Abstract
Little is known about the inflammatory effects of resistance exercise in healthy and even less in diseased individuals such as cardiac patients. The purpose of this study was to examine the acute pro- and anti-inflammatory responses during resistance exercise (RE) in patients with coronary artery disease. Eight low risk patients completed two acute RE protocols at low (50% of 1 RM; 2x18 rps) and moderate intensity (75% of 1 RM; 3x8 rps) in random order. Both protocols included six exercises and had the same total load volume. Blood samples were obtained before, immediately after and 60 minutes after each protocol for the determination of lactate, TNFα, INF-γ, IL-6, IL-10, TGF-β1, and hsCRP concentrations. IL-6 and IL-10 levels increased (p < 0.05) immediately after both RE protocols with no differences between protocols. INF-γ was significantly lower (p < 0.05) 60 min after the low intensity protocol, whereas TGF-β1 increased (p < 0.05) immediately after the low intensity protocol. There were no differences in TNF-& and hs-CRP after both RE protocols or between protocols. The above data indicate that acute resistance exercise performed at low to moderate intensity in low risk, trained CAD patients is safe and does not exacerbate the inflammation associated with their disease.
Key points.
Acute resistance exercise is safe without exacerbating inflammation in patients with CAD.
Both exercise intensities (50 and 75% of 1 RM) elicit desirable pro-and anti-inflammatory responses.
With both exercise intensities (50 and 75% of 1 RM) acceptable clinical hemodynamic alterations were observed.
Key words: Resistance exercise, inflammation, cardiac rehabilitation
Introduction
During the last two decades resistance exercise (RE) has gained popularity in patients with coronary artery disease (CAD) and several studies have indicated that this type of training is safe since it causes favorable physiological adaptations (Ghilarducci et al., 1989; Kelemen et al., 1986; McCartney et al., 1991; Sparling et al., 1990; Williams et al. 2007). Furthermore, resistance exercise significantly improves mood state, self-confidence and quality of life in these patients (Beniamini et al. 1997; Ewart, 1989). Therefore, the American Heart Association recommends resistance training as part of an exercise program for CAD patients at least twice a week (Williams et al., 2007).
Recently, low-grade inflammation has been recognized as an integral part of the development and progression of atherosclerosis (Hansson, 2005). On the other hand, research suggests that the levels of local and systemic inflammation can be reduced by different lifestyles and pharmacological interventions including drugs, weight loss, smoking cessation or exercise (Esposito et al., 2003; Petersen et al., 1995).
It is known that acute and chronic exercise elicits different inflammatory alterations that depend on the characteristics of the exercise, training level, age and health status of the individual. Acute exercise usually elicits a serious inflammatory response whereas chronic exercise can attenuate the response of a single bout of exercise. Thus, exercise is recommended as an anti-inflammatory therapy for patients with a chronic inflammatory disease (Brandt and Pedersen, 2010; Mathur and Pedersen, 2008).
Information relating to the inflammatory and anti-inflammatory nature of exercise is derived mainly from research that used aerobic training as the mode of exercise. Little research has examined the inflammatory effects of RE in healthy individuals in general and more specifically in diseased individuals with the results of the existing studies being equivocal (Izquierdo et al., 2009; Medham et al., 2011; Peake et al., 2006; Phillips et al., 2010; Smith et al., 2000; Uchida et al., 2009). An increase in IL-6 concentration after resistance training is a consistent finding with the magnitude of this alteration lower when compared with aerobic exercise (Pedersen et al., 2007).
To our knowledge there are no data on the pro- and anti-inflammatory effects of RE in patients with CAD. In addition, the extent to which acute RE alters the inflammatory response CAD patients is unclear. Clarity on this is important to ensure that this type of exercise is performed in a safe manner without amplification to inflammation. In addition, the intensity of RE is an important regulator of physiological stress and no data exist on the association between the intensity of RE and pro- and anti-inflammatory responses in CAD patients. Therefore, the purpose of our study was to examine the effects of acute RE on inflammatory markers in stable, low risk CAD patients. We hypothesized that acute RE of two different intensities [50 & 75 % of one repetition maximum (1 RM)] would elicit normal pro- and anti-inflammatory responses within physiological limits.
Methods
Participants
Eight males (age: 46.9 ± 10.3 y, height: 1.75 ± 0.09 m, body mass: 86.4 ± 11.9 kg, BMI: 28.2 ± 3.1 kg·m2) with coronary artery disease volunteered to participate in this study. They had previously experienced a myocardial infraction or had undergone coronary artery bypass grafting or percutaneous transluminal coronary angioplasty (Table 1).
Table 1.
Patient’s characteristics at the onset of the study. Values presented as and integral numbers.
| Condition/Procedure | |
|---|---|
| MI | 3 |
| CABG | 2 |
| PTCA | 3 |
| Rehabilitation phase | IV |
| Medications | |
| Nitrates | 2 |
| β-blockers | 6 |
| ACE inhibitors | 4 |
| Calcium channel blockers | 2 |
| Diuretics | 1 |
| Statins | 4 |
CABG: coronary artery bypass grafting; MI: myocardial infarction; PTCA: percutaneus transluminal coronary angioplasty; ACE: angiotensin-converting enzyme.
Exclusion criteria were uncontrolled congestive heart failure, unstable angina, uncontrolled diabetes mellitus, unstable dysrhythmia and uncontrolled systemic hypertension. Furthermore, patients with arthritis or other myoskeletal and inflammatory diseases as well as patients under anti-inflammatory drugs were also excluded. For safety reasons, low-risk patients were recruited according to the following criteria: i) functional capacity: >7 METs, ii) ejection fraction: > 50%, iii) absence of arrhythmias and iv) absence of ischemia (AACPR 1995). All participants followed a combined strength (2 sets, 12-15 rps, 8 exercises at 50-60% of 1 RM, 2x/week) and aerobic training program (60-75% of HRmax, 30-45 min, 2x/week) for 3 to 6 months before entering the study. A written informed consent was obtained from the subjects before the initiation of the study. The experimental protocol was approved by the institutional ethics committee and was completed in accordance with the declaration of Helsinki.
Experimental design
The participants reported to the laboratory at 8 – 9 a.m. after an overnight fast. They were instructed to avoid caffeine and alcohol consumption for 24h and not to perform any physical activity for 48h before the experimental sessions. Pro-inflammatory and anti-inflammatory cytokine responses were compared after the performance of two resistance exercise protocols: a low and a moderate intensity protocol. For the low intensity protocol (50% of 1-RM) the participants executed 2 sets of 18 repetitions for each exercise with 90 seconds rest between sets. For the moderate intensity protocol (75% of 1-RM) the participants executed 3 sets of 8 repetitions for exercise with 90 seconds rest between sets. Volume load (sets x repetitions x load) was identical in both the low and the moderate intensity protocols (6945 ± 647.5 vs 7040 ± 575.1 kg, respectively, p > 0.05). Both protocols included six exercises performed in the following order: seated chest press, shoulder press, leg press, lateral pull-downs, leg extension, and leg flexion. The two protocols were performed in random order and in a counterbalanced way with at least a 4 day interval.
Before the application of the protocols a warm-up routine of 10 min walking and muscular stretching was performed. Heart rate was continuously monitored during the exercise with a telemetric devise (Polar RS400; Polar Electro, Finland). Blood pressure was measured immediately after each exercise with a manual sphygmomanometer. Blood samples were obtained before the exercise session (BE), immediately after (IAE) and 60 minutes after (60AE) the end of the protocols, by veni-puncture for the determination of TNFα, IFN-γ, IL-6, IL-10, TGF-β1, and hsCRP concentrations. Blood lactate was measured before, immediately after and 30 min after the end of the protocols.
Blood analyses
Blood samples (10 ml) were drawn at each sampling time point and 10 μl was drawn into capillaries to be analyzed for blood lactate concentrations using an enzymatic method (Miniphotometer 8, Dr. Lange, Berlin, Germany). The blood was then centrifuged at 2500 rpm for 15 min at 44C. Serum (hs-CRP determination) and plasma was removed, separated into aliquots, and frozen at –808 C until analyzed. The analyses were performed using enzyme linked immunoabsorbent assay (ELISA) for TNF-α, IFN-γ (assay sensitivity 4 pg·mL-1; intra assay coefficients of variation 4.8% and 6.2%, respectively; eBioscience Inc.); IL-6, IL-10 (assay sensitivity 2 pg·mL-1; intra assay coefficients of variation 8.5% and 7.4%, respectively; eBioscience Inc.); TGF-β1 (assay sensitivity 1.9 pg·mL-1; intra assay coefficients of variation 2.5%; DRG International, Inc.); and hs-CRP (assay sensitivity 0.1 mg·L-1; intra assay coefficients of variation 5.1%; DRG International, Inc.). Samples from the same participant were analyzed in the same assay.
Statistical analyses
Normal distribution of the data was determined with the Shapiro-Wilks statistic. For normally distributed variables (TNFα, IL-10, TGF-β1) a two-way analysis of variance (protocol x time) with repeated measures was used to examine the effects of protocol, time point and the interaction effects. For variables that were not normally distributed (IFN-γ, IL-6, hsCRP) a log10 transformation was performed and thereafter the ANOVA procedure followed. The effect sizes were calculated using Cohen’s d (d = difference between means r pooled SD) for pair wise comparisons and statistical power (P) of the analysis was determined as suggested by Keppel (1991). The small, medium, and large effects would be reflected for Cohen’s d in values greater than 0.2, 0.5, and 0.8, respectively (Cohen 1988). Significant differences between means were located with the Tukey HSD procedure. The significance level was set at p<0.05.
Results
The execution of both the 75% protocol and the 50% protocol caused significant increases in systolic blood pressure (75% protocol: p = 0.01, max d = 2.93, P = 1; 50% protocol: p = 0.01, max d= 2.93, P = 1), diastolic blood pressure (75% protocol: p = 0.01, max d = 1.04, P = 1; 50% protocol: p = 0.01, max d = 1.43, P = 1), and heart rate (75% protocol: p = 0.01, max d = 2.28, P = 1; 50% protocol: p = 0.01, max d = 2.74, P = 1). No differences were observed between the protocols in systolic (p= 0.99, max d= 0.10, P = 0.07) and diastolic blood pressure (p = 0.52, max d = 0.64, P = 0.3), and heart rate (p = 0.26, max d = 0.56, P = 0.46) (Table 2) at any time point.
Table 2.
Hemodynamic responses during the execution of equal volume load resistance exercise protocols at an intensity of 50 and 75% of 1RM. Data are means (±SD).
| Rest | Chest press | Shoulder press | Leg press | Pull down | Leg extension | Leg curl | |
|---|---|---|---|---|---|---|---|
| Heart rate (b·min-1) | |||||||
| 50 % | 80.3 (10.4) | 95.3 (10.6)* | 101.9 (13.3)* | 106.7 (15.3)* | 105 (17.8)* | 115.1 (25.9)*†# | 126.6 (20.0)*†# |
| 75% | 80.9 (9.7) | 99.6 (23.1)* | 103.6 (20.8)* | 105 (14.8)* | 104.6 (12.9)* | 112.1 (16.5)* | 115.3 (17.6)* |
| Systolic BP (mmHg) | |||||||
| 50% | 116.4 (6.3) | 130.7 (12.7)* | 137.1 (7.6)* | 140.0 (7.6)* | 144.3 (11.0)*† | 144.3 (9.3)*† | 151.4 (14.6)*†# |
| 75% | 117.1 (7.6) | 132.9 (16.0)* | 138.6 (9.0)* | 142.9 (10.4)* | 145.7 (11.0)* | 146.4 (9.0)* | 150.0 (12.9)*† |
| Diastolic BP (mmHg) | |||||||
| 50% | 76.4 (6.9) | 78.6 (3.8) | 80.0 (7.6) | 82.9 (7.0) | 86.4 (4.8)* | 86.4 (4.3)* | 86.4 (4.3)* |
| 75% | 74.3 (4.5) | 79.3 (7.3) | 80.7 (6.7) | 77.1 (7.6) | 80.7 (10.6) | 81.4 (8.0) | 85.0 (12.9) |
| Double product (*103) | |||||||
| 50% | 9.4 (1.4) | 12.5 (1.8)* | 14.0 (2.1)* | 15.0 (2.8)* | 15.3 (3.6)* | 16.7 (4.2)* | 19.2 (3.8)*†# |
| 75% | 9.5 (1.5) | 13.3 (4.8)* | 14.4 (3.3)* | 15.1 (3.0)* | 15.2 (2.1)* | 16.5 (3.3)* | 17.3 (3.4)*† |
* p < 0.05 from rest
† p < 0.05 from chest press
# p < 0.05 from shoulder press
Blood lactate values were higher immediately after and 30 minutes after the execution of both the 75% (p = 0.01; IAE-BE: d = 6.15, 60AE-BE: d = 2.56, 60AE-IAE: d = -3.29; P = 1) and 50% (p = 0.01; IAE-BE: d = 15.88, 60AE-BE: d = 3.01, 60AE-IAE: d = -3.11; P = 1) protocols compared to pre exercise values (Figure 1). Blood lactate was higher immediately after and 30 minutes after the 50% protocol compared with the 75% protocol (p = 0.01; BE: d = -0.16, IAE: d = 2.5, 60AE: d = 1.22; P = 0.98).
Figure 1.
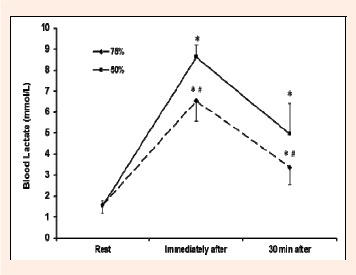
Blood lactate concentration following resistance exercise at an intensity of 50 and 75% of 1RM. * p< 0.05 from rest, # p< 0.05 from the 75% protocol
TNF-α concentration did not change over time in both the 75% (p = 0.87; IAE-BE: d = 0.11, 60AE-BE: d = -0.24, 60AE-IAE: d = 0.12; P = 0.07) and the 50% (p = 0.34; IAE-BE: d = -0.21, 60AE-BE: d = -0.06, 60AE-IAE: d = 0.13; P = 0.21) protocols (Figure 2).
Figure 2.
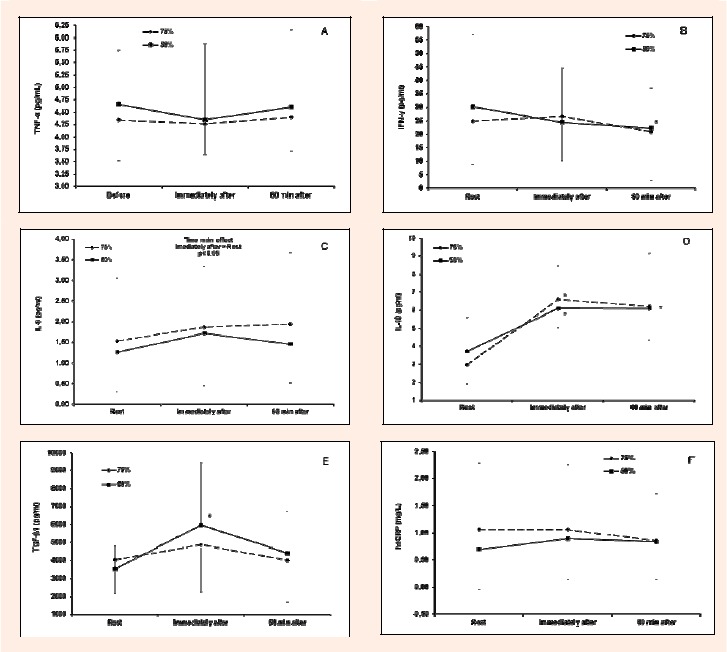
TNF-α (A), IFN-γ (B), IL-6 (C), IL-10 (D), TGF-β1 (E) and hsCRP (F) concentrations following resistance exercise at an intensity of 50 and 75% of 1RM. * p < 0.05 from rest, # p < 0.05 from the 75% protocol
IFN-γ concentration was lower 60 min after the end of resistance exercise compared with before and immediately after the exercise in the 75% protocol (p= 0.057; IAE-BE: d= 0.03, 60AE-BE: d= -0.28, 60AE-IAE: d= -0.31; P= 0.56) and did not change following the 50% protocol (p= 0.26; IAE-BE: d= -0.20, 60AE-BE: d= -0.28, 60AE-IAE: d= -0.09; P= 0.26). No differences (p= 0.2; BE: d= 0.22, IAE: d= 0.02, 60AE: d= 0.21; P= 0.31) were found in IFN-γ concentrations between the two protocols at any time point (Figure 2).
IL-6 concentrations did not change after the 75% (p= 0.17; IAE-BE: d= 0.18, 60AE-BE: d= 0.12, 60AE-IAE: d= -0.05; P= 0.35) and the 50% protocol (p= 0.09; IAE-BE: d= 0.31, 60AE-BE: d= 0.17, 60AE-IAE: d= -0.17; P= 0.48). However, a time main effect was observed the with IL-6 concentration being higher immediately after RE compared with pre exercise (p=0.04, P= 0.63). No significant differences (p= 0.88; BE: d= 0.31, IAE: d= 0.21, 60AE: d= 0.31; P= 0.07) were found in IL-6 concentrations between the two protocols at any time point (Figure 2).
IL-10 concentration was higher immediately after and 60 min after both the 75% (p = 0.001; IAE-BE: d = 0.95, 60AE-BE: d = 0.98, 60AE-IAE: d = 0.19; P = 0.98) and 50% (p = 0.001; IAE-BE: d= 1.02, 60AE-BE: d= 1.02, 60AE-IAE: d = 0.05; P=1) protocols. No differences (p = 0.34; BE: d = 0.0, IAE: d = -0.24, 60AE: d = -0.33; P = 0.21) were observed between the two protocols for IL-10 responses (Figure 2).
TGF-β1 concentration did not change after the 75% protocol (p = 0.22, IAE-BE: d = 0.22, 60AE-BE: d = -0.12, 60AE-IAE: d = -0.30; P = 0.29) but increased immediately after compared with pre exercise values during the 50% protocol (p = 0.03; IAE-BE: d = 0.74, 60AE-BE: d = 0.22, 60AE-IAE: d = 0.54; P = 0.69). No differences (p=0.24; BE: d= -0.34, IAE: d= 0.34, 60AE: d= 0.14; P=0.28) were observed between the two protocols at any time point (Figure 2).
hsCRP concentration did not change following the 75% protocol (p = 0.28; IAE-BE: d = 0.01, 60AE-BE: d = 0.19, 60AE-IAE: d = -0.19; P = 0.25) or the 50% protocol (p = 0.09; IAE-BE: d = 0.19, 60AE-BE: d = 0.08, 60AE-IAE: d = -0.12; P = 0.47). No differences (p = 0.15; BE: d = -0.32, IAE: d = -0.17, 60AE: d = -0.08; P = 0.36) were observed between the two protocols at any time point (Figure 2).
Discussion
The results of the present study demonstrate that acute resistance exercise performed at low to moderate intensity (50-75% of 1 RM) in previously trained CAD patients is safe without exacerbating underlying inflammation. Both exercise intensities elicited normal pro-and anti-inflammatory responses as shown by the concentrations of TNF-α, hs-CRP, INF-γ, IL-6, IL-10 and TGF-β1.
Although RE has been accepted as a safe and effective training modality for CAD patients, little is known about its potential effects on inflammatory markers. In our study, IL-6 significantly increased immediately after the end of both RE protocols, irrespective of exercise intensity (Figure 2). It is well-known that IL-6 is the first cytokine released exponentially into circulation during exercise (up to 100-fold) which is also consistent with the results of other RE studies in healthy, untrained individuals (Phillips et al., 2010; Smith et al., 2000). Recently, Philips et al., 2010), used a similar design in untrained men and observed that a low intensity resistance training program (65% of 1 RM) resulted in a greater circulating IL-6 concentration immediately after exercise compared with a high intensity program (85% of 1 RM).
In the current literature there is an ongoing debate regarding the anti-or pro-inflammatory effects of IL-6. Specifically, IL-6 secreted by myocytes appears to be anti-inflammatory, as opposed to IL-6 secreted chronically by adipose tissue (Pedersen and Febbraio 2008). When IL-6 is secreted by muscular contraction during exercise, it increases anti-inflammatory cytokines such as IL-10 and IL-1ra and inhibits IL-1β and TNF-& release (Brandt and Pedersen, 2010). Indeed, in our study, which was conducted at low and moderate intensity during resistance exercise, the concentrations of TNF-α and hs-CRP remained unchanged, whereas IFN-γ levels were reduced 60 min after exercise (significant only with the 75% of 1 RM protocol). Taken as a whole, our findings suggest that acute low-moderate intensity resistance exercise does not exacerbate underlying inflammation, in patients with CAD, and to our knowledge, this is the first study presented on this topic.
The circulating levels of the anti-inflammatory cytokines such as IL-10 and IL-1ra have been shown to increase after a session of aerobic exercise (Petersen and Pedersen, 1995). However, the few studies that have examined the anti-inflammatory effects of RE on healthy adults reported equivocal results (Peake et al., 2006; Smith et al., 2000; Uchida et al., 2009). In our study, we observed a significant increase in IL-10 concentration immediately and 60 min after both RE protocols. Differences in the mode, intensity or duration of the applied training protocols as well as the health or fitness status of the individuals are factors which could explain the inconsistency between studies. It has been reported that when IL-10 is added to a culture of mononuclear and neutrophil cells, the synthesis of the pro-inflammatory cytokines is inhibited (Bolger et al., 2002); thus IL-10 is an important suppressor of the inflammatory response after exercise.
In addition to IL-10, TGF-β1 has recently been established as an anti-inflammatory growth factor with a significant impact on plaque stability (Lutgens et al., 2002). TGF-β1 expression increases in response to mechanical stimuli in the vascular bed (O`Callaghan and Williams, 2000). Therefore, the increased shear stress expected during RE may act as the mechanical strain required for TGF-β1 mRNA over expression. Indeed, an increase in serum TGF-β1 levels has been noted after chronic resistance training in healthy adults (Hering et al., 2002) and in patients with type 2 diabetes, (Gordon et al., 2006; Touvra et al., 2011). There are no studies reporting an acute RE-induced alteration in TGF-β1 in CAD patients. The positive anti-inflammatory alterations (based on the IL-10 and TGF-β1 concentrations) observed in our study may restrict the magnitude of the inflammatory response to acute RE at a low (50% of 1 RM) and moderate intensity (75% of 1 RM) CAD patients.
Our results have several clinical applications. Inflammatory processes are not only involved in initiating the atherosclerotic disease process, but also in precipitating its complications. A continued activation of cytokines, such as IFN-γ, in the atherosclerotic plaque contributes to the degradation of collagen in the fibrous cap and increases the risk of plaque rupture (Gielen et al., 2005) On the other hand, an increase in serum TGF-β1 functions as an anti-inflammatory growth factor and has an impact on plaque stability. We observed a trend towards a reduction in IFN-γ and increases in TGF-β1 following RE. In the study, IFN-γ concentration did not change with the 50% protocol but TGF-β1 increased while in the 75% protocol IFN-γ decreased and TGF-β1 did not change; therefore both RE intensities may create a favorable environment for plaque stability. Performing RE is of significant clinical importance for CAD patients and may act as an intervention for the reduction of atherosclerotic complications.
In our study we had a small number of low-risk cardiac patients who participated in the exercise program and they also had experience with resistance training. For these reasons and because training status may modify the acute inflammatory responses of exercise, our results cannot be generalized for all patients with CAD and especially for those who participate in exercise for the first time. Furthermore, the repeated bout effect ‘acquired’ as a result of previous exercise exposure cannot be ruled out as a factor which may have impacted the results. Additionally, four of our patients (50%) were on statin therapy and this may have impacted the inflammatory responses to resistance exercise. Finally, it cannot be excluded that some alterations (for example IL-6 or hs-CRP), although not statistically significant, may be of clinical importance. Thus, more studies are required to clarify this topic.
Conclusion
Exercise programs do not only lead to significant physiological improvements in patients with CAD, but may also interfere with the progression of the underlying disease-specific inflammatory process. In this context, the normal pro-and anti-inflammatory responses observed in our study, strengthen the evidence for the implementation of resistance exercise protocols at a low to moderate intensity (50-75% of 1 RM) in low risk, previously trained patients with coronary artery disease.
Acknowledgements
This study was funded by the EPEAEK project (PYTHAGORAS II – 2.2.3.δτ), co-financed by Hellenic (25%) and European Community (75%) funds. On behalf of all authors, the corresponding author states that there is no conflict of interest.
Biographies
Konstantinos VOLAKLIS
Employment
Specialized Scientific Staff
Democritus Univ. of Thrace, Depart. of Physical Education and Sport Science, Depart. of Prevention and Sports Medicine, Technische Universitaet Muenchen, Munich, Germany, 7FIT, Ambulantes Herz-Rehazentrum, Augsburg, Germany
Degree
Ph.D.
Research interests
Cardiac rehabilitation, exercise training in people with chronic disease
E-mail: kvolakli@phyed.duth.gr
Ilias SMILIOS
Employment
Lecturer, Democritus University of Thrace, Department of Physical Education and Sport Science
Degree
Ph.D.
Research interests
Neuromuscular adaptations with various resistance exercise protocols, hormonal responses with resistance exercise, performance improvement with resistance training
E-mail: ismilios@phyed.duth.gr
Apostolos SPASSIS
Employment
Democritus University of Thrace, Department of Physical Education and Sport Science
Degree
Ph.D.
Research interests
Exercise training in cardiac patients, exercise physiology and performance
E-mail: aspassis@phyed.duth.gr
Christos ZOIS
Employment
Democritus University of Thrace, Department of Physical Education and Sport Science
Degree
Ph.D.
Research interests
Exercise testing and training in patients with diabetes, aspects of molecular biology in patients with chronic disease
E-mail: chzois@msn.com
Helen DOUDA
Employment
Assoc. Professor, Democritus University of Thrace, Department of Physical Education and Sport Science
Degree
Ph.D.
Research interests
Exercise physiology and performance, growth and development, kinanthro-pometry, rhythmic gymnastics
E-mail: edouda@phyed.duth.gr
Martin HALLE
Employment
Professor, Department of Prevention and Sports Medicine, Technische Universitaet Munich, Munich, & Munich Heart Alliance, Munich Germany
Degree
MD.
Research interests
Exercise therapy in patients with chronic disease, exercise testing and health screening of professional teams and athletes
E-mail: halle@sport.med.tum.de
Savvas TOKMAKIDIS
Employment
Professor, Democritus University of Thrace, Department of Physical Education and Sport Science
Degree
Ph.D.
Research interests
Exercise and chronic diseases, performance improvement with resistance training, hormonal adaptations with resistance training
E-mail: stokmaki@phyed.duth.gr
References
- American Association of Cardiovascular and Pulmonary Rehabilitation: Guidelines for Cardiac Rehabilitation Programs. (1995) Champaign, Human Kinetics. [Google Scholar]
- Beniamini Y., Rubenstein J.J., Zaichkowsky L.D., Crim M.C. (1997) Effects of high-intensity strength training on quality of life parameters in cardiac rehabilitation patients. American Journal of Cardiology 80(7), 841-846. [DOI] [PubMed] [Google Scholar]
- Bolger A., Sharma R., Von Haehling S., Doehner W., Oliver B., Rauchhaus M., Coats A.J., Adcock I.M., Anker S.D. (2002) Effect of interleukin-10 on the production of tumor necrosis factor-alpha by peripheral blood mononuclear cells from patients with chronic heart failure. American Journal of Cardiology 15(4), 384-389. [DOI] [PubMed] [Google Scholar]
- Brandt C., Pedersen B.K. (2010) The role of exercise-induced myokines in muscle homeostasis and the defense against chronic diseases. Journal of Biomedicine & Biotechnology 520, 258-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988) Statistical power analysis for the behavioral sciences. 2nd edition. Hillside, NJ: L. Erlbaum Associates. [Google Scholar]
- Esposito K., Pontillo A., Di Palo C., Giugliano G., Masella M., Marfella R., Giugliano D. (2003) Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. Journal of the American Medical Association 289(14), 1799-1804. [DOI] [PubMed] [Google Scholar]
- Ewart C.K. (1989) Psychological effects of resistive weight training: implications for cardiac patients. Medicine & Science in Sports & Exercise 21, 683-688. [DOI] [PubMed] [Google Scholar]
- Ghilarducci E., Holly R.G., Amsterdam E.A. (1989) Effects of high resistance training in coronary artery disease. American Journal of Cardiology 64, 866-870. [DOI] [PubMed] [Google Scholar]
- Gielen S., Walther C., Schuler G., Hambrecht R. (2005) Anti-inflammatory effects of physical exercise. A new mechanism to explain the benefits of cardiac rehabilitation? Journal of Cardiopulmonary Rehabilitation 25, 339-342. [DOI] [PubMed] [Google Scholar]
- Gordon P.L., Vannier E., Hamada K., Layne J., Hurley B.F., Roubenoff R., Castaneda-Sceppa C. (2006) Resistance training alters cytokine gene expression in skeletal muscle of adults with type 2 diabetes. International Journal of Immunopathology & Pharmacology 19, 739-749. [DOI] [PubMed] [Google Scholar]
- Hansson G. (2005) Inflammation, atherosclerosis and coronary artery disease. New England Journal of Medicine 352, 1685-1695. [DOI] [PubMed] [Google Scholar]
- Hering S., Jost C., Schulz H., Hellmich B., Schatz H., Pfeiffer H. (2002) Circulating transforming growth factor-β1 (TGF -β1) is elevated in extensive exercise. European Journal of Applied Physiology 86, 406-410. [DOI] [PubMed] [Google Scholar]
- Izquierdo M., Ibañez J., Calbet J.A., Navarro-Amezqueta I., González-Izal M., Idoate F., Häkkinen K., Kraemer W.J., Palacios-Sarrasqueta M., Almar M., Gorostiaga E.M. (2009) Cytokine and hormone responses to resistance training. European Journal of Applied Physiology 107, 397-409. [DOI] [PubMed] [Google Scholar]
- Kelemen M.H., Stewart K.J., Gillilan R.E., Ewart C.K., Valenti S.A., Manley J.D., Kelemen M.D. (1986) Circuit weight training in cardiac patients. Journal of American College of Cardiology 7, 38-42. [DOI] [PubMed] [Google Scholar]
- Keppel G. (1991) Design and analysis: A researcher’s handbook. 3rd edition. Upper Saddle River, NJ: Prentice-Hall Inc. [Google Scholar]
- Lutgens E., Gijbels M., Smook M., Heeringa P., Gotwals P., Koteliansky V.E., Daemen M.J. (2002) Transforming growth factor-β mediates balance between inflammation and fibrosis during plaque progression. Arteriosclerosis Thrombosis & Vascular Biology 22, 975-982. [DOI] [PubMed] [Google Scholar]
- Mathur N., Pedersen B.K. (2008) Exercise as a mean to control low-grade systemic inflammation. Mediators of Inflammation 109, 1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCartney N., McKelvie R., Haslam D., Jones N.L. (1991) Usefulness of weightlifting training in improving strength and maximal power output in coronary artery disease. American Journal of Cardiology 67, 939-945. [DOI] [PubMed] [Google Scholar]
- Medham A.E., Donges C.E., Liberts E.A., Duffield R. (2011) Effects of mode and intensity on the acute exercise-induced IL-6 and CRP responses in a sedentary, overweight population. European Journal of Applied Physiology 111, 1035-1045. [DOI] [PubMed] [Google Scholar]
- O’Callaghan C.J., Williams B. (2000) Mechanical strain– induced extracellular matrix production by Human vascular smooth muscle cells. Role of TGF-b1. Hypertension 36, 319-324. [DOI] [PubMed] [Google Scholar]
- Peake JM., Nosaka K., Muthalib M., Suzuki K. (2006) Systemic inflammatory responses to maximal versus submaximal lengthening contractions of the elbow flexors. Exercise Immunology Reviews 12, 72-85. [PubMed] [Google Scholar]
- Pedersen B.K., Akerström T.C.A., Nielsen A.R., Fischer C.P. (2007) Role of myokines in exercise and metabolism. Journal of Applied Physiology 103, 1093-1098. [DOI] [PubMed] [Google Scholar]
- Pedersen B.K., Febbraio M.A. (2008) Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiology Reviews 88(4), 1379-1406. [DOI] [PubMed] [Google Scholar]
- Petersen A.M.W., Pedersen B.K. (1995) The anti-inflammatory effect of exercise. Journal of Applied Physiology 98(4), 1154-1162. [DOI] [PubMed] [Google Scholar]
- Phillips M.D., Mitchell J.B., Currie-Elolf L.M., Yellott R.C., Hubing K.A. (2010) Influence of commonly employed resistance exercise protocols on circulating IL-6 and indices of insulin sensitivity. Journal of Strength and Conditioning Research 24, 1091-1101. [DOI] [PubMed] [Google Scholar]
- Smith L.L., Anwar A., Fragen M., Rananto C., Johnson R., Holbert D. (2000) Cytokines and cell adhesion molecules associated with high-intensity eccentric exercise. European Journal of Applied Physiology 82, 61-67. [DOI] [PubMed] [Google Scholar]
- Sparling P.B., Cantwell J.D., Dolan C.M. (1990) Strength training in a cardiac rehabilitation program. a six month follow up. Archives of Physical Medicine & Rehabilitation 71, 148-152. [PubMed] [Google Scholar]
- Touvra A.M., Volaklis K., Spassis A., Zois C.E., Douda H.D., Kotsa K., Tokmakidis S.P. (2011) Combined strength and aerobic training increases transforming growth factor-β1 in patients with type 2 diabetes. Hormones 10(2), 125-130. [DOI] [PubMed] [Google Scholar]
- Uchida M.C., Nosaka K., Ugrinowitsch C., Yamashita A., Martins E., Jr., Moriscot A.S., Aoki M.S. (2009) Effect of bench press exercise intensity on muscle soreness and inflammatory mediators. Journal of Sports Sciences 27, 499-507. [DOI] [PubMed] [Google Scholar]
- Williams M.A., Haskell W.L., Ades A.A., Amsterdam E.A., Bittner V., Franklin B.A., Gulanick M., Laing S.T., Stewart K.J. (2007) Resistance exercise in individuals with and without cardiovascular disease: 2007 Update: A scientific statement from the American Heart Association council on clinical cardiology and council on nutrition, physical activity and metabolism. Circulation 116, 572-584. [DOI] [PubMed] [Google Scholar]


