Abstract
The current study evaluates associations between control processes and Oppositional Defiant Disorder (ODD) and attention deficit hyperactivity disorder (ADHD) during early childhood. Participants were 98 children between ages 3 and 6 and their primary caregivers. Diagnostic information on ODD and ADHD symptoms was available from parents and teachers/caregivers via standardized rating forms. Affective, effortful, and cognitive control processes were measured using parent and examiner ratings via standardized questionnaires, observational ratings, and child performance on laboratory tasks of cognitive control. Affective control, but not effortful control, was significantly associated with cognitive control. A latent factor of control was significantly associated with ADHD, but not ODD, symptoms.
Children demonstrate dramatic gains in control processes between the ages of 3 and 6. During this developmental period, children begin to actively develop these rudimentary regulation skills in the affective, cognitive, and behavioral domains via rapidly developing limbic and neocortical circuitry (Casey, Tottenham, Liston, & Durston, 2005) and in the context of parental socialization (Eisenberg, Spinrad, & Eggum, 2010). Further, disorders of dysregulation such as Disruptive Behavior Disorders (DBD), including Oppositional Defiant Disorder (ODD) and arguably attention deficit hyperactivity disorder (ADHD) are first able to be reliably diagnosed during this developmental period (Keenan & Wakschlag, 2002; Task Force on Research Diagnostic Criteria: Infancy and Preschool, 2003).
Per the Diagnostic and Statistical Manual of Mental Disorders (4th ed. [DSM-IV-TR]; American Psychiatric Association, 2000) the most common DBD occurring during early childhood are ODD and arguably ADHD (particularly hyperactivity-impulsivity vs. inattention). ODD and ADHD occur in approximately 5–10% of the general population (Egger & Angold, 2006; Lavigne et al., 1996) and affect approximately 10% of preschool-age children (Egger & Angold, 2006). These disorders are frequently comorbid, co-occurring in approximately 50% of cases (Angold, Costello, & Erkanli, 1999). Therefore, it makes sense to study them together. Further, these disorders are associated with increased risk for later psychopathology, as well as social and academic problems (Foster, Jones, & the Conduct Problems Prevention Research Group, 2005; Pelham, Foster, & Robb, 2007). Recent work suggests that a common liability factor for these disorders and perhaps particularly ADHD may be disinhibition, or poor regulation of affect and cognition (Krueger et al., 2002; Nigg, 2000).
Although disinhibition has been suggested as a prominent correlate and perhaps an early-emerging marker of DBD (Krueger et al., 2002; Martel, 2009), the definition of disinhibition, or dysregulated affect and cognition, is very broad, and there is a long tradition of alternative measurements of the construct at different levels of analysis (e.g., Nigg, 2000). Affective regulation is typically defined as the modulation of emotional responses via control processes that occur somewhat reflexively (Cole, Martin, & Dennis, 2004). Affective regulation is often assessed using temperamental measures (e.g., reactive control, emotional regulation; Eisenberg & Spinrad, 2004). Children with ODD and ADHD often experience problems controlling their emotions (reviewed by Martel, 2009). In fact, poor affective, or reactive, control during preschool predicts the later longitudinal development of DBD-related behaviors in school-aged children (Eisenberg et al., 2009), perhaps particularly hyperactivity-impulsivity and ODD (Martel & Nigg, 2006).
Effortful control is a temperament trait that refers to thoughtful, deliberate temperamental control and has been conceptually related to cognitive regulation (Nigg, 2000; Rueda, Posner, & Rothbart, 2005). Effortful control exhibits associations with cognitive regulation by middle childhood, or between ages 8 and 10 (Martel, Nigg, & von Eye, 2009; Rueda et al., 2005). Low effortful control during preschool has also been associated with the longitudinal development of ODD and ADHD and more general externalizing problems in school-aged children (Eisenberg et al., 2009; Kochanska, Barry, Jiminez, Hollatz, & Woodard, 2009). Further, low effortful control and the somewhat synonymous personality trait of conscientiousness have been linked to clinical ADHD and ODD in school-aged children (De Pauw & Mervielde, 2011; Martel & Nigg, 2006), perhaps particularly those displaying high levels of inattention (vs. hyperactivity-impulsivity; Martel & Nigg, 2006).
Cognitive regulation is often referred to as cognitive control, or executive function, meaning the ability to problem-solve to obtain a future goal (see Pennington & Ozonoff, 1996). Cognitive control, although a unitary construct, contains several componential, or more specific, abilities (Miyake, Friedman, Emerson, Witzki, & Howerter, 2000). These abilities commonly include response inhibition, or inhibition of a dominant response in order to perform a subordinate response; set-shifting, or multitasking; and working memory, or the ability to manipulate information in short-term memory (Pennington & Ozonoff, 1996; Miyake et al., 2000). Substantial work has linked these types of poor cognitive control to behavioral problems, perhaps most specifically ADHD, in school-aged children between the ages of 6 and 12. School-aged children with DBD, including ODD and ADHD, often experience problems with cognitive control, or executive function, including response inhibition, set-shifting, and working memory, and these deficits are typically viewed as being more specific to ADHD than ODD (Barkley, 1997; Willcutt, Doyle, Faraone, & Pennington, 2005). Increasingly, similar patterns of findings have been found in preschool-aged children with ADHD, who are often characterized by problems with cognitive control (Thorell & Wahlstedt, 2006). Further, cognitive control deficits appear to be most specifically associated with inattentive ADHD symptoms (vs. hyperactive-impulsive ADHD symptoms; Sonuga-Barke, 2003).
Thus, in line with multiple pathway models suggesting somewhat distinct influences on different DBD symptom dimensions (e.g., Sonuga-Barke, 2003), affective dysregulation may be associated with both ODD and ADHD (perhaps particularly hyperactivity-impulsivity), and effortful and cognitive dysregulation may be most specifically associated with ADHD (and perhaps particularly inattention) during middle childhood. By middle childhood, affective and cognitive forms of regulation are largely developed and highly inter-correlated such that children who have strong affective and cognitive regulation typically exhibit few behavioral problems related to DBD, and children with weak affective and cognitive regulation typically exhibit increased behavioral problems related to DBD (Eisenberg et al., 1996; Murphy & Kochanska, 2002). However, earlier developmental associations among affective regulation, cognitive regulation, and DBD remain unclear. Affective, cognitive, and behavioral regulation all develop substantially during the preschool age range (Garon, Bryson, & Smith, 2008). Affective regulation is typically viewed as developing earliest due to its reliance on subcortical structures and its important role in early socialization (Casey et al., 2005; Nigg & Casey, 2005). Cognitive forms of control, and possibly effortful temperamental control, are typically viewed as developing slightly later due to their reliance on the prefrontal cortex and anterior cingulate gyrus and their facilitation of individual-driven influences on the environment (Casey et al., 2005; Nigg & Casey, 2005). In line with this idea, DBD symptoms such as ODD and hyperactivity-impulsivity, which are hypothesized to depend on affective control, typically peak early during development and then decline; whereas DBD symptoms such as inattention, that are believed to depend more on cognitive control, usually start later and are relatively stable (Greven, Asherson, Rijsdijk, & Plomin, 2011; Lahey, Pelham, Loney, Lee, & Willcutt, 2005).
More primary forms of affective regulation may provide the foundation for the slightly later development of cognitive and behavioral regulation. However, this idea remains untested since it is seldom that all three types of regulation are included in any given study, particularly in studies examining relevant clinical populations such as preschool-aged children with DBD including ODD and ADHD. The current study provides an initial examination of early-emerging affective and cognitive control processes in a cross-sectional sample of children between ages 3 and 6 with ODD and/or ADHD. Since early childhood is the earliest developmental period during which affective and cognitive forms of regulation can be reliably measured, this may be the ideal time to examine the inter-relations among these emerging forms of control in relation to disorders of behavioral dysregulation such as DBD. Due to the rapid development of underlying neural anatomy during preschool, control processes may exhibit more distinct associations with one another and forms of DBD such as ODD and ADHD during this period. Because affective forms of regulation develop as early as infancy, it was predicted that affective control would exhibit the most prominent associations with other emerging forms of control, including cognitive control, during preschool. In addition, it was predicted that affective, effortful, and cognitive control processes would be most specifically associated with ADHD symptoms during preschool.
Methods
Participants
Overview
Participants were 98 children between the ages of 3 and 6 (M = 4.34 years, SD = 1.08) and their primary caregivers (hereafter termed parents for simplicity; 67% mothers with the remaining 33% fathers+mothers, fathers only, foster parents, or grandmothers with guardianship). Fifty-seven percent of the sample was male, and 32% of the sample was ethnic minority (23% African American and 8% other including Latino, American Indian, and mixed race children). Parental educational level ranged from unemployed to highly skilled professionals, with incomes ranging from below $20,000 to above $100,000 annually. Based on multistage and comprehensive diagnostic screening procedures (detailed below), children were recruited into two groups: DBD (n = 74), subdivided into those with ADHD-only (n = 17), those with ODD-only (n = 18), and those with ADHD+ODD (n = 39); and children without DBD (n = 24). The non-DBD group included children with subthreshold symptoms (i.e., fewer than 4 ODD symptoms or 6 ADHD symptoms) to provide a more continuous measure of ADHD and ODD symptoms, consistent with research suggesting that ODD and ADHD may be better captured by continuous dimensions than categorical diagnosis (Marcus & Barry, 2011). No siblings were included.
Recruitment and identification
Participants were recruited from the community primarily through direct mailings to families with children between the ages of 3 and 6 and Internet postings, as well as through advertisements in newspapers and flyers posted at doctors' offices, community centers, daycares, and on campus bulletin boards. Two sets of advertisements were utilized; one set of advertisements targeted children between ages 3 and 6 with disruptive behavior problems and/or attention problems and a second set of advertisements targeted children between ages 3 and 6 without these types of problems. After recruitment, families passed through a multi-gated screening process. An initial telephone screening was conducted to rule out children prescribed long-acting psychotropic medication (i.e., antidepressants) or children with neurological impairments, mental retardation, psychosis, autism spectrum disorders, seizure history, head injury with loss of consciousness, or other major medical conditions. Only 10 families were screened out at this phase. All families screened into the study at this point completed written and verbal informed consent procedures consistent with the Institutional Review Board, the National Institute of Mental Health, and American Psychological Association (APA) guidelines.
During the second stage, parents and children attended a three-hour campus laboratory visit. Parents of children taking psycho-stimulant medication were asked to consult with a physician about discontinuing children's medication for 24 to 48 hours prior to the visit depending on their dosage and type of medication in order to ensure a more accurate measure of cognitive performance (less than 5% of children in the study were prescribed medication for attention problems). Before and during the laboratory visit, diagnostic information was collected via parent and teacher/caregiver ratings. Parents completed the Kiddie Disruptive Behavior Disorders Schedule (K-DBDS: Leblanc et al., 2008), a semi-structured diagnostic interview modeled after the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children administered by a trained graduate student clinician. Questions about endorsed DBD symptoms were followed by questions that determine symptom severity, duration, onset, and cross-situational pervasiveness. For endorsed symptoms to count toward ADHD diagnosis, the symptom must have been present in more than one setting (i.e., school, home, or public) and must have occurred frequently compared to same-aged peers. The K-DBDS demonstrates high test–retest reliability and high inter-rater reliability in the preschool population (LeBlanc et al., 2008). In the current study, fidelity to interview procedure was determined via stringent check-out procedures before interview administration. In addition, reliability of interviewer ratings was determined by blind ratings of interviews of each interviewer on 10% of families. Inter-rater clinician agreement was adequate for ODD and ADHD symptoms (r = .99, p < .001, r = 1.00, p < .001, respectively).
Families were mailed teacher/caregiver questionnaires one week prior to the laboratory visit and instructed to provide the questionnaires to children's teacher and/or daycare provider or babysitters who then mailed the completed questionnaires back to the university. When available (i.e., available on 50% of participating families; response rate did not differ based on child DBD diagnostic group; χ2[3] = .59, p = .9), teacher/caregiver report on DBD symptoms was obtained via report on the Disruptive Behavior Rating Scale (DBRS; Barkley & Murphy, 2006). In the current study, approximately 67% of completed teacher/caregiver report was available from teachers, with most of the remaining questionnaires completed by daycare providers or babysitters. Some families did not have teacher/caregiver report available because they could not identify a second reporter; however, in most cases of missing data, teachers/caregivers did not return the questionnaire measures.
Ultimately, clinical diagnoses were determined by the Principal Investigator, a licensed clinical psychologist, after a review of parent ratings on the K-DBDS and (when available) teacher/caregiver ratings on the DBRS, consistent with current best practice guidelines for current diagnosis (Pelham, Fabiano, & Massetti, 2005). A second blind diagnostician also independently reviewed parent and teacher ratings of child symptoms to reach a diagnosis on a random 10% of cases with a 100% agreement rate (kappa = 1).
Measures
Symptom counts
Parent and teacher/caregiver reports on symptoms were available via the DBRS (Barkley & Murphy, 2006), which assesses symptoms using a 0 to 3 scale for a more continuous dimension and is valid for use with preschoolers. Endorsed symptoms are summed within each diagnostic subdomain (i.e., ODD symptoms, ADHD total symptoms, inattentive ADHD symptoms, hyperactive-impulsive ADHD symptoms) to determine symptom counts within these categories. The DBRS has high internal consistency ranging from .78 to .96 in the preschool age range (Pelletier, Collett, Gimple, & Cowley, 2006). All scales for parent and teacher/caregiver report on the DBRS had high internal reliability (all alphas > .92) in the current sample. Primary analyses were conducted using parent report on the DBRS with secondary checks conducted on teacher report on the DBRS.
Affective control
To measure affective control, an examiner completed the California Child Q-Sort (CCQ; Block & Block, 1980) after spending 3 hours interacting with the child during the on-campus laboratory visit. The CCQ is a typical Q-Sort consisting of 100 cards that must be placed in a forced-choice, nine-category, rectangular distribution. The rater describes the child by placing descriptive cards in one of the categories, ranging from one (least descriptive) to nine (most descriptive). A 19-item scale for affective control (also called reactive control) developed by Eisenberg and colleagues (1996) for use with young children was utilized (e.g., “inhibited and constricted,” “self assertive”). The composite scale score was generated by reverse-scoring selected items and computing the average. Scale reliability was .86. In addition, a paradigm from the preschool Laboratory Temperament Assessment Battery (LABTAB), gift delay, was utilized (Goldsmith, Reilly, Lemery, Longley, & Prescott, 1999; Kochanska, Murray, & Harlan, 2000). Children were asked to wait with their back turned while the examiner wrapped a present; the child was instructed not to touch the gift while the examiner left to room to retrieve a bow for the present. Extent of peeking for the entire segment was coded on a five point scale (1 = child peeks the entire time; 5 = child never peeks). Reliability was acceptable for all observational coding in the current study (all kappas > .78).
Effortful control
To measure effortful temperamental control, parents completed the very short form of the Child Behavior Questionnaire (CBQ) for use in children between ages 3 and 7 (Rothbart, Ahadi, Hershey, & Fisher, 2001; Putnam & Rothbart, 2006). The very short form of the CBQ contains 36 descriptive statements that parents rate on a 1 (extremely untrue of your child) to 7 (extremely true of your child) scale. Effortful control was measured using the 12-item scale suggested by Rothbart and colleagues (2001). A composite scale score was generated by reverse-scoring selected items and computing the average. The scale had an acceptable internal reliability coefficient of.70 in the current sample.
Cognitive control
Selected cognitive control tasks assessing response inhibition, working memory, and set-shifting were utilized, based on their validity and sensitivity in the preschool population and their reliance on prefrontal cortex and frontal-striatal circuitry (Garon et al., 2008). In order to measure response inhibition, the Shape School was used. The Shape School uses a bright, large storybook format with stimulus figures (i.e., colored circles and squares with happy and sad facial expressions, some of which wear hats; Espy, Bull, Martin, & Stroup, 2006). The task has four conditions and each is preceded by a short practice. The second condition provides a measure of response inhibition and entails having the child name the colors of happy-faced figures while being asked to inhibit naming of the colors of sad-faced figures. Number of correctly identified stimuli divided by time to complete the second trial served as a measure of response inhibition. This task has adequate reliability with test–retest reliability ranging from .65 to .78, and alpha coefficients exceeding .71 for the second condition within this age range (Isquith, Crawford, Espy, & Gioia, 2005). Backward Digit Span served as a measure of simple and complex working memory. In Digit Span backward condition, the child is instructed to repeat a series of numbers in the reverse order heard. The total of correctly completed items for this condition provided a measure of working memory (Garon et al., 2008). In order to assess set-shifting, an adaptation of the Trail-Making Task, TRAILS-P (Espy & Cwik, 2004), was administered. Condition B provides a measure of set-shifting. During condition B, the switching condition, children are asked to stamp pictures of dogs and bones in order of size, alternating between the two. Number of errors made in condition B served as a measure of set-shifting. This task has good test–retest reliability across a 2-week period with mean correlations of.64 between conditions within this age range (Isquith et al., 2005).
Data Analysis
Missingness was minimal in the current study, with the exception of teacher ratings on the DBRS. Only 50% of children in the current sample had teacher ratings on the DBRS available due to poor response rate. The missingness and nonnormality of data (i.e., symptom counts) were addressed using robust full information maximum likelihood estimation (FIML; i.e., direct fitting) in Mplus (Múthen & Múthen, 1998–2007), a method of directly fitting models to raw data without imputing data (McCartney, Burchinal, & Bub, 2006). Power analysis indicated that statistical power was adequate (.80) to detect a medium-size effect (r = .25).
Data analysis proceeded in a step-wise fashion. Preliminary statistics were conducted in SPSS. Chi-square tests and univariate analysis of variance (ANOVA) were conducted to examine mean differences between the ODD, ADHD, ODD+ADHD, and non-ODD/ADHD groups on demographic variables. Next, main analyses were conducted in Mplus using bivariate and partial correlations and confirmatory factor analysis; the latent factor score was saved and utilized in subsequent correlational analyses (Raykov, 1997). In order to correct for Type I error, correlations between control and DBD symptoms are only interpreted if p < .01.
Results
Preliminary evaluation of group differences on demographic variables indicated that there were no significant differences between the ODD, ADHD, ADHD+ODD, or non-DBD group in percentage of boys/girls (X2[3] = .85, p = .84), ethnicity minority status (X2[12] = 17.002, p = .15), or maternal education or employment status (X2[24] = 25.95, p = .36 for education; X2[15] = 13.89, p = .53 for employment). However, children with ODD, ADHD, and ODD+ADHD were significantly older than the non-DBD comparison children (F[3,94] = 2.85, p = .04) and were from families with lower incomes (X2[15] = 28.63, p = .02) Therefore, child age and family income was covaried in all analyses involving DBD symptoms.
Bivariate correlations were conducted to examine associations between parent- and teacher-reported child DBD symptoms (not shown). Bivariate correlations of parent and teacher DBD symptom ratings within domain were all significant and at least in the moderate range (r range from .52 to .59, all p < .01). Correlations among DBD symptom domains (e.g., among ODD, hyperactivity-impulsivity, and inattention) within informant were also significant and moderate (r = .6, p< .01 or above for parents; r = .32, p < .05 or above for teachers).
Partial correlations, controlling for child age, were conducted between affective, effortful, and cognitive control and parent- and teacher-rated child DBD symptoms (ODD, ADHD, inattention, and hyperactivity-impulsivity). As shown in Table 1, examiner-rated affective control was not significantly associated with any parent- or teacher-rated DBD symptom domain (all p > .1). However, decreased observationally-rated affective control (measured via the gift delay task) was associated with increased parent- and teacher-rated ADHD symptoms, specifically inattention as rated by parents and hyperactivity-impulsivity as rated by parents and teachers (all p < .05). Decreased parent-rated effortful control was significantly associated with increased parent-rated ODD symptoms (p < .05). Worse response inhibition and working memory was significantly associated with increased teacher-rated inattentive ADHD symptoms (p < .05), but not parent-rated symptoms. Worse set-shifting was significantly associated with increased ADHD symptoms and increased inattention, as rated by parents and teachers (all p < .05).
Table 1. Partial Correlations Between Control and DBD Symptoms.
| ODD | ADHD | Inattention | Hyperactivity-Impulsivity | |
|---|---|---|---|---|
| Reactive Control | −.09 (−.22) | −.24 (−.04) | −.18 (.09) | −.28 (−.18) |
| Gift Delay: Peek | −.18 (−.45) | −.55* (−.45*) | −.51 (−.28) | −.53* (−.56*) |
| Effortful Control | −.48* (−.43+) | −.22 (−.1) | −.18 (−.03) | −.24 (−.17) |
| Response Inhibition | −.2 (−.23) | −.35 (−.44+) | −.35 (−.53*) | −.31 (−.26) |
| Set-Shifting | .37(.12) | .50* (.33) | .58** (.46*) | .38 (.13) |
| Working Memory | −.19 (−.42+) | −.3 (−.54*) | −.3 (−.54*) | −.26 (−.43+) |
Note. Age and family income covaried. Parent-rated symptoms (teacher-rated symptoms). ADHD = attention deficit hyperactivity disorder; ODD = Oppositional Defiant Disorder.
p < .01.
p < .05.
p < .1.
Associations Among Affective, Effortful, and Cognitive Control
Bivariate correlations were conducted between measures of affective, effortful, and cognitive control. As shown in Table 2, affective control was significantly associated with components of cognitive control (i.e., response inhibition, set-shifting, and working memory) in the expected direction with worse affective control being correlated with worse cognitive control (r = .26–.3; p < .05). However, effortful control was not significantly associated with affective control or components of cognitive control (r = –.01–.16; all p > .1).
Table 2. Correlations Between Measures of Affective, Effortful, and Cognitive Control.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Affective Control | 1 | .30* | .06 | .28** | −.18 | .26* |
| Gift Delay: Peek | 1 | .07 | .51** | −.32* | .43** | |
| Effortful Control | 1 | .16 | −.01 | .1 | ||
| Response Inhibition | 1 | −.3** | .61** | |||
| Set-Shifting | 1 | −.3** | ||||
| Working Memory | 1 |
p < .05.
p < .01.
Based on these results, a confirmatory factor analysis was conducted in order to attempt to identify a latent factor of control from components of cognitive control (i.e., response inhibition, set-shifting, and working memory) and affective control. The fit of the one-factor model was good (X2[5] = 3.12, p = .68; CFI = 1; RMSEA = 0 with a 90% confidence interval of 0–.11; McDonald & Ho, 2002). As shown in Figure 1, all loadings are significant (all p < .01) and in the expected direction. Based on these loadings, the factor was labeled “control”; higher scores on the latent factor indicated better cognitive and affective control. Individual scores on the latent factor were saved for subsequent analyses.
Figure 1.
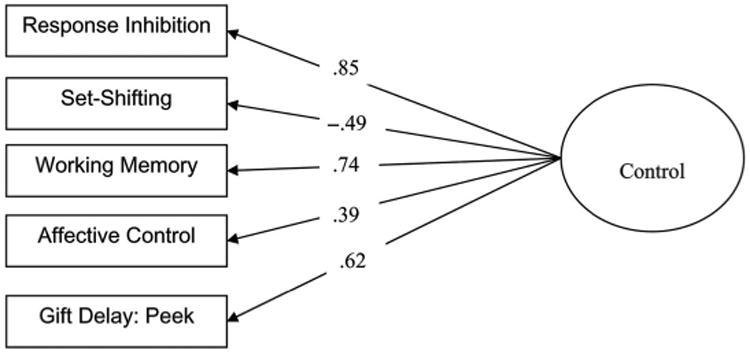
Latent factor model of control. X2(5) = 3.122, p = .68. CFI = 1; RMSEA = 0 with a 90% confidence interval of 0–.11. All loadings are significant at p < .01.
Associations Between Control and DBD
Partial correlations, controlling for child age and family income, were conducted between the latent factor of control and DBD symptoms. As shown in Table 3, better control was significantly associated with decreased parent-rated ADHD symptoms (r = –.39, p < .01), but not with parent-rated ODD symptoms (r = .1, p = .37). These correlations were significantly different from one another (z = –3.53, p < .01). Within ADHD, better control was significantly associated with decreased parent-rated hyperactivity-impulsivity (r = –.37, p < .01), but not parent-rated inattention (r = .02, p = .91), and these correlations were also significantly different from one another (z = –2.81, p < .01). Secondary analyses conducted using teacher-rated symptoms were similar (Table 3). Better control was significantly associated with decreased teacher-rated ADHD symptoms (r = –.41, p < .01), but not teacher-rated ODD symptoms (r = .09, p = .42; significant difference z = –3.62, p < .01). However, better control was significantly associated with decreased teacher-rated inattention (r = –.43, p < .01), but not with teacher-rated hyperactivity-impulsivity (r = .03, p = .85; significant difference z = –3.38, p < .01).
Table 3. Correlations Between Control Latent Factor and DBD Symptom Domains.
| Control | |
|---|---|
| ODD symptoms (parent-rated; p) | .1 |
| ADHD symptoms (p) | −.39** |
| Inattentive symptoms (p) | .02 |
| Hyperactive-impulsive symptoms (p) | −.37** |
| ODD symptoms (teacher-rated; t) | .09 |
| ADHD symptoms (t) | −.41** |
| Inattentive symptoms (t) | −.43** |
| Hyperactive-impulsive symptoms (t) | .03 |
Note. Age and family income covaried. ADHD = attention deficit hyperactivity disorder; ODD = Oppositional Defiant Disorder.
p < .01.
Discussion
The current study examined emerging forms of affective, effortful, and cognitive control in children with DBD and ADHD. Cognitive control was significantly associated with affective temperamental control, but not with effortful temperamental control. Indices of cognitive control and affective (reactive) control formed a latent control factor, termed control. Control was significantly associated with ADHD symptoms, but not ODD symptoms, during early childhood. Specifically, better control was significantly associated with decreased parent-rated hyperactive-impulsive ADHD symptoms, but not parent-rated inattentive ADHD symptoms, and with decreased teacher-rated inattentive ADHD symptoms, but not teacher-rated hyperactive-impulsive ADHD symptoms.
Affective temperamental control, but not effortful temperamental control, was associated with cognitive forms of control during early childhood. This finding is counter to prior work conducted in school-age children in which effortful temperamental control is frequently found to be prominently associated with cognitive control (e.g., Martel et al., 2009; Rueda et al., 2005). Characteristics of the sample or the instruments utilized to measure the constructs may explain this finding and that is an important direction for future work. For example, age range and the high percentage of clinical cases in the sample may have influenced results. Affective forms of regulation are believed to develop early during development due to their reliance on subcortical structures, and they may serve as the early foundation of the later development of more effortful forms of regulation by facilitating parental socialization of emotion regulation (Casey et al., 2005; Cole et al., 2004; Nigg & Casey, 2005). Then, cognitive control, which is just beginning to develop during this period due to its reliance on the prefrontal cortex and anterior cingulate gyrus, allows children to learn from their environment and may provide a foundation for dispositional effortful control (Casey et al., 2005; Nigg & Casey, 2005). Effortful control may, in turn, facilitate children's ability to influence their environment, including success at academics (Bull, Espy, & Wiebe, 2008). In this way, more primary forms of affective regulation may provide the foundation for the development of cognitive and behavioral regulation important in the expression and regulation of DBD-related behaviors. These processes may become dysfunctional in clinical populations such as in children with DBD. Of course, it is possible that the choice of measurement instruments may have influenced associations.
Cognitive forms of control including response inhibition, set-shifting, and working memory, and affective control seem to tap into emerging control during early childhood. Affective control may very well underpin early cognitive control during this period (Carlson & Wang, 2007; Liebermann, Giesbrecht, & Muller, 2007). Better control was significantly associated with ADHD, but not ODD symptoms, during early childhood, in line with work suggesting that disinhibition is a primary deficit of ADHD (Barkley, 1997; Nigg, 2000), emerging as early during development as ADHD can be reliably measured and potentially even predisposing individuals to ADHD (Brocki, Nyberg, Thorell, & Bohlin, 2007; Thorell & Wahlstedt, 2006). ADHD may thus be characterized by delays in cortical maturation that contributes to deficits in emerging forms of control even measured as early as preschool (Shaw et al., 2007). Control was not significantly associated with ODD symptoms, in line with recent work suggesting that ODD may be best considered a disorder of high negative affect rather than a disorder primarily characterized by poor cognitive control (Stringaris, Maughan, & Goodman, 2010).
However, associations between control and specific ADHD symptom domains were dependent on the rater. Control was significantly associated with hyperactivity-impulsivity, but not inattention, based on parent report. In contrast, control was significantly associated with inattention, but not hyperactivity-impulsivity, based on teacher report. Parents and teachers appear to be sensitive to different kinds of child problem behaviors relevant to ADHD, depending on the specific context, in line with work suggesting that parents and teachers are each valid reporters of ADHD symptoms (Ferdinand et al., 2003). That is, hyperactivity-impulsivity may be a particularly prominent behavioral manifestation of preschool ADHD in the home, whereas inattention may be more salient in the school setting (Lahey et al., 2005). Further, specificity of associations between emerging control and ADHD symptom domains is in line with recent multiple-pathway models of ADHD, suggesting somewhat specific correlates of inattention versus hyperactivity-impulsivity (e.g., Sonuga-Barke, 2003), although specific effects may depend on rater. Regardless of what symptom domain is particularly associated with poor emerging control, problems with emerging control seem to be particularly associated with ADHD versus ODD.
Despite the rich sample and the multi-method assessment procedure utilized in the current study, the current study had several important limitations. The current study utilized a cross-sectional design with temperamental, behavioral, and cognitive control measured at only one time point. Thus, longitudinal associations between emerging control and DBD symptoms cannot be directly assessed. However, use of a young sample of children with DBD provides important new information about the early manifestation of these types of regulation in relation to DBD. Second, only about 50% of teachers/caregivers returned questionnaires on child DBD symptoms; thus, divergence of findings between parent and teacher ratings is difficult to interpret. Although the multiple-informant, multiple-method assessment approach was considered a study strength, other measures might have been useful in operationalizing cognitive control constructs. Finally, although the use of a community-recruited sample enriched for clinical DBD symptoms is considered a study strength, the current findings should be replicated in other types of samples, including general population and clinical samples.
A key question that remains unresolved from this cross-sectional study is whether control processes can predict the longitudinal development of ADHD symptoms during early and later childhood. Thus, an important direction for future work is short-term longitudinal studies examining whether early-emerging temperamental and cognitive control can predict the later development of ADHD symptoms. This same type of longitudinal design would be useful for assessing changes in associations in temperamental, behavioral, and cognitive control over time, particularly during key developmental periods when neural development is notable (e.g., between preschool and early childhood; adolescence). Finally, examination of these processes in general population samples and clinical samples would be useful in order to elucidate how the development of control processes occurs in these different populations.
Overall, the current study suggests that affective control, but not effortful control, was significantly associated with cognitive control as a prominent form of control during early childhood in children with DBD and ADHD. This latent control composite was significantly associated with ADHD, but not ODD, symptoms during early childhood in line with the idea that ADHD is an early-emerging disorder of disinhibition. Further, control was specifically associated with hyperactivity-impulsivity, based on parent report, but with inattention, based on teacher report, suggesting that parents and teachers are each assessing different, but valid, components of ADHD.
Acknowledgments
We are indebted to the families who made this study possible.
This research was supported by National Institute of Health and Human Development grant 5R03 HD062599-02 to M. Martel.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th Text Rev. Washington, DC: Author; 2000. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- Barkley RA. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121(1):65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR. Attention-deficit hyperactivity disorder: A clinical workbook. 3rd. New York, NY: The Guilford Press; 2006. [Google Scholar]
- Block JH, Block J. The role of ego-control and ego-resiliency in the organization of behavior. In: Collins WA, editor. Minnesota symposia on child psychology. Vol. 13. Hillsdale, NJ: Erlbaum; 1980. pp. 39–101. [Google Scholar]
- Brocki KC, Nyberg L, Thorell LB, Bohlin G. Early concurrent and longitudinal symptoms of ADHD and ODD: Relations to different types of inhibitory control and working memory. Journal of Child Psychology and Psychiatry. 2007;48(10):1033–1041. doi: 10.1111/j.1469-7610.2007.01811.x. [DOI] [PubMed] [Google Scholar]
- Bull R, Espy RA, Wiebe SA. Short-term memory, working memory, and executive functioning in preschoolers: Longitudinal predictors of mathematical achievement at age 7 years. Developmental Neuropsychology. 2008;33(3):205–228. doi: 10.1080/87565640801982312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson SM, Wang TS. Inhibitory control and emotion regulation in preschool children. Cognitive Development. 2007;22:489–510. [Google Scholar]
- Casey BJ, Tottenham N, Liston C, Durston S. Imagining the developing brain: What have we learned about cognitive development? Trends in Cognitive Science. 2005;9(3):104–110. doi: 10.1016/j.tics.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: Methodological challenges and directions for child development research. Child Development. 2004;75(2):317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- De Pauw SSW, Mervielde I. The role of temperament and personality in problem behaviors of children with ADHD. Journal of Abnormal Child Psychology. 2011;39(2):277–291. doi: 10.1007/s10802-010-9459-1. [DOI] [PubMed] [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47(3/4):313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Guthrie IK, Murphy BC, Maszk P, Holmgren R, Suh K. The relations of regulation and emotionality to problem behavior in elementary school children. Development and Psychopathology. 1996;8:141–162. [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL. Emotion-related regulation: Sharpening the definition. Child Development. 2004;75(2):334–339. doi: 10.1111/j.1467-8624.2004.00674.x. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL, Eggum ND. Emotion-related self-regulation and its relation to children's maladjustment. Annual Review of Clinical Psychology. 2010;6:495–525. doi: 10.1146/annurev.clinpsy.121208.131208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Valiente C, Spinrad TL, Cumberland A, Liew J, Reiser M, et al. hellip Losoya SH. Longitudinal relations of children's effortful control, impulsivity, and negative emotionality to their externalizing, internalizing, and co-occurring behavior problems. Developmental Psychology. 2009;45(4):988–1008. doi: 10.1037/a0016213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espy KA, Bull R, Martin J, Stroup W. Measuring the development of executive control with the Shape School. Psychological Assessment. 2006;18(4):373–381. doi: 10.1037/1040-3590.18.4.373. [DOI] [PubMed] [Google Scholar]
- Espy KA, Cwik MF. The development of a trail-making test in young children: The TRAILS-P. Clinical Neuropsychology. 2004;18:1–2. doi: 10.1080/138540409052416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdinand RF, Hoogerheide KN, van der Ende J, Visser JH, Koot HM, Kasius MC, Verhulst FC. The role of the clinician: Three-year predictive value of parents', teachers', and clinicians' judgment of childhood psychopathology. Journal of Child Psychology and Psychiatry. 2003;44(6):867–876. doi: 10.1111/1469-7610.00171. [DOI] [PubMed] [Google Scholar]
- Foster EM, Jones DE the Conduct Problems Prevention Research Group. The high costs of aggression: Public expenditures resulting from Conduct Disorder. American Journal of Public Health. 2005;95(10):1767–1772. doi: 10.2105/AJPH.2004.061424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garon N, Bryson SE, Smith IM. Executive function in preschoolers: A review using an integrative framework. Psychological Bulletin. 2008;134(1):31–60. doi: 10.1037/0033-2909.134.1.31. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Reilly J, Lemery KS, Longley S, Prescott A. The laboratory temperament assessment battery: Preschool version. Madison: University of Wisconsin; 1999. [Google Scholar]
- Greven CU, Asherson P, Rijsdijk FV, Plomin R. A longitudinal twin study on the association between inattentive and hyperactive-impulsivity ADHD symptoms. Journal of Abnormal Child Psychology. 2011;39:623–632. doi: 10.1007/s10802-011-9513-7. [DOI] [PubMed] [Google Scholar]
- Isquith PK, Crawford JS, Espy KA, Gioia GA. Assessment of executive function in preschool-aged children. Mental Retardation and Developmental Disabilities. 2005;11:209–215. doi: 10.1002/mrdd.20075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Wakschlag LS. Can a valid diagnosis of disruptive behavior disorder be made in preschool children? The American Journal of Psychiatry. 2002;159(3):351–358. doi: 10.1176/appi.ajp.159.3.351. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Barry RA, Jimenez NB, Hollatz AL, Woodard J. Guilt and effortful control: Two mechanisms that prevent disruptive developmental trajectories. Journal of Personality and Social Psychology. 2009;97(2):322–333. doi: 10.1037/a0015471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, Murray KT, Harlan ET. Effortful control in early childhood: Continuity and change, antecedents, and implications for social development. Developmental Psychology. 2000;36(2):220–232. [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111(3):411–424. [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Gibbons RD, Christoffel KK, Arend R, Rosenbaum D, Binns H, et al. Isaacs C. Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(2):204–214. doi: 10.1097/00004583-199602000-00014. [DOI] [PubMed] [Google Scholar]
- Leblanc N, Boivin M, Dionne G, Brendgen M, Vitaro F, Tremblay RE, et al. Perusse D. The development of hyperactive-impulsive behaviors during the preschool years: The predictive validity of parental assessments. Journal of Abnormal Child Psychology. 2008;36:977–987. doi: 10.1007/s10802-008-9227-7. [DOI] [PubMed] [Google Scholar]
- Liebermann D, Giesbracht GF, Muller U. Cognitive and emotional aspects of self-regulation in preschoolers. Cognitive Development. 2007;22:511–529. [Google Scholar]
- Marcus DK, Barry TD. Does attention-deficit/hyperactivity disorder have a dimensional latent structure: A taxometric analysis. Journal of Abnormal Psychology. 2011;120(2):427–442. doi: 10.1037/a0021405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM. A new perspective on attention-deficit/hyperactivity disorder: Emotion dysregulation and trait models. Journal of Child Psychology & Psychiatry. 2009;50(9):1042–1051. doi: 10.1111/j.1469-7610.2009.02105.x. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nigg JT. Child ADHD and personality/temperament traits of reactive and effortful control, resiliency, and emotionality. Journal of Child Psychology and Psychiatry. 2006;47(11):1175–1183. doi: 10.1111/j.1469-7610.2006.01629.x. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nigg JT, von Eye A. How do trait dimensions map onto ADHD symptom domains? Journal of Abnormal Child Psychology. 2009;37:337–348. doi: 10.1007/s10802-008-9255-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCartney K, Burchinal MR, Bub KL. Best practices in quantitative methods for developmentalists. In: Overton WF, Berry M, editors. Monographs of the Society for Research in Child Development. Boston, MA: Blackwell Publishing; 2006. pp. 1–145. [DOI] [PubMed] [Google Scholar]
- McDonald RP, Ho MR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7(1):64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cognitive Psychology. 2000;41:49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- Murphy KT, Kochanska G. Effortful control: Factor structure and relation to externalizing and internalizing behaviors. Journal of Abnormal Child Psychology. 2002;30(5):503–514. doi: 10.1023/a:1019821031523. [DOI] [PubMed] [Google Scholar]
- Múthen LK, Múthen BO. MPlus user's guide. 4th. Los Angeles, CA: Múthen & Múthen; 1998–2007. [Google Scholar]
- Nigg JT. On inhibition/disinhibition in developmental psychopathology: Views from cognitive and personality psychology and a working inhibition taxonomy. Psychological Bulletin. 2000;126(2):220–246. doi: 10.1037/0033-2909.126.2.220. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Casey BJ. An integrative theory of attention-deficit/hyperactivity disorder based on the cognitive and affective neurosciences. Development & Psychopathology. 2005;17(3):785–806. doi: 10.1017/S0954579405050376. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Foster M, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Ambulatory Pediatrics. 2007;7(1S):121–131. doi: 10.1016/j.ambp.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Jr, Fabiano GA, Massetti GM. Evidence based assessment of attention-deficit/hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):449–476. doi: 10.1207/s15374424jccp3403_5. [DOI] [PubMed] [Google Scholar]
- Pelletier J, Collett B, Gimple G, Cowley S. Assessment of disruptive behaviors in preschoolers: Psychometric properties of the Disruptive Behavior Disorders Rating Scale and School Situations Questionnaire. Journal of Psychoeducational Assessment. 2006;24(1):3–18. [Google Scholar]
- Pennington BF, Ozonoff S. Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry. 1996;37(1):51–87. doi: 10.1111/j.1469-7610.1996.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Putnam SP, Rothbart MK. Development of short and very short forms of the Children's Behavior Questionnaire. Journal of Personality Assessment. 2006;87(1):103–113. doi: 10.1207/s15327752jpa8701_09. [DOI] [PubMed] [Google Scholar]
- Raykov T. Estimation of composite reliability for congeneric measures. Applied Psychological Measurement. 1997;21(2):173–184. [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, Fisher P. Investigations of temperament at three to seven years: The Children's Behavior Questionnaire. Child Development. 2001;72(5):1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- Rueda MR, Posner MI, Rothbart MK. The development of executive attention: Contributions to the emergence of self-regulation. Developmental Neuropsychology. 2005;28(2):573–594. doi: 10.1207/s15326942dn2802_2. [DOI] [PubMed] [Google Scholar]
- Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, et al. Rapoport JL. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proceedings of the National Academy of Sciences. 2007;104(49):19649–19654. doi: 10.1073/pnas.0707741104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. The dual pathway model of AD/HD: An elaboration of neuro-developmental characteristics. Neuroscience and Biobehavioral Reviews. 2003;27:593–604. doi: 10.1016/j.neubiorev.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Maughan B, Goodman R. What's in a disruptive disorder? Temperamental antecedents of Oppositional-Defiant Disorder: Findings from the Avon Longitudinal Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(5):474–483. doi: 10.1097/00004583-201005000-00008. [DOI] [PubMed] [Google Scholar]
- Task Force on Research Diagnostic Criteria: Infancy and Preschool. Research diagnostic criteria for infants and preschool children: The process and empirical support. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(12):1504–1512. doi: 10.1097/01.chi.0000091504.46853.0a. [DOI] [PubMed] [Google Scholar]
- Thorell LB, Wahlstedt C. Executive functioning deficits in relation to symptoms of ADHD and/or ODD in preschool children. Infant and Child Development. 2006;15:503–518. [Google Scholar]
- Willcutt EG, Doyle AE, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry. 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]


