Determination Theory43; Leventhal, Meyer, and Nerenz’s self-regulatory model of illness representations15,44; Social-cognitive theory/self-efficacy15 | Sample size: n = 15115–28943 Age range across studies: 11–18 years old15,43,44 Parents of youth with T1DM44 |
| Perceived self-efficacy scale related to exercise30 | Personalized exercise prescription intervention model30 | Sample size: n = 1230 9 subjects non-Hispanic white, 3 subjects Hispanic; no SES data30 Age range: 12–19 years old30 Parents of youth with T1DM30 |
| Diabetes self-efficacy scale31 | Not identified31 | Sample size: n = 12331 Age range: 13–2531 |
| Perceived Diabetes Self-Management Scale32 | Not identified32 | Sample size: n = 5232 Age range: 12–20 years old32 |
| Maternal Self-Efficacy for Diabetes Scale19 | Self-efficacy19 | Sample size: n = 4119 Mothers of youth with T1DM19 |
| Self-Efficacy in Diabetes Education20 | Bandura’s Theory of Self-Efficacy20 | Sample size: n = 11520 School nurses at elementary and middle schools in suburban New England20 |
Youth as young as 8 years old completing surveys may alter results for adolescents16,28; youth as young as 8 years old interviewed for scale development6; study recruited families of youth with T1DM between ages of 2 and 17 years old; however, only adolescents ages 12 to 17 years old completed SEDM51
Legend for abbreviations: Type 1 Diabetes (T1DM), Self-Efficacy for Diabetes Scale (SED), Self-Efficacy for Diabetes Self-Management (SEDM), Diabetes Empowerment Scale (DES)
Table 3.
Assessment of Instruments Used to Measure Self-Efficacy in T1DM Youth and Caregivers
| Instrument/ Reference |
Validity of Instrument | Reliability of Instrument | Outcomes related to Self- Efficacy/Level of Evidence |
|---|---|---|---|
| Self-Efficacy for Diabetes Scale (SED)7,16,24,25,28,29,33–42,53,55,56 | Confirmatory factor analysis36; Used to establish construct validity for a novel instrument measuring diabetes self-management in adolescents40; No other evaluation for validity reported7,24,25,28,29,33–35,37–39,41,42,53,55,56 | Internal consistency: Cronbach’s α =.88 to .9434,35,41; diabetes subscale .84 to .9028,29,35; medical subscale .6035 and .7128; general subscale .5835 and .7028; α = .8416and .8740 for diabetes subscale only, .87 to .88 for parents only,55,56 .88 to .90,33,35,53; .90 for youth and parents37,42; reliability coefficient =.90 to .92 (unclear if established in this study or previous studies)39; not reported7,24,25,36,38 | Outcomes: Higher self-efficacy for female teens on pump
therapy compared to multiple daily injections24; more parental emotional support and maternal acceptance
associated with higher self-efficacy33,34; better diabetes
problem solving related to higher self-efficacy and youth self-efficacy predicted
youth responsibility for more diabetes management36; higher self-efficacy reported six months after starting pump
therapy38; higher maternal
self-efficacy associated with lower rates of health-care utilization by
youth42; positive relationship
between social support and self-efficacy in parents of T1DM youth, greater
self-efficacy found following web-based intervention to improve social support in
parents of T1DM youth.7 Critical parenting associated in lower self-efficacy in preteens, mediated by depressive symptoms53; lower self-efficacy mediated relationship between depressive symptoms and fewer self-care behaviors53; adolescents describing mothers as having firm control had worse self-efficacy33; parents reporting lower self-efficacy also reported more frequent pediatric parenting stress.56 Level of Evidence: 1b16,28,35,38,39,41; 2b7,24,29,33,34,36,37,40,42,53,55,56; 3b25 |
| (Self-Efficacy for Diabetes Self-Management SEDM)5,6,21–23,27,47–52 | Face validity assessed by developmental psychologists and pediatric endocrinologists6; Principal Component Factor Analysis reported6; Predictive validity determined through hierarchical regression analysis6; SEDM used as convergent validation of the Perceived Coping Effectiveness (PCE) measure48; SEDM used to establish concurrent validity with novel Adherence in Diabetes Questionnaire51; No other evaluation for validity reported5,21–23,27,47,49,50,52 | Test-retest reliability:.896 Internal consistency: Cronbach’s α = .906; α = .81 to .90,21–23,27,47,48,49.87 to .88 for mothers and .90 to .91 for fathers,22,23 .85 for youth and parents,5 .88 at baseline and .90 at 6 month for youth and .90 at baseline and .93 at 6 month for parents50; not reported51,52 |
Outcomes: Higher self-efficacy associated with diabetes
self-management adherence,6,51 good glycemic control,6 more collaboration between youth and
primary caregivers,27 patient
centered communication with their provider,50 blood glucose monitoring frequency,52 lower HbA1c and higher self-control.49 Higher perceived coping effectiveness associated with self-efficacy across age48 Self-efficacy is mediator for association between parental-teen relationship and diabetes management.21 Higher levels of family conflict associated with lower diabetes self efficacy.52 Level of Evidence: 2b5,6,21–23,27,47–52 |
| Diabetes Empowerment Scale (DES)7,26 | None reported 7,26 | Test-retest reliability:.7926 Internal consistency: Cronbach’s α = .87, .68, .91 for respective subscales (psychosocial aspects of diabetes, dissatisfaction, and readiness to change/achieving diabetes goals)26; None reported7 |
Outcomes: High levels of self-efficacy predicted the
benefits of adhering to self-care regimen26; no significant difference in parent DES scores after receiving a
web-based intervention to improve social support.7 Level of Evidence: 2b7,26 |
| Diabetes-Specific Self-Efficacy Scale17,18,45,46 | None reported17,18,45,46 | Internal consistency:Cronbach’s α =.85,17,45,46 .8618 | Outcomes: For youth living independently higher
self-efficacy associated with greater responsibility45; diabetes management better for youth with higher
self-efficacy.46 Lower
self-efficacy associated with greater responsibility for adolescents living at home
after high school.45 Level of Evidence: 2b17,18,45,46 |
| Dietary Self-Efficacy Scale15,43,44 | None reported15,43,44 | Internal consistency: Cronbach’s α =.86,43.95,15,44 .98 for parents44 | Outcomes: Dietary self-care positively and significantly
related to self-efficacy43; higher
levels of dietary self-efficacy associated with less perceived consequences of
diabetes and diabetes distress but stronger beliefs about the effects of dietary
self-care to control symptoms and greater dietary self-care.15 Adolescent diabetes distress related to lower
self-efficacy and dietary self-efficacy predicted adolescent diabetes
distress.44 Level of Evidence: 2b15,43,44 |
| Perceived self-efficacy scale related to exercise30 | None reported30 | None reported30 | Outcomes: Perceptual factors influencing adherence to
exercise was not strongly associated with exercise self-efficacy.30 Level of Evidence: 1b30 |
| Diabetes self-efficacy scale31 | None reported31 | Internal consistency: α = .7731 | Outcomes: No difference in self-efficacy between
rural/urban youth; higher diabetes self-efficacy, lower risk behavior, predicted
better diabetes self-care, which subsequently predicted better glycemic control and
mental health.31 Level of Evidence: 2b31 |
| Perceived Diabetes Self-Management Scale32 | None reported32 | Internal consistency: α = .8032 | Outcomes: Higher self-efficacy related to good metabolic
control and patients more likely to reach target diabetes control.32 Lower self-efficacy found in youth who
had longer diabetes duration.32 Level of Evidence: 2b32 |
| Maternal Self-Efficacy for Diabetes Scale19 | Content validity established from 2 parents of youth with diabetes and 3 nurse practitioners19 | Test-retest reliability: coefficient of stability = .7519 | Outcomes: Maternal coping resources significantly related
to maternal diabetes self-efficacy.19 No significant relationship between maternal self-efficacy and
maternal diabetes management behaviors.19 Level of Evidence: 2b19 |
| Self-Efficacy in Diabetes Education20 | Sent to 5 school nurse experts for content20 | Internal consistency: α = .9420 | Outcomes: Significant relationship between greater
self-efficacy and having a diabetes curriculum; significant positive relationships
between self-efficacy and participating in care of children with diabetes, having T1DM
youth in the school system, and supervising blood glucose monitoring.20 Level of Evidence: 2b20 |
Legend for abbreviations: Type 1 Diabetes (T1DM), Self-Efficacy for Diabetes Scale (SED), Cognitive Behavioral Therapy (CBT), Self-Efficacy for Diabetes Self-Management (SEDM), Diabetes Empowerment Scale (DES)
Legend for Levels of Evidence: 1a systematic review (SR) of randomized controlled trials (RCT)/inception cohort studies/diagnostic studies/prospective cohort studies/economic studies; 1b individual RCT, individual inception cohort study with >80% follow-up, validating cohort study, prospective cohort study with good follow-up; 1c all or none case series; 2a SR of cohort studies/retrospective cohort studies or untreated control groups in RCTs; 2b individual cohort study (including low quality RCT), retrospective cohort study, exploratory cohort study; 2c outcomes research/ecological studies; 3a SR of case-controlled studies; 3b individual case-control study, non-consecutive cohort study; 4 case-series; 5 expert opinion without critical appraisal.13
Results
Research Process
The authors summarized the results based on theoretical frameworks for the respective articles, sample characteristics, instrument descriptions, scoring, and psychometrics(Tables 1 to 3). Table 1 identifies and describes the various instruments and the identified studies, while Table 2 includes information about the theoretical framework and sample in each article, and Table 3 describes the psychometric details of the measurements and outcomes related to self-efficacy.
Theoretical frameworks
Theory driven measurement assigns meaning to a research question, clarifies associations between concepts, and gives researchers a guide to explore a specific concept.8,14 A lack of a theoretical framework in instrument development jeopardizes the ability to adequately measure a concept. Despite the importance of a theoretical framework, many of the articles analyzed in this integrative review did not identify a theoretical framework, as indicated in Table 2, column 2.
Of the 28 articles evaluating youth or caregiver self-efficacy that identified or implied a theory, the most common framework was Bandura’s social cognitive theory (SCT) or model of self-efficacy.6,7,15–20 Although not explicitly stated, an additional five studies implied Bandura’s model of self-efficacy.21–25
Less common, yet applicable, frameworks included the extended Health Belief Model(HBM),26 the risk and resistance model of chronic illness adaptation,27 and the stress-adaptation model.16,28,29 Each of these guiding models related to the construct of self-efficacy or patient/family adaptation to chronic disease management.
Sample and subjects
Since the purpose of this integrative review was to identify self-efficacy measures in youth with T1DM and their caregivers, all identified studies included a sample of children or adolescents or parents/caregivers. Many studies had youth ≥10 years old complete the various instruments; yet, a few had participants as young as 8 years old.16,28 Of the 45 articles in the review, 39 encompassed an adolescent age range of participants5,6,15–18,21–53 (10–18 years old as defined by the American Psychological Association),54 25 studies included parents as participants,5–7,16,19,21–23,27,28,30,33,36,37,39,42,44,47–52,55,56 and 11 studies measured parental self-efficacy in diabetes management5,7,19,37,42,55,56 or parental confidence in their child.22,23,44,50 One study measuring self-efficacy in diabetes care and education focused on the role of school nurses in diabetes management (including both T1DM and type 2 diabetes),20 and one focused on the role of camp counselors.41
An analysis of participant demographics revealed that31 studies had a homogenous sample that included white and/or middle-class participants.5,6,16,17,19,21–25,27–30,33,34,36,37,40–42,45–50,52,53,55,56 Additionally, 10 studies took place internationally, outside of the United States.15,18,26,31,32,35,38,43,44,51
Evaluation of Instruments
This integrative review identified 10 instruments to measure self-efficacy in youth with T1DM and their caregivers. Given the inclusion criteria of articles from the last decade (2003–2013), the initial literature search did not reveal the original articles that described all of the instruments. The following instruments were identified: a) Self-Efficacy for Diabetes scale (SED);b) Self-Efficacy for Diabetes Self-Management scale (SEDM);c) Diabetes Empowerment Scale (DES); d) Diabetes-Specific Self-Efficacy Scale; e) Dietary Self-Efficacy Scale; f) Perceived Self-Efficacy Scale related to exercise; g) Diabetes Self-Efficacy Scale; h) Perceived Diabetes Self-Management Scale (PDSMS); i) Maternal Self-Efficacy for Diabetes Management Scale; j) Self-Efficacy in Diabetes Education (SEDE). Of the 10 instruments, four were used in youth,17,18,30–32,45,46 three were used in youth/parents,5–7,15,21–23,26,27,43,44,47–52 one was used in youth/parents/camp counselors,7,16,24,25,28,29,33–42,53,55,56 one was used in mothers,19 and one was used in school nurses.20 The most commonly used instruments were the original and adapted SED7,16,24,25,28,29,33–42,53,55,56 and the original and adapted SEDM.5,6,21–23,27,47–52 One study used two instruments, the SED and the DES, to measure parental self-efficacy.7
Instrument description
All instruments used either a Likert-like scale or a semantic differential scale,57 except the Diabetes-Specific Self-Efficacy Scale, which used scoring from 20 (F) to 100 (A+) to evaluate perceived self-efficacy. The instruments ranged from 7 to 35 items with two of the surveys (SED and DES) consisting of three different subscales within the self-efficacy measurement. The SED included subscales for diabetes, medical, and general situations. The three DES subscales included managing psychosocial aspects of diabetes, assessing dissatisfaction, and readiness to change/goal setting. While all questionnaires assessed perceived self-efficacy related to confidence in diabetes management, one instrument explicitly measured dietary self-efficacy,15,43,44 another measured exercise self-efficacy,30 and one assessed confidence in diabetes education,20 Surprisingly, only one study described modifying an instrument (SED) to incorporate pump therapy.29 The literature search did not identify other measures that assessed youth self-efficacy related to current technologies, e.g. pump therapy or continuous glucose monitoring.
Measurement of perceptions and scoring
The instruments’ response categories ranged from five- to eleven-point Likert-like scales and varied as to whether low or high scores indicated less or greater self-efficacy. All articles discussed how scoring related to the level of self-efficacy and/or provided the mean participant scores with the respective instruments. One study using the SEDM survey combined youth and parent scores to evaluate family self-efficacy,5 although this combination in scoring differed from the original description of the instrument.6
Method of administration
The method and site for instrument completion varied, ranging from the clinical or camp setting to completion by mail, the web, or telephone; some studies utilized more than one approach. The majority of studies had participants complete the instruments at the time of a medical or study visit.5,16,18,21,23,24,27,28,31,32,35–37,39,40,42,43,47,48,50,52,56 The second most frequent method of administration was via the mail6,7,15,20,22,26,33,49,55 followed by the web.17,29,45,46,51
Reliability
Most articles reported reliability statistics for the self-efficacy instrument under study. Although certain studies may not have explicitly stated reliability or validity data, the psychometrics from the original studies prior to 2003 were identified; however, caution is warranted when applying these psychometrics to different samples. Most studies using the SED or an adapted version of the scale reported internal consistency for the diabetes specific subscale16,29,40 or total scale33–35,37,39,41,42,53,55,56 with α values ranging from .84–.94, indicating a high internal consistency. Cronbach’s α values of .70 and greater are considered acceptable.58 Other studies using all 3 subscales of the SED reported α values of .84 and .90 for the diabetes subscale, .60 and .71 for the medical subscale, and .58 and .70 for the general subscale.28,35 The original article by Grossman and colleagues cited a Kuder-Richardson coefficient α of .90 for the total scale, .92 for the diabetes subscale, as well as significant intercorrelations among the scales in a study sample of 68 adolescents with T1DM.59
Studies using the SEDM scale revealed high alpha coefficients ranging from .81–.93.5,6,21–23,27,47–50 Adapted versions of the SEDM used in parents as well as youth performed well, with high levels of internal consistency for parents (α = .85–.93)5,22,23,50 and slightly lower levels for youth (α = .81–.90).5,22,23,50 The DES demonstrated internal consistency across the three subscales of psychosocial aspects (α = .87), dissatisfaction (α = .68), and readiness to change/goal setting (α = .91),26 which were slightly lower than the original assessments of the total scale (α = .96) and subscales of psychosocial aspects (α = .93), dissatisfaction (α = .81), and achieving goals (α = .91).60 The Diabetes Specific Self-Efficacy Scale reported Cronbach’s α of .8517,45,46 and .86,18 which was higher than the originally reported .78.61 The Dietary Self-Efficacy Scale also reported high internal consistency with Cronbach’s α of .8643 and 0.9515,44 for youth and .98 for parents,44 while the original Dietary Self-Efficacy Scale reported a Cronbach’s α of .94.62 All but one of the studies representing the remaining five self-efficacy scales reported reliability information for the current study participants. The study using the Perceived Self-Efficacy Scale related to exercise reported reliability coefficients from past studies only.30 The internal consistencies for the Diabetes Self-Efficacy Scale, the PDSMS, and the SEDE survey ranged from α = .77–.94.20,31,32 The original PDSMS reported a relatively high internal consistency with a Cronbach’s α of .83 in a sample of adults with T1DM or type 2 diabetes (T2DM).63 Similarly, the original report of Diabetes Self-Efficacy Scale had an α of .85 in a sample of adults with T2DM.64
Test-retest reliability was reported for the Maternal Self-Efficacy for Diabetes Management Scale, with a 37% response rate in repeating the measure after two weeks and a modest correlation of .75,19 and was reported for the DES with test-retest reliability of .7926. In the original study, researchers expanded the SEDM psychometrics by establishing test-retest reliability6; they administered the survey twice in 1 week to 38 youth, revealing a test-retest intra-class correlation coefficient of .89, reflecting the stability of the scale over time.65 The original Perceived Self-Efficacy related to exercise scale also reported reliability using the test-retest method with a result of 0.98966 and the original Diabetes Self-Efficacy Scale reported a test-retest of .80.64
Validity
A few of the articles reported content and face validity of the self-efficacy instruments. Content validity was established by consulting school nurses as experts for the SEDE instrument20 and parents of youth with diabetes plus nurse practitioners for the Maternal Self-Efficacy for Diabetes Management Scale.19,67 Similarly, nine family interviews and consultation with experts in developmental psychology and pediatric endocrinology established face validity for the original SEDM scale.6
Factor analysis was another approach to establish validity. In one article using the SED, the researchers performed a confirmatory factor analysis among variables that included self-efficacy to determine the strength of relationships among the variables.36 In the original publication of SEDM scale, the authors reported extensive validity metrics, including factor analysis and predictive validity.6 They identified significant although modest correlations between the SEDM scale and glycemic control (r = .21) and the youth (r = .37) and parent (r = .29) report on the Diabetes Self Management survey.6 The original article describing the DES reported a single factor for the measure.61
Other articles described construct, convergent, and concurrent validity. One study used the SED to establish construct validity for the survey measuring diabetes self-management, the Self-Management of T1DM in Adolescents.40 Although not directly related to the validity of the SEDM scale, one study used this instrument to establish convergent validity for another measure, Perceived Coping Effectiveness (PCE),48 and another study used the SEDM survey to establish concurrent validity with an Adherence in Diabetes Questionnaire.51
To identify other validity assessments, one must evaluate the original articles describing the self-efficacy instruments. The initial article using the SED reported evidence for criterion and construct validity for this measure59 while the original DES article reported evidence for concurrent validity.60 The original article describing the PDSMS also reported sufficient establishment of construct validity.63 Pender and colleagues reported predictive validity, which was established with significant correlations with other variables for the Perceived Self-Efficacy Scale related to exercise.66 The original Dietary Self-Efficacy article did not describe a validity assessment.62
Feasibility of instrument use
The identified studies did not readily discuss the feasibility of implementation of the instruments.8 In some cases, authors identified compensation amounts for study participation or the time required for completion; however, the time reported often involved completion of multiple questionnaires, not just the self-efficacy instrument. Therefore, it is difficult to ascertain how long each measure takes to complete. However, Table 1 lists the number of items per survey. Access to the instrument is another feasibility consideration. On an initial search, the majority of surveys do not seem readily available within the public domain and often require identifying the original article describing the instrument. The following instruments are publicly accessible: the DES is accessible on the Michigan Diabetes Research and Training Center website,68 the Perceived Self-Efficacy Scale related to exercise30 and the Diabetes Self-Efficacy Scale31 are available through websites noted in the studies’ reference lists. The SEDM and PDSMS items are listed as tables in the original studies.6,63 Additionally, the original studies describing the Maternal Self-Efficacy for Diabetes Management Scale and the SED included the scales as appendices in the articles.59,67
Conclusions
Research Process
Theoretical Issues
Despite the importance of theory driven research, not all articles in this integrative review on self-efficacy identified a theoretical framework. Instruments based upon a theoretical framework and theoretical definition of the concept of interest will ultimately provide a better means to operationalize the concept.8 Not surprisingly, most studies that did recognize a guiding framework used Bandura’s SCT or the model of self-efficacy. The six constructs of the SCT provide a framework for health promotion and chronic disease management to translate health knowledge into positive health outcomes.9 These health behavior constructs include the following: knowledge, perceived self-efficacy, outcome expectations, goals, perceived facilitators, and impediments.9 Knowledge and personal motivation will help individuals face challenging situations, which is particularly important in the self-management of chronic disease.9 Moreover, the SCT highlights how individuals proactively cope and adapt to environmental stressors by relying on personal cognitive and emotional resources.69 The SCT is a natural framework to explore the concept and measurement of self-efficacy as well as one’s perceived ability to face challenging situations,70 especially in youth managing the rigors of T1DM while navigating the developmental stages of pediatric growth and development. Additionally, self-efficacy, a central component to the SCT, relates to an individual’s assessment of personal capabilities in a certain situation and the belief that carrying out behaviors will lead to a specific outcome.20,70 Utilizing the SCT or the model of self-efficacy as the underlying framework for development of self-efficacy instruments provides a theoretical overview of how youth with T1DM or their caregivers may carry out specific behaviors related to diabetes management in various scenarios.
Researchers should also consider the Social Ecological Model (SEM) when measuring self-efficacy in youth with T1DM, as one study identified through this review did.53 Similar to SCT, the SEM has been used to guide health promotion and may provide a unique perspective to assess the multifactorial relationships involved in the concept of self-efficacy for youth with T1DM.71 This widely used framework highlights the potential for dynamic interactions between the individual’s environment and layers of social support. Furthermore, this model would have direct application to evaluating various levels of caregiver self-efficacy particularly as it relates to the youth with T1DM.
Methodological Issues
The prevalence of T1DM in older children is highest in non-Hispanic white youth,72 as reflected in the homogenous participant pool of predominately white youth in the studies reviewed above. Thus, the results of this integrative review may not be generalizable to non-white youth with T1DM. Future research should include purposeful sampling of minority youth with T1DM. Additionally, the majority of participants across the reviewed studies were from higher socioeconomic status(SES) backgrounds. This further limits the generalizability of the current assessments of self-efficacy instruments, because youth and families from lower SES backgrounds may inherently face more challenges related to financial stressors, additionally impacting self-efficacy. Identifying and testing appropriate measurement instruments to evaluate self-efficacy in these vulnerable populations may be increasingly important to provide greater understanding of the relevance of this concept in all youth with T1DM.
This integrative review identified self-efficacy instruments at the individual, parent, camp counselor, and school nurse level. The SED, SEDM, DES, Dietary Self-Efficacy scale, the Maternal Self-Efficacy for Diabetes scale, and the SEDE, all measure an aspect of caregiver self-efficacy. Instrument selection depends on the specific participant sample and focus. Capturing caregiver self-efficacy is valuable as both family and caregivers outside of the family are an integral part of a youth’s success with diabetes management. Additionally, researchers and clinicians will be able to fine-tune education efforts by identifying gaps in confidence related to aspects of diabetes management for those involved in the care of the child. However, no articles evaluated peer self-efficacy or the perceived confidence of helping a friend manage diabetes in challenging situations. Because support typically shifts from the family system to friends and peers in adolescence,73 it would be useful to evaluate peer self-efficacy in diabetes management to further guide adolescents through this developmental transition. Furthermore, youth with T1DM often have multiple caregivers beyond the parents or school nurse. Use of self-efficacy instruments to assess confidence levels in T1DM management for grandparents, babysitters, and athletic coaches, among others, may expand the self-efficacy knowledge base and identify essential educational needs of these important caregivers and other key support groups in the community.
Instruments
Methods of administration, feasibility, and psychometrics
There were no major issues identified in administering the 10 instruments to youth or their caregivers, since the majority of surveys were administered during an office visit or by mail. One might not expect different psychometric properties according to response mode but future research could clarify this issue. Although none of the studies noted the exact time required to complete the respective self-efficacy assessments, time-to-completion did not appear to be a burden for survey administration. One must also consider that all instruments, except for three, were administered in English,18,32,51 an important consideration when establishing eligibility criteria. Survey translation would help broaden international access and generalizability. The main feasibility issue in fielding the various surveys is access to the instruments. The research team should consider the need to search for and possibly purchase surveys when developing a study budget.
Most instruments measuring self-efficacy demonstrated internal consistency, a form of equivalence reliability, indicating the items within the instrument conceptually fit with one another.65 However, it is important to consider that the internal consistency may vary based on the number of response options used in the Likert scale with a higher number of responses resulting in greater internal consistency74 and that the alpha value may also vary based on the number of survey items.58 Both the number of Likert options and survey length varied based on the different instruments. Apart from the SED and SEDM, extensive validity assessments for the different instruments were not frequently described. Often, the authors had to revert back to the original article describing the psychometrics of the self-efficacy instrument to obtain validity evidence. Even in these cases, the original sample may have included adults with T1DM or T2DM vs. youth with T1DM. The lack of validity data reported in the identified articles is a limitation of the contemporary literature. Validity assessments are paramount to evaluating an instrument’s capacity to measure self-efficacy or the concept of interest within a certain population.65 During instrument development and refinement, when translating available instruments into different languages, or when using instruments in different patient samples, validity tests reinforce the adequate measurement of self-efficacy. Additional research efforts should establish further psychometric analysis of these instruments in diverse populations of youth with T1DM because the sample homogeneity from the identified articles could limit the applicability of the results.
When evaluating the various self-efficacy instruments identified, it is important to acknowledge that many of the self-efficacy instruments were used in multiple articles highlighting the affinity for use. The SED and SEDM were the self-efficacy instruments most often used in the identified articles. Additionally, several studies from this integrative review revised or adapted the self-efficacy instrument to include a certain population, such as youth parent dyads for example, which clinicians and researchers should consider when selecting an instrument based on a specific population.
Another element to consider when evaluating self-efficacy instruments for future research and clinical care pertains to the ability to measure self-efficacy in the contemporary era of diabetes technologies. One article described modifying the SED instrument to include current aspects of T1DM (pump therapy),29 yet a lack of instruments to measure self-efficacy pertaining to current diabetes technology is a pertinent limitation of the available instruments. A caveat to this is that not all articles identified through the integrative review or the original articles describing the instruments included a description of survey items. While advances in diabetes technology aim to improve self-management and glycemic control, it is important to assess an individual’s confidence in the ability to use such devices. Currently available self-efficacy instruments would provide added benefit with the inclusion of assessments of self-efficacy related to technology advancements in the contemporary diabetes era. Alternatively, clinicians and researchers could design instruments to specifically evaluate youth and parent confidence related to using diabetes technologies, such as continuous glucose monitors, which are increasingly relevant with the advent of the Artificial Pancreas Project.75
Implications
Reliable and valid instruments to measure a concept of interest, such as self-efficacy, are essential for quality research and use in clinical care. The use of well-constructed measurements will confirm potential results and enhance opportunities to generalize findings to populations at large. This review is relevant to research, clinical care, and diabetes education of youth with T1DM because it identified several reliable and valid instruments to evaluate self-efficacy, an important component of diabetes self-management. The available instruments vary in length, with respect to the targeted participant age group, and whether caregivers are the focus of the assessment. Although certain studies may not have explicitly stated reliability or validity data, the psychometrics were identified in articles published prior to the 2003–2013 timeframe; however, caution is warranted if applying these psychometric properties across time and in different groups.58
This integrative review identified various gaps that could guide future research and instrument development. This search was restricted to the past decade and, thus, was not exhaustive. Of particular note is the absence of self-efficacy instruments or proxy reports that focus on peers of youth with T1DM. During the teenage years, adolescents often seek support of friends and peers, with less emphasis on support from the family unit.73 Therefore, it would be important to assess peer self-efficacy in assisting friends with T1DM in various diverse settings. Additionally, in all youth, and specifically younger children, it would be beneficial to identify valid and reliable instruments to measure self-efficacy in other caregivers, e.g., grandparents. Such research across other care providers and possibly peers could help to identify knowledge deficits and avenues for education of important groups for social support of youth with T1DM. Future studies are needed to implement self-efficacy measurements in minority populations, as well as international samples, to further assess the psychometric properties of these instruments and to broaden their application to youth with T1DM globally. Additionally, instruments to measure the construct of self-efficacy in the current era of advanced diabetes technologies, including use of insulin pumps and continuous glucose monitoring technologies, appear to be needed. A lack of instruments to measure self-efficacy related to diabetes technologies implies that the available self-efficacy instruments need to be adapted or new instruments need to be developed to be relevant in the contemporary era.
In selecting an instrument to measure self-efficacy in the pediatric population with T1DM and their caregivers, the clinical or research team must contemplate various factors. One must consider the population (i.e. youth, parents, school nurses, camp counselors), length of the scale, available psychometric data, availability of the measure, and the particular aspect related to diabetes management that the self-efficacy scale measures (i.e. diet, physical activity, general diabetes self-efficacy). Having specific criteria will guide the instrument selection. Additionally, when identifying instruments for use in the pediatric population and in the context of diabetes education, it is important to consider how the concept of self-efficacy can span throughout childhood and at what age youth are able to understand and answer questions related to self-efficacy. Many studies identified in this integrative review had youth ≥10 years old complete the various instruments, including the self-efficacy assessments; however, some studies had participants as young as 8 years old. A final consideration when evaluating instruments for use with caregivers is to determine whether the purpose of the instrument is to assess the caregiver’s own perception of confidence related to diabetes management or whether the instrument assesses the caregiver’s confidence in the child’s self-care, an important component to keep in mind when measuring the construct of self-efficacy.
In conclusion, when selecting an instrument to measure self-efficacy in youth with T1D and their caregivers, it is important to remember that one’s perceived ability for diabetes self-management reflects a constellation of behaviors. Furthermore, improvements in intensive therapy options can add to self-management challenges as diabetes technologies continue to evolve, reinforcing the need to capture self-efficacy. The evolvement of T1DM technologies will require either making modifications to existing self-efficacy instruments or developing new instruments altogether; evaluation of the psychometric properties of these instruments will be necessary. It is essential to select an instrument that is appropriate, acceptable, feasible, and responsive to both the needs of the patient and the clinician or researcher as well as an instrument that it is valid, reliable, and precise in measurement to ensure clinical and research integrity are maintained.
Acknowledgements
The authors would like to express appreciation to Mathew Gregoski, PhD, and John Dinolfo, PhD, for their guidance and encouragement. This research was supported by the NIH grant P30DK036836. The content is solely the responsibility of the authors and does not represent the official view of this organization.
Contributor Information
Lisa Rasbach, College of Nursing, Medical University of South Carolina, Charleston, SC; Joslin Diabetes Center, Boston, MA.
Carolyn Jenkins, College of Nursing, Medical University of South Carolina, Charleston, SC.
Lori Laffel, Joslin Diabetes Center, Boston, MA.
References
- 1.Hood KK, Rohan JM, Peterson CM, Drotar D. Interventions with adherence-promoting components in pediatric type 1 diabetes: meta-analysis of their impact on glycemic control. Diabetes Care. 2010 Jul;33(7):1658–1664. doi: 10.2337/dc09-2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levine BS, Anderson BJ, Butler DA, Antisdel JE, Brackett J, Laffel LM. Predictors of glycemic control and short-term adverse outcomes in youth with type 1 diabetes. J Pediatr. 2001 Aug;139(2):197–203. doi: 10.1067/mpd.2001.116283. [DOI] [PubMed] [Google Scholar]
- 3.Urbach SL, LaFranchi S, Lambert L, Lapidus JA, Daneman D, Becker TM. Predictors of glucose control in children and adolescents with type 1 diabetes mellitus. Pediatr Diabetes. 2005 Jun;6(2):69–74. doi: 10.1111/j.1399-543X.2005.00104.x. [DOI] [PubMed] [Google Scholar]
- 4.CDC. National diabetes fact sheet: National estimates and general information on diabetes and prediabetes in the United States. 2011 http://www.searchfordiabetes.org/documents/CDCFact2011.pdf. [Google Scholar]
- 5.Herge WM, Streisand R, Chen R, Holmes C, Kumar A, Mackey ER. Family and youth factors associated with health beliefs and health outcomes in youth with type 1 diabetes. J Pediatr Psychol. 2012 Oct;37(9):980–989. doi: 10.1093/jpepsy/jss067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iannotti RJ, Schneider S, Nansel TR, et al. Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. J Dev Behav Pediatr. 2006 Apr;27(2):98–105. doi: 10.1097/00004703-200604000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Merkel RM, Wright T. Parental self-efficacy and online support among parents of children diagnosed with type 1 diabetes mellitus. Pediatr Nurs. 2012 Nov-Dec;38(6):303–308. [PubMed] [Google Scholar]
- 8.Waltz CF, Strickland OL, Lenz ER. Measurement in nursing and health research. 4th ed. New York: Springer; 2010. [Google Scholar]
- 9.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004 Apr;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 10.Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005 Dec;52(5):546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 11.AADE. AADE7 self-care behaviors: Measureable behavior change is the desired outcome of diabetes education. 2013 http://www.diabeteseducator.org/ProfessionalResources/AADE7/. [Google Scholar]
- 12.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CEBM. Oxford centre for evidence-based medicine: Levels of evidence. 2009 http://www.cebm.net/index.aspx?o=1025. [Google Scholar]
- 14.Redding CA, Maddock JE, Rossi JS. The sequential approach to measurement of health behavior constructs: Issues in selecting and developing measures. Californian J Health Promot. 2006;4(1):83–101. [Google Scholar]
- 15.Nouwen A, Urquhart Law G, Hussain S, McGovern S, Napier H. Comparison of the role of self-efficacy and illness representations in relation to dietary self-care and diabetes distress in adolescents with type 1 diabetes. Psychol Health. 2009 Nov;24(9):1071–1084. doi: 10.1080/08870440802254597. [DOI] [PubMed] [Google Scholar]
- 16.Grey M, Whittemore R, Jaser S, et al. Effects of coping skills training in school-age children with type 1 diabetes. Res Nurs Health. 2009 Aug;32(4):405–418. doi: 10.1002/nur.20336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stupiansky NW, Hanna KM, Slaven JE, Weaver MT, Fortenberry JD. Impulse control, diabetes-specific self-efficacy, and diabetes management among emerging adults with type 1 diabetes. J Pediatr Psychol. 2013 Apr;38(3):247–254. doi: 10.1093/jpepsy/jss110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart SM, Lee PW, Waller D, et al. A follow-up study of adherence and glycemic control among Hong Kong youths with diabetes. J Pediatr Psychol. 2003 Jan-Feb;28(1):67–79. doi: 10.1093/jpepsy/28.1.67. [DOI] [PubMed] [Google Scholar]
- 19.Marvicsin D. School-age children with diabetes: role of maternal self-efficacy, environment, and management behaviors. Diabetes Educ. 2008 May-Jun;34(3):477–483. doi: 10.1177/0145721708316944. [DOI] [PubMed] [Google Scholar]
- 20.Fisher KL. School nurses' perceptions of self-efficacy in providing diabetes care. J Sch Nurs. 2006 Aug;22(4):223–228. doi: 10.1177/10598405050220040701. [DOI] [PubMed] [Google Scholar]
- 21.Berg CA, King PS, Butler JM, Pham P, Palmer D, Wiebe DJ. Parental involvement and adolescents' diabetes management: the mediating role of self-efficacy and externalizing and internalizing behaviors. J Pediatr Psychol. 2011 Apr;36(3):329–339. doi: 10.1093/jpepsy/jsq088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Butler JM, Berg CA, King P, et al. Parental negative affect and adolescent efficacy for diabetes management. J Fam Psychol. 2009 Aug;23(4):611–614. doi: 10.1037/a0016141. [DOI] [PubMed] [Google Scholar]
- 23.Palmer DL, Berg CA, Butler J, et al. Mothers', fathers', and children's perceptions of parental diabetes responsibility in adolescence: examining the roles of age, pubertal status, and efficacy. J Pediatr Psychol. 2009 Mar;34(2):195–204. doi: 10.1093/jpepsy/jsn073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Battaglia MR, Alemzadeh R, Katte H, Hall PL, Perlmuter LC. Brief report: disordered eating and psychosocial factors in adolescent females with type 1 diabetes mellitus. J Pediatr Psychol. 2006 Jul;31(6):552–556. doi: 10.1093/jpepsy/jsj047. [DOI] [PubMed] [Google Scholar]
- 25.Winsett RP, Stender SR, Gower G, Burghen GA. Adolescent self-efficacy and resilience in participants attending A diabetes camp. Pediatr Nurs. 2010 Nov-Dec;36(6):293–296. quiz 297. [PubMed] [Google Scholar]
- 26.Gillibrand R, Stevenson J. The extended health belief model applied to the experience of diabetes in young people. Br JHealth Psychol. 2006 Feb;11(Pt 1):155–169. doi: 10.1348/135910705X39485. [DOI] [PubMed] [Google Scholar]
- 27.Wysocki T, Nansel TR, Holmbeck GN, et al. Collaborative involvement of primary and secondary caregivers: associations with youths' diabetes outcomes. J Pediatr Psychol. 2009 Sep;34(8):869–881. doi: 10.1093/jpepsy/jsn136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ambrosino JM, Fennie K, Whittemore R, Jaser S, Dowd MF, Grey M. Short-term effects of coping skills training in school-age children with type 1 diabetes. Pediatr diabetes. 2008 Jun;9(3 Pt 2):74–82. doi: 10.1111/j.1399-5448.2007.00356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whittemore R, Jaser SS, Jeon S, et al. An internet coping skills training program for youth with type 1 diabetes: six-month outcomes. Nurs Res. 2012 Nov-Dec;61(6):395–404. doi: 10.1097/NNR.0b013e3182690a29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Faulkner MS, Michaliszyn SF, Hepworth JT. A personalized approach to exercise promotion in adolescents with type 1 diabetes. Pediatr diabetes. 2010 May;11(3):166–174. doi: 10.1111/j.1399-5448.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hackworth NJ, Hamilton VE, Moore SM, Northam EA, Bucalo Z, Cameron FJ. Predictors of diabetes self-care, metabolic control, and mental health in youth with type 1 diabetes. AustPsychologist. 2013;48:360–368. [Google Scholar]
- 32.Chih AH, Jan CF, Shu SG, Lue BH. Self-efficacy affects blood sugar control among adolescents with type I diabetes mellitus. J Formos Med Assoc. 2010 Jul;109(7):503–510. doi: 10.1016/S0929-6646(10)60084-8. [DOI] [PubMed] [Google Scholar]
- 33.Butler JM, Skinner M, Gelfand D, Berg CA, Wiebe DJ. Maternal parenting style and adjustment in adolescents with type I diabetes. J Pediatr Psychol. 2007 Nov-Dec;32(10):1227–1237. doi: 10.1093/jpepsy/jsm065. [DOI] [PubMed] [Google Scholar]
- 34.Chiu HJ. A test of the Bruhn and Parcel Model of Health Promotion. J Nurs Res. 2005 Sep;13(3):184–196. doi: 10.1097/01.jnr.0000387540.83630.38. [DOI] [PubMed] [Google Scholar]
- 35.Edmunds S, Roche D, Stratton G, Wallymahmed K, Glenn SM. Physical activity and psychological well-being in children with Type 1 diabetes. Psychol Health Med. 2007 May;12(3):353–363. doi: 10.1080/13548500600975446. [DOI] [PubMed] [Google Scholar]
- 36.Holmes CS, Chen R, Streisand R, et al. Predictors of youth diabetes care behaviors and metabolic control: a structural equation modeling approach. J Pediatr Psychol. 2006 Sep;31(8):770–784. doi: 10.1093/jpepsy/jsj083. [DOI] [PubMed] [Google Scholar]
- 37.Kaugars AS, Kichler JC, Alemzadeh R. Assessing readiness to change the balance of responsibility for managing type 1 diabetes mellitus: adolescent, mother, and father perspectives. Pediatr Diabetes. 2011 Sep;12(6):547–555. doi: 10.1111/j.1399-5448.2010.00737.x. [DOI] [PubMed] [Google Scholar]
- 38.McMahon SK, Airey FL, Marangou DA, et al. Insulin pump therapy in children and adolescents: improvements in key parameters of diabetes management including quality of life. Diabet Med. 2004;22:92–96. doi: 10.1111/j.1464-5491.2004.01359.x. [DOI] [PubMed] [Google Scholar]
- 39.Rossello JM, Jimenez-Chafey MI. Cognitive-behavioral group therapy for depression in adolescents with diabetes: a pilot study. Interramerican Journal of Psychology. 2006;40(2):219–226. [Google Scholar]
- 40.Schilling LS, Dixon JK, Knafl KA, et al. A new self-report measure of self-management of type 1 diabetes for adolescents. Nurs Res. 2009 Jul-Aug;58(4):228–236. doi: 10.1097/NNR.0b013e3181ac142a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sullivan-Bolyai S, Crawford S, Johnson K, Huston B, Lee MM. Educating diabetes camp counselors with a human patient simulator: a pilot study. Journal for specialists in pediatric nursing : JSPN. 2012 Apr;17(2):121–128. doi: 10.1111/j.1744-6155.2011.00322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kichler JC, Kaugars AS, Ellis J, Alemzadeh R. Exploring self-management characteristics in youths with type 1 diabetes mellitus: does membership in a glycemic control category matter? Pediatr Diabetes. 2010 Dec;11(8):536–543. doi: 10.1111/j.1399-5448.2010.00638.x. [DOI] [PubMed] [Google Scholar]
- 43.Austin S, Senecal C, Guay F, Nouwen A. Effects of gender, age, and diabetes duration on dietary self-care in adolescents with type 1 diabetes: a Self-Determination Theory perspective. J Health psychol. 2011 Sep;16(6):917–928. doi: 10.1177/1359105310396392. [DOI] [PubMed] [Google Scholar]
- 44.Law GU, Walsh J, Queralt V, Nouwen A. Adolescent and parent diabetes distress in type 1 diabetes: the role of self-efficacy, perceived consequences, family responsibility and adolescent-parent discrepancies. J Psychosom Res. 2013 Apr;74(4):334–339. doi: 10.1016/j.jpsychores.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 45.Hanna KM, Weaver MT, Stump TE, et al. Initial findings: primary diabetes care responsibility among emerging adults with type 1 diabetes post high school and move out of parental home. Child Care Health Dev. 2011 Jan;39(1):61–68. doi: 10.1111/j.1365-2214.2011.01320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hanna KM, Weaver MT, Stump TE, Slaven JE, Fortenberry JD, DiMeglio LA. Readiness for living independently among emerging adults with type 1 diabetes. Diabetes Educ. 2013 Jan-Feb;39(1):92–99. doi: 10.1177/0145721712465341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Berg CA, Butner JE, Butler JM, King PS, Hughes AE, Wiebe DJ. Parental persuasive strategies in the face of daily problems in adolescent type 1 diabetes management. Health Psychol. 2013 Jul;32(7):719–728. doi: 10.1037/a0029427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Berg CA, Skinner M, Ko K, et al. The fit between stress appraisal and dyadic coping in understanding perceived coping effectiveness for adolescents with type 1 diabetes. J Fam Psychol. 2009 Aug;23(4):521–530. doi: 10.1037/a0015556. [DOI] [PubMed] [Google Scholar]
- 49.Hughes AE, Berg CA, Wiebe DJ. Emotional processing and self-control in adolescents with type 1 diabetes. J Pediatr Psychol. 2012 Sep;37(8):925–934. doi: 10.1093/jpepsy/jss062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Croom A, Wiebe DJ, Berg CA, et al. Adolescent and parent perceptions of patient-centered communication while managing type 1 diabetes. J Pediatr Psychol. 2011 Mar;36(2):206–215. doi: 10.1093/jpepsy/jsq072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kristensen LJ, Thastum M, Mose AH, Birkebaek NH. Psychometric evaluation of the adherence in diabetes questionnaire. Diabetes Care. 2012 Nov;35(11):2161–2166. doi: 10.2337/dc11-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sander EP, Odell S, Hood KK. Diabetes-specific family conflict and blood glucose monitoring in adolescents with type 1 diabetes: Mediational role of diabetes self-efficacy. Diabetes Spectrum. 2010;23(2):89–94. [Google Scholar]
- 53.Armstrong B, Mackey ER, Streisand R. Parenting behavior, child functioning, and health behaviors in preadolescents with type 1 diabetes. J Pediatr Psychol. 2011 Oct;36(9):1052–1061. doi: 10.1093/jpepsy/jsr039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.APA. A reference for professionals: Developing adolescents. 2002 http://www.apa.org/pi/families/resources/develop.pdf. [Google Scholar]
- 55.Streisand R, Mackey ER, Elliot BM, et al. Parental anxiety and depression associated with caring for a child newly diagnosed with type 1 diabetes: opportunities for education and counseling. Patient Educ Couns. 2008 Nov;73(2):333–338. doi: 10.1016/j.pec.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 56.Streisand R, Swift E, Wickmark T, Chen R, Holmes CS. Pediatric parenting stress among parents of children with type 1 diabetes: the role of self-efficacy, responsibility, and fear. J Pediatr Psychol. 2005 Sep;30(6):513–521. doi: 10.1093/jpepsy/jsi076. [DOI] [PubMed] [Google Scholar]
- 57.DeVellis RF. Scale development theory and applications. 3rd ed. Los Angeles, CA: Sage; 2012. [Google Scholar]
- 58.Streiner DL. Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess. 2003 Feb;80(1):99–103. doi: 10.1207/S15327752JPA8001_18. [DOI] [PubMed] [Google Scholar]
- 59.Grossman HY, Brink S, Hauser ST. Self-efficacy in adolescent girls and boys with insulin-dependent diabetes mellitus. Diabetes Care. 1987 May-Jun;10(3):324–329. doi: 10.2337/diacare.10.3.324. [DOI] [PubMed] [Google Scholar]
- 60.Anderson RM, Funnell MM, Fitzgerald JT, Marrero DG. The Diabetes Empowerment Scale: a measure of psychosocial self-efficacy. Diabetes Care. 2000 Jun;23(6):739–743. doi: 10.2337/diacare.23.6.739. [DOI] [PubMed] [Google Scholar]
- 61.Littlefield CH, Craven JL, Rodin GM, Daneman D, Murray MA, Rydall AC. Relationship of self-efficacy and binging to adherence to diabetes regimen among adolescents. Diabetes Care. 1992 Jan;15(1):90–94. doi: 10.2337/diacare.15.1.90. [DOI] [PubMed] [Google Scholar]
- 62.Senecal C, Nouwen A, White D. Motivation and dietary self-care in adults with diabetes: are self-efficacy and autonomous self-regulation complementary or competing constructs? Health Psychol. 2000 Sep;19(5):452–457. doi: 10.1037//0278-6133.19.5.452. [DOI] [PubMed] [Google Scholar]
- 63.Wallston KA, Rothman RL, Cherrington A. Psychometric properties of the Perceived Diabetes Self-Management Scale (PDSMS) J Behav Med. 2007 Oct;30(5):395–401. doi: 10.1007/s10865-007-9110-y. [DOI] [PubMed] [Google Scholar]
- 64.Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ. 2009 Jul-Aug;35(4):641–651. doi: 10.1177/0145721709335006. [DOI] [PubMed] [Google Scholar]
- 65.DeVon HA, Block ME, Moyle-Wright P, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39(2):155–164. doi: 10.1111/j.1547-5069.2007.00161.x. [DOI] [PubMed] [Google Scholar]
- 66.Pender NJ, Bar-Or O, Wilk B, Mitchell S. Self-efficacy and perceived exertion of girls during exercise. Nurs Res. 2002 Mar-Apr;51(2):86–91. doi: 10.1097/00006199-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 67.Leonard BJ, Skay CL, Rheinberger MM. Self-management development in children and adolescents with diabetes: the role of maternal self-efficacy and conflict. J Pediatr Nurs. 1998 Aug;13(4):224–233. doi: 10.1016/S0882-5963(98)80049-3. [DOI] [PubMed] [Google Scholar]
- 68.University of Michigan. Michigan Diabetes Research and Training Center: Survey instruments. 2013 http://www.med.umich.edu/mdrtc/profs/survey.html - des. [Google Scholar]
- 69.Benight CC, Bandura A. Social cognitive theory of posttraumatic recovery: the role of perceived self-efficacy. Behav Res Ther. 2004 Oct;42(10):1129–1148. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 70.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977 Mar;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 71.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996 Mar-Apr;10(4):282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 72.CDC. Children and diabetes: SEARCH for diabetes in youth. 2013 http://www.cdc.gov/diabetes/projects/diab_children.htm.
- 73.Wysocki T, Greco P. Social support and diabetes management in childhood and adolescence: influence of parents and friends. Curr Diab Rep. 2006 Apr;6(2):117–122. doi: 10.1007/s11892-006-0022-y. [DOI] [PubMed] [Google Scholar]
- 74.DiIorio CK. Measurement in health behavior. San Francisco, CA: Jossey-Bass. A Wiley Imprint; 2005. [Google Scholar]
- 75.Kowalski AJ. Can we really close the loop and how soon? Accelerating the availability of an artificial pancreas: a roadmap to better diabetes outcomes. Diabetes Technol Ther. 2009 Jun;11(Suppl 1):S113–S119. doi: 10.1089/dia.2009.0031. [DOI] [PubMed] [Google Scholar]